Perforating metastatic melanoma
Takenobu Ohashi, Nobuyuki Kikuchi, Yuka Hanami, Takako Miura, Mikio Otsuka, Toshiyuki Yamamoto
Sir,
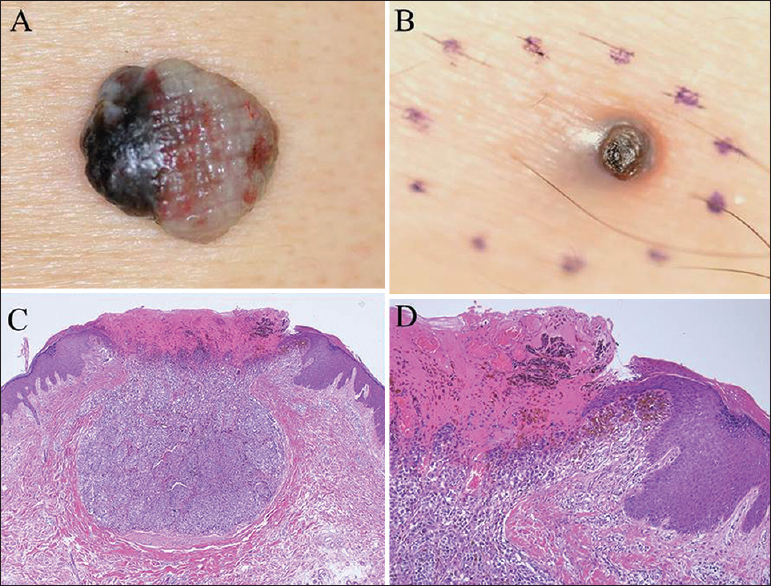
We describe a case of metastatic malignant melanoma on the thigh with comedo-like appearance, which histologically showed elimination of tumor cells.
A 70 year-old man was diagnosed with a nodular type malignant melanoma involving the lower back with satellite lesions (stage IIIB, T4b N2c M0, Breslow’s tumor thickness; 10.3 mm, Clark’s level; IV) (Fig. 1a). Sentinel lymph node evaluation was not performed. Three months after the excision of the primary melanoma with a 2-cm margin, skin metastasis appeared on his right inguinal region. Physical examination an additional month later revealed a firm, black-colored 5-mm sized nodule with crusts on the surface on the right thigh, with surrounding subcutaneous induration (Fig. 1b). Dermatoscopic examination found that keratins at the surface of the central lesion and a blue-white veil at the periphery. Histological examination of a totally removed nodule showed a small, symmetric and well-circumscribed lesion composed of nests of numerous atypical melanocytes in the dermis (Fig. 1c). Those atypical cells were positively stained with Melan-A, HMB45 and S-100. Tumor cells were located in abutment with and also within the epidermis. Nests of atypical melanocytes were confined to the crusts and perforated the skin surface (Fig. 1d). Treatment with chemotherapy was not implemented because the patient refused aggressive treatments. Six months after the onset of skin metastasis, he died of respiratory failure.
The patient’s informed consent was obtained.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
The most interesting feature in this case is the elimination of metastatic skin tumor masses through the epidermis. An epidermotropic growth pattern is an uncommon feature in malignant skin neoplasms, and tumor cell invasion in the epidermis is extremely rare in cutaneous metastatic tumors [1]. In our case, metastatic tumor cells were located in abutment with and also within the epidermis, which may lead to the clinical manifestations of superficial ulceration and crusts. The mechanism of epidermotropism in cutaneous metastasis still remains unknown; however, affinity of tumor cells with keratinocytes is speculated, possibly via adhesion molecules. Alternatively, epidermotropism in cutaneous metastases may be related to transepidermal elimination. Transepidermal elimination is a mechanism whereby foreign or altered constituents can be removed from the dermis through a channel that facilitates extrusion without gross disturbance of epidermal integrity. Transepidermal elimination of malignant tumor cells has been reported in the primary lesions of malignant melanoma [2,3]. By contrast, in our case we could not find any indication of elimination of tumor cells through the epidermis in the primary lesion. The presence of tumor cells in abutment with the epidermis, or infiltration of tumor cells into the epidermis, may trigger transepidermal elimination of tumor cells. In a strict meaning, our case did not show transepidermal elimination, and thus we prefer to use the term of perforating melanoma.
CONSENT
The examination of patient is conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. Saeed S, Keehn CA, Morgan MB, Cutaneous metastasis: A clinical, pathological, and immunohistochemical appraisalJ Cutan Pathol 2004; 31: 419-30.
2. Goette DK, Transepithelial elimination in malignant melanomaJ Assoc Milit Dermatol 1980; 6: 9.
3. Gartmann H, Transepidermal elimination of nevus and melanoma cellsHauzart 1982; 33: 495-7.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.