since 05.January 2015
ORIGINAL ARTICLES
[Full article in HTML], [PDF], [XML]
……………………………………………………………………………………………………
Even Hyppocrates from Cos, prime founder of the Art of the Science of Medicine (or perhaps of the Science of the Art of Medicine) used to refer that „OCULUS SALUTIS SPECULUM”, and I have to confess that throughout all my experience I have noticed that psoriatic individuals present always eye malaises, even the simplest yellowish cornea, which reflects a status of bilirubin disarray; I have often suggested to instill eye drops made with Great Plantain mother tincture (Plantago Major Linné) plus white copperas (Zincum sulphuricum) in the eyes of psoriatic patient. Lorenzo Martini, M.Sc. (Italy)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… I, congratulate Zonunsanga for taking pain in conducting this trial. This research under taken by Zonunsanga et al is a step forward in the field of targeted phototherapy showing efficacy of excimer light therapy in the treatment of alopecia areata; opening a field of further research before this modality is offered / recommended as a good therapeutic option for AA. From the present evidence available corticosteroids being the most popular and minoxidil being the least preferred treatment in the management of AA. The same conclusions have been documented in this study also. Addition of certain criteria in results section [ like Salt scoring tool, AGS six point scale, statistical analysis between the groups, flow diagram of the intervention, discussion of adverse effects in all the groups, relapse/ failure during follow-up period, age criteria in material and methods, maximum and minimum doses used in the excimer and steroid group] of this article would have made this article more comprehensive and elaborate. Dr Rakesh Tilak Raj (India) Excimer laser has been regarded by some authors as a ‘‘super-narrowband’’ UVB light source which is postulated to induce T cell apoptosis. The role of T cell in the pathogenesis of alopecia areata has been proposed to play a crucial role in the developing of this entity [1]. The present study shows how excimer laser can be a safe and effective option in our therapeutic armamentum when treating this disease. References: 1. McMichael AJ. Excimer laser: a module of the alopecia areata common protocol. J Investig Dermatol Symp Proc. J Investig Dermatol Symp Proc. 2013;16:S77-9. Dr Manuel Valdebran (República Dominicana)
BRIEF REPORTS
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… This is a valuable study because of importance that pure neural leprosy, a rare form of leprosy, is mostly seen in India with a percentage of %18. Assesment of relationship between bacillary load and neuritis in an endemic region makes results more reliable. Dr Seval Boyraz Karasat (Turkey)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… It is utterly reliable that the usage of an „escariotic” as salicylic acid 30% hydrogel is useful to struggle scars after a drastic peeling of acneic skin performed by the aids of high dosages of glycolic acid. It is the insistence of the application of a physical „escariotic” that yields to the complete restitutio ad integrum, in my view. The oral administration of vitamin C during the treatment is appreciable and really praiseworthy! Lorenzo Martini, M.Sc. (Italy) The author deserves appreciation for his deep insight in using Chemical peel and micro needling in the treatment of acne scarring. Dermatologists should mind complications like pigmentary changes, infection and prolonged erythema after procedure, and contraindications like active bacterial, viral, fungal, or herpetic infection, Open wounds, history of photosensitizing drugs, pre-existing inflammatory dermatoses (e.g., psoriasis, atopic dermatitis),Uncooperative patient (patient is careless about sun exposure or application of medicine), Patient with unrealistic expectations. Dr. Yugandar Inaks (India) Authors have published a manuscript about one of the most challenging issue in Dermatology: Acne scarring. As I always state on my daily practice, the best treatment for acne scars is the prevention since once the management of this condition is quite difficult. Since my experience on managing acne scars with topical acid is unsatisfactory, the regime used by authors is attractive, compelling, and easy to perform. Therefore, it is likely to implement this therapy on my outpatient daily practice. Even with reduced sample size, like the one from this study, more researches on this way are needed for setting new hypothesis and thus, more promising and effective therapies. Dr. Husein Husein-ElAhmed (Spain)
[Full article in HTML], [PDF], [XML]
CASE REPORTS
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… We congratulate Dobrev and Nocheva [1] for their excellent depiction on the use of videodermatoscopy (VD) on pearly penile papules. We entirely agree that VD and its static counterparts non-digital (ED) and digital epiluminescence dermoscopy/dermatoscopy (DED) are highly effective in substantiating the diagnoses of many non-pigmented cutaneous conditions. We strived to share our experience to echo the findings of Dobrev and Nocheva, and inserted a review of the underlying biophysical principles. For the use of dermatoscopy in pearly penile papules, we were actually the first in reporting such [2]. However, this previous article was focused on sexually transmitted infections, and the terms dermoscopy or dermatoscopy are not listed in the title or abstract in Medline or other indexes. We have found that DED can be helpful in diagnosing pityriasis rosea, through magnification of the lesions and the elimination of other epidermal details such as skin creases and excoriation [3,4]. For pediculosis pubis, VD could identify the nits and moving lice [5]. As the imaging was performed in real time projection on the computer monitor, the experience was thrilling for the patient, who subsequently modified his sexual behaviour desirably. For pseudofolliculitis barbae, we depicted inverted-U-shaped ingrowing hairs through DED [6]. Upon providing the patient with solid proof that the over-enthusiastic use of triple-bladed razors did lead to ingrown hairs, pseudofolliculitis, and subsequent hypertrophic scars, we achieved therapeutic success by behavioural modifications alone. Lastly, for focal vitiligo, DED revealed the sparing of perifollicular pigments while the interfollicular pigments were destroyed by the autoimmunity at the border of the lesions [7]. This pattern is pathognomonic for all types of urticaria, and VD and DED should play tremendous roles in reaching a definite diagnosis particularly for patients with marginal findings on examination with bare eyes or with magnifying lens. A number of trainees have indicated to us that they do not understand the underlying biophysical principles of ED, DED, and VD. We thus take the liberty to cover such briefly here. These devices incorporate two filters at 90° to each other, one for light emitting from and the other for light returning to the scope. The emitting light passes through the first filter, and becomes polarised. Some of the polarised light is reflected from the skin surface. As only one reflection occurs, the returning light is still polarised, and is blocked by the second filter. Some of the polarised light passes through the skin surface to lower layers of the epidermis and superficial dermis. Through repeated refractions, the returning light becomes non-polarised, and is not blocked by the second filter. The viewer thus sees the light from deeper layers of the epidermis and upper dermis only, which is free from details of the skin surface such as skin creases and excoriations. We congratulate Dobrev and Nocheva again for their outstanding article with VD images of unsurpassed quality, and look forward to seeing further reports broadening the utilisations of ED, DED and VD. References: 1. Dobrev HP, Nocheva DG. Videodermatoscopy of pearly penile papules – Case reports. Our Dermatol Online. 2014;5:29-31. 2. Chuh AAT, Wong WCW, Lee A. Ten common myths in sexually transmitted diseases. Aust Fam Physician. 2006;35:127-9. 3. Chuh AAT. Collarette scaling in pityriasis rosea demonstrated by digital epiluminescence dermatoscopy. Australas J Dermatol. 2001;42:288-90. 4. Chuh AAT. The use of digital epiluminescence dermatoscopy to identify peripheral scaling in pityriasis rosea. Comput Med Imaging Graph. 2002;26:129-34. 5. Chuh A, Lee A, Wong W, Ooi C, Zawar V. Diagnosis of pediculosis pubis – a novel application of digital epiluminescence dermatoscopy. J Eur Acad Dermatol Venereol. 2007;21:837-8. 6. Chuh A, Zawar V. Pseudofolliculitis barbae – epiluminescence dermatoscopy enhanced patient compliance and achieved treatment success. Australas J Dermatol. 2006;47:60-2. 7. Chuh AAT, Zawar V. Demonstration of residual perifollicular pigmentation in localized vitiligo – a reverse and novel application of digital epiluminescence dermoscopy. Comput Med Imaging Graph. 2004;28:213-7. Ass. Prof. Antonio Chuh (Hong Kong) and Prof. Vijay Zawar (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… A very interesting case report. Thanks to authors. Epidermodysplasia verruciformis (EV) is a rare genodermatosis, first described by Lewandosky and Lutz in 1922 [1]. This premalignant lesion has occurred de novo, as well as in patients with impaired cell-mediated immunity, including those infected with HIV, systemic lupus erythematosus [2], or lymphoma [3], or those who have received a solid organ transplant [4]. In immunocompromised and immunocompetent populations, typical clinical findings are similar, and include pityriasis versicolor-like macules, as well as flat papules and lesions resembling verruca plana. Characteristic histologic features of the disease are the coexistence of epidermal thickening, a loose horny layer with a basketweave–like appearance, and the presence of large cells in the spinous and granular layers of the skin, presenting with a large blue-gray cytoplasm often associated with a perinuclear halo [5]. References: 1. Lewandowsky F, Lutz W. Archives of dermatology and syphilology. Berlin: 1922:141(193). 2. Tanigaki T, Kanda R, Sato K. Epidermodysplasia verruciformis (L-L, 1922) in apatient with systemic lupus erythematosus. Arch Dermatol Res. 1986;278:247-8. 3. Barr BB, Benton EC, McLaren K, Bunney MH, Smith IW, Blessing K, et al. Papillomavirus infection and skin cancer in renal allograft recipients. Lancet. 1989;2:224-5. 4. Gross G, Ellinger K, Roussaki A, Fuchs PG, Peter HH, Pfister H. Epidermodysplasia verruciformis in a patient with Hodgkin’s disease: characterization of a new papillomavirus type and interferon treatment. J Invest Dermatol. 1988;91:43-8. 5. Majewski S, Jablonska S. Epidermodysplasia verruciformis as a model of human papillomavirus-induced genetic cancer of the skin. Arch Dermatol. 1995;131:1312-8. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… The authors describe an interesting case report of Tinea faciei highlighting the practical aspects in daily activity. Adequately written, very well documented and updated the article focuses on what is known and what is new in a clinical problem frequently seen by dermatologists. It is an educative paper, well illustrated and presented. Prof. Anca Chiriac (Romania) Thanks to authors for posting rare case report. Dermatophytoses are the most common fungal infections of the skin. In the clinical practise, tinea pedis is most common clinical form of dermatophytosis. Other clinical forms are tinea cruris, tinea capitis, tinea corporis and tinea faciei. Tinea faciei is a rare form of dermatophytosis of glabrous skin, characterized by a well- circumscribed erythematous patch, and is more commonly misdiagnosed with some dermatologic diseases as seborrheic dermatitis, contact dermatitis, polymorphic light eruption and lymphocytic infiltrations. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks to author for posting an interesting case report. Cheilitis is a general term that refers to an inflammation of the vermilion border of the lips. Cheilitis is classified into various types: angular cheilitis, actinic cheilitis, contact cheilitis, plasma cell cheilitis, cheilitis glandularis, cheilitis granulomatosa, exfoliative cheilitis and factitious chelitis. Exfoliative cheilitis, a rare, localized condition, is a chronic superficial inflammatory condition that is characterized by regular peeling of a superficial excessive layer of keratin. In most cases, a good history, thorough clinical examination and relevant investigations will help the clinician arrive at a diagnosis. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks for presenting these case report. Lupus miliaris disseminatus faciei (LMDF) is a benign condition characterized by a papular eruption located in the central face. Histologic studies of the papules show granulomatous infiltrates with central necrosis. The condition is self-limited and usually resolves within 1 to 2 years yet can be cosmetically debilitating, given the location and potential for scarring. Dr. Yugandar Inaks (India) This case corresponds to the facial granulomatous dermatosis, a group of disorders characterized by facial papules with the common histological feature of epithelioid granulomas. LMDF is a a diagnosis supported by the poor response to tetracyclines and the good response to steroids, in addition to the signs of rosacea (facial redness) that she presented during the course of the disease. All this lead in the presente time to consider LMDF, granulomatous rosacea, perioral granulomatous dermatitis, and the nodular cutaneous form of sarcoidosis to be in the same diagnostic category, the facial granulomatous dermatoses. Prof. Beatriz Di Martino Ortiz (Paraguay)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks to authors for presenting rare disease. Moniletherix is a rare hereditary condition with variable expressivity characterized by the presence of beaded or spindle-shaped shafts of scalp hair.It is usually inherited as an autosomal-dominant trait but rarely can be autosomal-recessive. It shows considerable variations in age of onset, severity, and course. Hair is usually normal at birth and is progressively replaced by abnormal hair during first few months of life. Dr. Yugandar Inaks (India) This is yet another case report of monilethrix. It is of interest to note that in this case it is associated with Keratotic horny papules on the nape of the neck. Had skin biopsy been taken from that site it would have keratosis pilaris. Though topical minoxidil 2% will be useful, we cannot predict the growth of hairs with similar monilethrix features on other unwanted areas like cheeks, chin and arms at a younger age which will not be welcome. It required lot of research to decipher the genetic mutations in affected families. Congratulations to the authors for the nice presentation. Prof. Sundaramoorthy Srinivasan (India) The article is very comprehensive and accurate. Monilethrix is a picture of hypotrichosis of childhood. The differential diagnosis should consider: woolly hair, ectodermal dysplasia, Hereditary hypotrichosis simplex of the scalp, Marie Unna hypotrichosis, generalized hypotrichosis simplex, among others. Dra. María Bibiana Leroux (Argentina)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Localized scleroderma causes one or more patches of hard skin. There are different types. The linear type can cause problems to underlying tissues such as muscles and bones. En coup de sabre or morphea en coup de sabre is a type of linear scleroderma characterized by a linear band of atrophy and a furrow in the skin that occurs in the frontal or fronto-parietal scalp. Only few cases have been documented in literature related to late onset variety. For ex. 1. Yamanaka CT, Gibbs NF. Trauma-induced linear scleroderma. Cutis. 1999;63:29–32; 2. Mohan SV, Nittur V, Stevens KJ. Late-onset en coup de sabre of the skull.Skeletal Radiol. 2013;42:1447-50. This phenomenon can be categorized as a recently introduced Post traumatic isotopic response: (the occurrence of a new skin disease at the site of previous trauma). Please refer- Proposed classification for koebner, wolf isotopic, renbok, koebner nonreaction, isotopic nonreaction & other related phenomen. Kannangara, Ajith P; Yosipovitch, Gil; Fleischer Jr., Alan B. Dermatology Online Journal, 20(11) November 16, 2014. According to our experience for severe form of disease oral mini pulse steroids or methotrexate and topical Calcipotriol and Tacrolimus ointment would be the most suitable treatment for early cases. Dr Ajith Prasanna Kannangara (Sri Lanka)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… An Interesting case report with peerless association. Thanks to authors. Ledderhose disease is a relatively rare foot disorder of unknown etiology. Although it is listed as a “rare disease” by the Office of Rare Diseases (ORD). It is characterized by local proliferation of abnormal fibrosis tissue in the plantar fascia. The nodules are typically slow growing and most often found in the central and medial portions of the plantar fascia. This tissue is locally aggressive and progressively replaces the normal plantar aponeurosis. LD may occur at any age with the greatest prevalence at middle age and beyond. This disorder is more common in men than woman and it is sometimes associated with other forms of fibromatosis, such as Dupuytren’s disease in the hand, Peyronie’s disease, or knuckle pads. Only 25 percent of patients have bilateral involvement. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks to Author for an interesting case report. Cervical cancer rarely metastasizes to the skin; this occurs in less than 2% of patients.2–5 Patients with cutaneous metastatic disease may present at the time of diagnosis or up to 10 years later [1-3]. The presence of metastatic disease in the skin signals a poor prognosis, because skin metastasis is usually associated with local or regional recurrence [2,4]. The treatment is usually palliative [1,4]. The mechanism of metastasis can be understood as a series of steps providing three basic patterns of distribution: 1) mechanical (arising from anatomical proximity and lymphatic draining), 2) site-specific (arising from the selective attachment of tumour cells to a specific organ), 3) non-selective (independent of these distribution factors) [4]. The proposed mechanism of cutaneous metastasis is radiationinduced endothelial cell damage, leading to tumour cell trapping [5,6]. It is usually confined to the irradiation fields, appearing months to years after treatment completion [5]. Another probable mechanism described is alteration of the lymphatic flow by tumour [2]. In most cases, it probably results from the obstruction of deep lymphatic pathways by tumour with shunting of the lymphatic flow to the cutaneous lymphatics [2,3]. References: 1. Malfetano JH. Skin metastasis from cervical carcinoma: a fatal event. Gynecol Onco.l 1986;24:177–82. 2. Tharakaram S, Rajendran SS, Premalatha S, Yesudian P, Zahara A. Cutaneous metastasis from carcinoma cervix. Int J Dermatol. 1985;24:598–9. 3. Freeman CR, Rozenfeld M, Schopflacher P. Cutaneous metastases from carcinoma of the cervix. Arch Dermatol. 1982;118:40–1. 4. Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol. 1995;33:161–82. 5. Diehl LF, Hurwitz MA, Johnson SA, Butler WM, Taylor HG. Skin metastases confined to a field of previous irradiation; report of two cases and review of the literature. Cancer. 1984;53:1864–8. 6. Yamamoto T, Ohkubo H, Nishioka K. Cutaneous metastases from carcinoma of the cervix resemble acquired lymphongioma. J Am Acad Dermatol. 1994;30:1031–2. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks to authors for nice brief report. Mycosis fungoides (MF), a low-grade lymphoproliferative disorder, is the most common type of cutaneous T-cell lymphoma. Typically, neoplastic T cells localize to the skin and produce patches, plaques, tumours or erythroderma. Diagnosis of MF can be difficult due to highly variable presentations and the sometimes nonspecific nature of histological findings. Molecular biology has improved the diagnostic accuracy. So Mycosis Fungoides is a Dermatological Masquerader. Table shows differential diagnosis of mycosis fungoides [1-3]. References: 1. Kikuchi A, Shimizu H, Nishikawa T. Mycosis fungoides with marked hyperpigmentation. Dermatology. 1996;192:360–3. 2. Co´rdoba S, Ferna´ndez-Herrera J, Sa´nchez-Perez J, Fraga J, García-Díez A. Vesiculobullous mycosis fungoides. Br J Dermatol. 1999;141:164–5. 3. Kodama K, Fink-Puches R, Massone C, Kerl H, Cerroni L. Papular mycosis fungoides: a new clinical variant of early mycosis fungoides. J Am Acad Dermatol. 2005;52:694–8. Dr. Yugandar Inaks (India) This very interesting article highlights the skin as mirror to internal disease. In every dermatologist, there should be something of the detective. Keen observation, intense inspection of the subject, attention to details and apparent trifles are particularly pertinent to dermatologist. Recent overenphasis of dermatology on cosmiatric subjects may lead to lack of interest on investigative aspects. In fact, lucrative aspects of cosmiatric procedures is the prime suspect of this new behavior that leads dermatology to dangerous directions. Various systemic illnesses manifest in the skin and skin offers the advantage of easy access for biopsy. This case also stresses the importance of close inspection with ” eye of eagle ” – as the authors wisely quote – of every otherwise unimportant lesions and subsequent biopsy for that skin lesions often represent just the tip of the iceberg. The precoce diagnosis can be of substantial benefit to the patients avoiding progression of many diseases. Dr César Bimbi (Brasil)
REVIEW ARTICLES
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Congratulations to Author. An interesting up-to-date review of Hepatitis B virus association with dermatological changes. By improving awareness about screening among dermatologists regarding the risks of HBV reactivation and its prevention for patients receiving following drugs seems warranted. 1) Interleukin receptor antagonists: Ustekinumab, anakinra, tocilizumab. 2) Tumor necrosis factor (TNF) inhibitors: Infliximab, etanercept, adalimumab. 3) Antineoplastic agents: methotrexate. 4) Glucocorticoids, follow abrupt discontinuation. 5) Anti-CD20 antibodies: Ofatumumab, rituximab. Dr. Yugandar Inaks (India)
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… A very interesting -up to date- review of alopecia areata treatment. Alopecia areata is highly unpredictable; no treatment is effective in preventing or halting progression of the condition. Many professional consider the treatment of most alopecia areata is not mandatory, as the condition is benign, and spontaneous remissions and recurrences are common. Although medically benign, alopecia areata can cause tremendous emotional and psychosocial distress in affected patients and their families. This is a good comprehensive review of available treatments for alopecia areata. Furthermore, we need always to remember that patient education is a key factor in alopecia areata; inform patients that expectations regarding therapy should be realistic. Other options as the use of hairpieces or take part in support groups should be considered in the management because they are of great benefit. Dr Amani Tresh (Libya) This is a very interesting article of common topic in clinical dermatology. Under the classification of alopecia areata I would like to propose the 7th sub variety as- alopecia areata co-localization with other auto immune disease such as vitiligo and lichen planus. Both alopecia areata and vitiligo are common skin disorders that are considered to be caused by an autoimmune response targeted to hair follicle and melanocyte antigens, respectively. The association of these two diseases in the same patient is well known, however, coexistence of alopecia areata and vitiligo within the same lesion is very rare. For eg. 1. Ozcan D, Cevlik Aydo?an F. Concurrence of alopecia areata and vitiligo at the same anatomical site. Australas J Dermatol. 2012;53:61-3; 2. Yadav S, Dogra S, Kaur I. An unusual anatomical colocalization of alopecia areata and vitiligo in a child, and improvement during treatment with topical prostaglandin E2. Clin Exp Dermatol. 2009;34:1010-1; 3. Dhar S, Dhar S. Colocalization of alopecia areata and lichen planus. Pediatr Dermatol. 1996;13:258-9. This phenomenon can be categorized as a recently introduced, Isotopic co-response: (If the second skin disease appeared on the site of previous active disorder). Please refer- Proposed classification for koebner, wolf isotopic, renbok, koebner nonreaction, isotopic nonreaction & other related phenomen. Kannangara, Ajith P; Yosipovitch, Gil; Fleischer Jr., Alan B. Dermatology Online Journal, 20(11) November 16, 2014. Dr Ajith Prasanna Kannangara (Sri Lanka)
CLINICAL IMAGES
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thank you Dr. Patricia for your nice presentation. Having a good experience with Cutaneous Leishmaniasis, some few notes on the laboratory diagnosis I may add to the topic. In the study in the laboratory investigation performed a microscopic examination of the lesion with Giemsa stain, obtained by skin scraping, was negative and another biopsy for histologic examination was negative too. That is usually expected as falls negative in almost 50% of the positive cases diagnosed by the smear method looking particularly for the LD bodies ( the amastigote forms within the macrophage ) as the principle of the Leishman-Donovan method to detect the disease. Recent discoveries in the field revealed the existence of not only the amastigote form within the macrophage but the promastigote form as well within the smear of the infected skin scraping. The promastigote from usually exists in the extracellular fluid of the infected tissues and could be easily localized in the stained smear by an experienced technician. (See 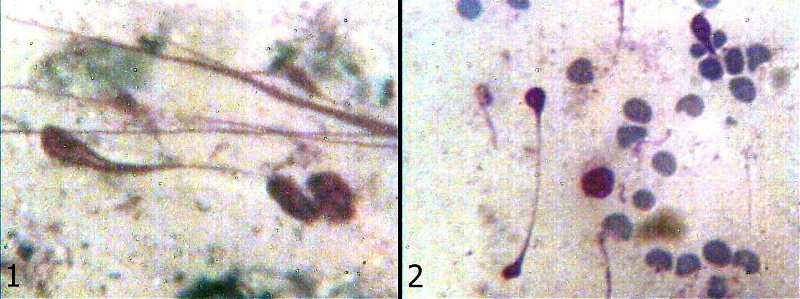 ). Having said so, the investigation of the promastigote existence by the skin scrap through the conventional smear method after staining with Giemsa or Wright stain will absolutely add much to the sensitivity and specificity of the smear method procedure reaching almost a 100%. This will allow a fast easy recognition of the disease diagnosis with limited non sophisticated measures and will facilitate the diagnosis in arias with restricted facilities. It may be of paramount importance to start applying the additional figures of the promastigote to the original smear procedure (Leishman-Donovan) method in order to achieve the best diagnosis from the method itself. For further information see the references: 1. Wael Daboul M. Promastigote existence in infected lesions of Cutaneous Leishmaniasis Journal of general Practice Review article. 2. Wael Daboul M. Cutaneous Leishmaniasis- A New Concept. Lap Lambert Academic Publishing 2012. 3. Wael Daboul M. Application of the microscopic method in cutaneous leishmania diagnosis. Our Dermatol Online. 2011;2:199-203. Dr. Mohamed Wael Daboul (Syrian Arab Republic)
). Having said so, the investigation of the promastigote existence by the skin scrap through the conventional smear method after staining with Giemsa or Wright stain will absolutely add much to the sensitivity and specificity of the smear method procedure reaching almost a 100%. This will allow a fast easy recognition of the disease diagnosis with limited non sophisticated measures and will facilitate the diagnosis in arias with restricted facilities. It may be of paramount importance to start applying the additional figures of the promastigote to the original smear procedure (Leishman-Donovan) method in order to achieve the best diagnosis from the method itself. For further information see the references: 1. Wael Daboul M. Promastigote existence in infected lesions of Cutaneous Leishmaniasis Journal of general Practice Review article. 2. Wael Daboul M. Cutaneous Leishmaniasis- A New Concept. Lap Lambert Academic Publishing 2012. 3. Wael Daboul M. Application of the microscopic method in cutaneous leishmania diagnosis. Our Dermatol Online. 2011;2:199-203. Dr. Mohamed Wael Daboul (Syrian Arab Republic)
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
LETTERS TO THE EDITOR – Observations
LETTER TO THE EDITOR
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… The authors show a curious case of tinea versicolor showing a follicutropic distribution. Certainly this type of presentation is not frequent. It would have been interesting to know if deeper sections were examined when reviewing the histopathological slides to exclude the possibility of a follicular involvement. I encourage the authors to do a prospective study to show the frequency, based on your demographics, of this interesting clinical presentation of tinea versicolor. Dr. Manuel Valdebran (Dominican Republic)
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
…………………………………………………………………………………………………… Thanks to Authors. In a short review, Author describes the chemical, physical, and mechanical properties of some skin suture materials. The choice of an appropriate suture for any wound closure will make a large contribution to the final functional and cosmetic result. The choice of suture material depends on the following: 1) Type and anatomic location of the wound. 2) Thickness of the skin. 3) Degree of tension. 4) Desired cosmetic result. Dr. Yugandar Inaks (India)
HISTORICAL ARTICLES
[Full article in HTML], [PDF], [XML]
[Full article in HTML], [PDF], [XML]
BOOK REVIEW
[Full article in HTML], [PDF], [XML]
Comments are closed.