A retrospective study of profile of leprosy patients in a District Hospital in North India
Neerja Puri, Manjinder Kaur
Department of Dermatology and Venereology, Punjab Health Systems Corporation, Ferozepur, Punjab, India
ABSTRACT
Introduction: There is a high prevalence of leprosy in certain areas of our country. The main problem with leprosy is the prevalence of disability in untreated patients. Aims: To know the clinical profile of leprosy patients and to find out the risk factors for disabilities. Methods: A retrospective study of 10 years was conducted from April 2003 to March 2014 was conduced. Results:There were 137 MB (75.6%) and 44 PB (24.4%) cases. There were 35 (19.33%) MB patients with disability and 5 (2.76%) PB patients with disability. There were 5 cases (2.7%) with childhood leprosy. The percentage of defaulters was 9 (4.97%). The Patients were grade II disability were 19.4% and patients with grade I disability were 2.8%. Regarding the nerve involvement in leprosy, ulnar nerve was most commonly involved in 45 (24.86%) patients, lateral popliteal nerve in 20 (11.04%) patients, posterior tibial nerve in 15 (8.28%) patients and median nerve was involved in 12 (6.62%) patients. Conclusions:The multibacillary patients are more susceptible to neuritis as compared to the paucibacillary patients. The occurence of neuritis is a significant risk factor for disabilities in leprosy. Early diagnosis and treatment is important to reduce the load of infection.
Key words: Disability; prevalence; leprosy; grading; treatment; peripheral nerves; thickened
INTRODUCTION
Leprosy is a chronic infectious disease caused by mycobacteriae leprae. India has achieved elimination of leprosy with a national prevalence below 1/10,000. But due to lack of awareness about early diagnosis and treatment, there are many cases of disability still prevailing [1,2].
AIMS
- To know the clinical profile of leprosy patients
- To find out the patients with grade II disability
- To find out the risk factors for disabilities
- To find out the cases of childhood leprosy.
MATERIAL AND METHODS
A retrospective study of 10 years was conducted from April 2003 to March 2014 was conduced. The record of the patients was taken from the registers maintained. The registers had all the details about the dermatoneurological examination and WHO grading of disability. According to the WHO grading of disability: Grade 0- No disability due to leprosy; Grade I- Sensory impairment only; Grade II- Motor dysfunction and sequelae due to leprosy. All the thickened peripheral nerves were noted. The photographic record of the patients was also retrieved. The data including the age and sex of the patients, clinical profile and disability grading was tabulated and the data was analyzed statistically using chi square test.
RESULTS
The mean age of the patients was 25.85 years (Table 1). There were 139 (77.2%) males and 42 (18.9%) females. The male:female ratio was 3.3:1. There were 137 MB (75.6%) and 44 PB (24.4%) cases. There were 35 (19.33%) MB patients with disability (Fig. 1) and 5 (2.76%) PB patients with disability (Table 2). There were 5 cases (2.7%) with childhood leprosy (Fig. 2). The percentage of defaulters was 9 (4.97%). The percentage of Punjabi patients was 18.9% and non Punjabi patients was 81.7%. Patients were grade II disability (Fig. 3) were 19.4% and patients with grade I disability were 2.8%. Regarding the nerve involvement in leprosy, ulnar nerve was most commonly involved in 45 (24.86%) patients, lateral popliteal nerve in 20 (11.04%) patients, posterior tibial nerve in 15 (8.28%) patients and median nerve was involved in 12 (6.62%) patients (Table 3). A total of 11% patients had history of contact in the family and friends. The various risk factors for the development of disabilities were tabulated. Patients having multibacillary leprosy (75.69%) had high risk for development of deformities. Other risk factors for development of disability were: Old age (4.97%), patients with severe clinical disease (16.57%) and patients with neuritis (11.04%) (Table 4).
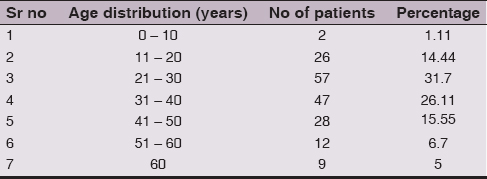

Figure 1: Claw hand in a 50 years old male
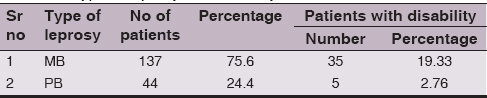
Table 2: Type of leprosy and disability

Figure 2: 12 years old child showing borderline tuberculoid leprosy

Figure 3: Facial deformity in a 78 years old male
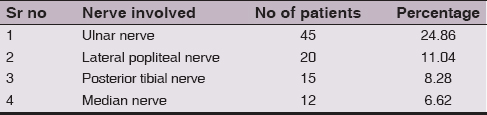
Table 3: Nerve involvement in leprosy
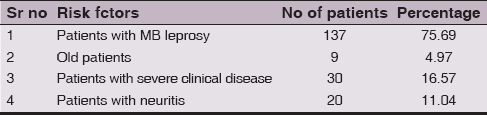
Table 4: Risk factors for disability in leprosy
DISCUSSION
The present study shows that more males were involved as compared to females which is not unusual as males have more exposure as compared to females who mostly stay indoors. It was also seen that multibacillary cases had higher chances of disability as compared to the paucibacillary cases (Fig. 4) as the patients with multibacillary leprosy required a long treatment and therefore some of the patients have poor compliance [3]. There were 2.7% cases of childhood leprosy in our study. With the decrease in the prevalence of leprosy in India, the number of childhood cases of leprosy have decreased significantly [4]. Contact tracing in leprosy is very important in leprosy and in our study 11% patients had history of contact in the family. India has achieved elimination of leprosy in 2005. Although elimination of leprosy has been achieved, still there are some high endemic zones in our country [5,6]. The main problem with leprosy is the development of impairments. The neurological sequelae are responsible for the stigma of leprosy as being a deforming disease.

Figure 4: Borderline tuberculoid leprosy in a 26 years old female
Leprosy is a chronic granulomatous disease which mainly involves skin and peripheral nerves [7,8]. According to the WHO classification, leprosy is divided into MB or multibacillary leprosy and PB or paucibacillary leprosy depending upon the number of lesions. Several factors have been associated with disabilities in leprosy [9,10]. The main risk factors associated with disability in leprosy are patients having multibacillary leprosy, delay in the diagnosis of leprosy, old age, the extent of clinical disease and the presence of neuropathy. All the high risk patients with disabilities must be carefully followed up to prevent any further impairments [11,12].
CONCLUSIONS
To conclude, the multibacillary patients are more susceptible to neuritis as compared to the paucibacillary patients. The occurence of neuritis is a significant risk factor for disabilities in leprosy. Also, there are many other multiple factors causing disability in leprosy. Also, timely diagnosis and treatment is an important factor for the prevention of neural function impairment in leprosy. Early diagnosis and treatment is important to reduce the load of infection.
CONSENT
The examination of the patient was conducted according to the declaration of Helsinki principles.
REFERENCES
1. Singhi MK, Ghiya BC, Gupta D, Kachhawa D, Disability rates in leprosyIndian J Dermatol Venereol Leprol 2004; 70: 314-6.
2. Pathak Thapa D, Kumar Jha A, Clinico – histopathological correlation in leprosy: a tertiary care hospital based studyOur Dermatol Online 2013; 4: 294-6.
3. Barbieri RR, Sales AM, Illarramendi X, Moraes MO, Nery JA, Moreira SJ, Diagnostic challenges of single plaque-like lesion paucibacillary leprosyMem Inst Oswaldo Cruz 2014; 109: 944-7.
4. Sachdeval S, Amin SS, Khan Z, Alam S, Sharma PK, Childhood Leprosy: A retrospective studyJ Public health Epidemiol 2010; 2: 267-71.
5. Peters RM, Dadun Van Brakel WH, Zweekhorst MB, Damayanti R, Bunders JF, The cultural validation of two scales to assess social stigma in leprosyPLoS Negl Trop Dis 2014; 8: e3274.
6. Freitas LR, Duarte EC, Garcia LP, Leprosy in Brazil and its association with characteristics of municipalities: ecological study 2009-2011Trop Med Int Health 2014; 19: 1216-25.
7. Yogeesh HR, Chankramath S, Yadalla HKK, Shariff S, Ramesh SB, Sreekantaiah SB, Type 2 lepra reactions (ENL) presenting with extensive cutaneous ulcerationsOur Dermatol Online 2012; 3: 17-20.
8. Scollard DM, Truman RW, Ebenezer GJ, Mechanisms of nerve injury in leprosyClin Dermatol 2015; 33: 46-54.
9. Kar HK, Gupta R, Treatment of leprosyClin Dermatol 2015; 33: 55-65.
10. Talhari C, Talhari S, Penna GO, Clinical aspects of leprosyClin Dermatol 2015; 33: 26-37.
11. Kar S, Pal R, Bharati DR, Understanding non-compliance with WHO-multidrug therapy among leprosy patients in Assam, IndiaJ Neurosci Rural Pract 2010; 1: 9-13.
12. Marcos LA, Conerly S, Walker S, LeprosyAm J Trop Med Hyg 2014; 91: 216.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.