Recurrent lupus miliaris disseminatus faciei: A case report
Zonunsanga, AK Khare Manisha, Poonam Saini
Department of Skin and VD, RNT Medical College, Udaipur, Rajasthan 313001, India
ABSTRACT
Lupus miliaris disseminatus faciei (LMDF) is a granulomatous eruption characterized by monomorphic, reddish-brown papules and nodules predominantly localized on the face. A 43 years old lady presented with multiple, painful, papulo-pustules over face 6 years back. Biopsy showed showed large foci of suppurative granulomatous dermatitis with a large central area of suppuration surrounded by histiocytes and occasional giant cells. Epidermis is not disrupted. Perifollicular and perivascular lymphocytic infiltrates were also seen. The lesions were healed with atrophic scars. She is now presented with multiple asymptomatic papules over bilateral periorbital regions of the face.
Key words: Lupus miliaris disseminatus faciei (LMDF), tuberculosis, rosacea, Demodex folliculorum
INTRODUCTION
Lupus miliaris disseminatus faciei (LMDF) is a granulomatous eruption characterized by monomorphic, reddish-brown papules and nodules predominantly localized on the face [1–3]. Earlier, it was thought to be a hypersensitivity reaction to tuberculosis, but a conclusive relationship to tuberculosis has not been established. Now a days, it is considered to be a variant of rosacea. Extrafacial manifestations can also be seen which may affect the axilla, shoulders, arms, hands, groins and leg. Tuberculin test and culture for Mycobacteria are usually negative [1–4]. Scarring is the primary complication. Recurrence is not common as far as our knowledge is concern after checking pubmeds and few dermatological journals. We hereby report a case of recurrent LMDF [2–5].
CASE REPORT
A 43 years old lady presented with multiple, painful, papulo-pustules over face 6 years back (Fig. 1 and 2). There was no history of cough, chest pain, hemoptysis, weight loss, fever, photosensitivity, flushing. Patient denied history of aggravation with spicy foods. She had undergone skin punch biopsy which showed large foci of suppurative granulomatous dermatitis with a large central area of suppuration surrounded by histiocytes and occasional giant cells. Epidermis is not disrupted. Perifollicular and perivascular lymphocytic infiltrates were also seen (Fig. 4). The features seems to be consistent with Lupus Miliasis Disseminatus faciei (LMDF). She was treated with Cap. Tetracyclines 500 mg QID, Tab. Dapsone 100mg OD and Fusidic acid ointment. Response to the treatment was seen after 3months of starting therapy. Due to slow response, patient was not satisfied and Tab. Azithromycin pulse (Azithromycin 500mg OD for 3 days followed, after Azithromycin off days for 10 days, by 3 days course of same dose of Azithromycin). was added to the treatment after 7 months. 1 month after Azithromycin pulse was started, the papulo-pustular lesions completely subsided and the patient left the treatment by herself. The lesions were healed with atrophic scars. There was no recurrence until November 2013, when she started developing multiple asymptomatic papules over bilateral periorbital regions of the face. The morphology and the distribution was more or less same as before except that it was in a less severe form. The photograph of the active phase of the second episode could not be taken as it was not so severe that she neglected as far as possible. Besides, she had some problem in transportation as she came from some far off village. By the time she came, only few lesions were present. However, he atrophic scars from previous episode were also present (Fig. 3). Unfortunately, she refused biopsy this time to confirm the recurrence. However, by clinically, It seems to be same as before and it is more or less proved to be recurrence.
The patient’s informed consent was obtained.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.

Figure 1: Periocular lesions of previous episode
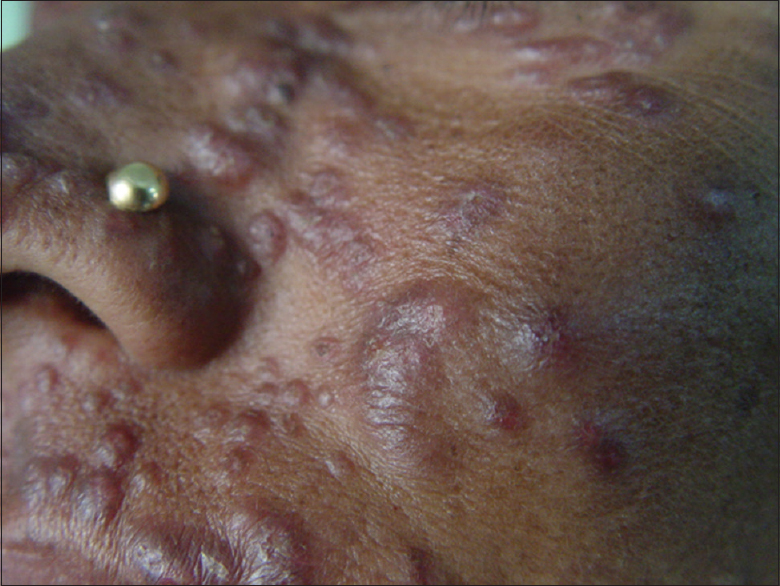
Figure 2: Perioral and cheeks of previous episode

Figure 3: Current episode (after healing)

Figure 4: Histopathology. Suppurative granulomatous dermatitis with a large central area of suppuration surrounded by histiocytes and occasional giant cells. Epidermis is not disrupted. Perifollicular and perivascular lymphocytic infiltrates
DISCUSSION
LMDF was first described in 1903 as an eruption consisting of groups of discrete dull red-brown papules tending to form pustules with spontaneous involution over several weeks, healing with scars [1–6]. It affects only skin [3–5]. Originally, LMDF was considered to be a variant of lupus vulgaris or a tuberculid, since the histological features show granulomatous-type inflammation and caseation necrosis [5–7]. However, there has been no evidence to date supporting a link with tuberculosis. Therefore, acne agminata and facial idiopathic granuloma with regressive evolution have replaced the term LMDF in some parts of the world [2–6]. Some authors suggested that LMDF is a reaction to Demodex folliculorum but the association has not been confirmed [5]. Others suggested that LMDF is a granulomatous reaction to hair follicle destruction or ruptured epidermal cyst [1–6]. The etiopathogenesis of LMDF is currently unknown. Originally, LMDF was thought to be a “tuberculid,” i.e., a condition related to tuberculosis because of its histopathologic features resembling this infection (epithelioid cell granuloma with central necrosis) [6–9]. However, bacteriological cultures from LMDF lesions failed to reveal bacilli and studies using the more sensitive polymerase chain reaction failed to detect Mycobacterium tuberculosis DNA. Therefore, the tuberculous origin of LMDF is no more accepted. Based on the fact that the granulomatous reaction frequently develops in the vicinity of a ruptured hair follicle, it has been hypothesized that LMDF is an expression of an immune response to the pilosebaceous units [5–9]. According to this hypothesis, damage to the hair-follicle epithelium (occurring in the early stage) releases follicular antigens that trigger an autoimmune reaction directed against hair-follicles [2–7]. Other authors consider LMDF to be a variant of granulomatous rosacea on the basis of the localization of the lesions in the midface and the pathological changes, which may be similar to those seen in granulomatous rosacea. However, several clinicopathological differences exist between rosacea and LMDF [4–8]. The former runs a more chronic course than LMDF. Extrafacial involement may occur in LMDF [8]. Patients do not report flushing and the disease is not worsened by alcohol or spicy food intake. Contrary to rosacea, LMDF lesions do not contain Demodex mites and they are more resistant to treatment and heal with scarring [5–7,10–12].
The treatment is unsatisfactory. The response to tetracyclines and retinoids (isotretinoin) is variable. Some repots of tetracyclines with isoniazide have been coming up. Some reports of effectiveness of dapsone are also seen [1,11,12]. Recently, Nonablative fractionated laser resurfacing and 1450-nm Diode Laser are reported to give promising results [13,14].
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. Rocas D, Kanitakis J, Lupus miliaris disseminatus faciei: Report of a new case and brief literature reviewDermatol Online J 2013; 19: 4.
2. Sanai M, Nadeem M, Aman S, Hasnain Kazmi A, Lupus miliaris disseminatus faciei: A case reportJ Pak Associat Dermatol 2013; 23: 232-5.
3. Moreira E, Lisboa C, Azevedo F, Lupus Miliaris Disseminatus Faciei – A case with preferential involvement of the penisTrab Soc Dermatol Venereol 2008; 66: 453-6.
4. Mullan E, Green P, Pasternak S, Lupus miliaris disseminatus faciei with extrafacial involvement in a 17-year-old white girlJ Cutan Med Surg 2011; 15: 340-3.
5. Esteves T, Faria A, Alves R, Marot J, Viana I, Vale E, Lupus miliaris disseminatus faciei: A case reportDermatol Online J 2010; 16: 10.
6. Van de Scheur MR, Van der Waal RI, Starink TM, Lupus miliaris disseminatus faciei: A distinctive rosacea-like syndrome and not a granulomatous form of rosaceaDermatology 2003; 206: 120-3.
7. Khokhar O, Khachemoune A, A case of granulomatous rosacea: Sorting granulomatous rosacea from other granulomatous diseases that affect the faceDermatol Online J 2004; 10: 6.
8. Hodak E, Trattner A, Feuerman H, Feinmesser M, Tsvieli R, Mitrani-Rosenbaum S, Lupus miliaris disseminatus faciei – the DNA of Mycobacterium tuberculosis is not detectable in active lesions by polymerase chain reactionBr J Dermatol 1997; 137: 614-9.
9. Kim DS, Lee KY, Shin JU, Roh MR, Lee MG, Lupus miliaris disseminatus faciei without facial involvementActa Derm Venereol 2008; 88: 504-5.
10. Sehgal VN, Srivastava G, Aggarwal AK, Reddy V, Sharma S, Lupus miliaris disseminatus faciei. Part I: Significance of histopathologic undertones in diagnosisSkinmed 2005; 4: 151-6.
11. Al-Mutairi N, Nosology and therapeutic options for lupus miliaris disseminatus facieiJ Dermatol 2011; 38: 864-73.
12. Ganzetti G, Giuliodori K, Campanati A, Simonetti O, Goteri G, Offidani AM, Doxycycline-isoniazid: A new therapeutic association for recalcitrant acne agminataDermatol Ther 2012; 25: 207-9.
13. Beleznay K, Friedmann DP, Liolios AM, Lupus miliaris disseminatus faciei treated with 1,565 nm nonablative fractionated laser resurfacing: A case reportLasers Surg Med 2014; 46: 663-5.
14. Ming H. Jih, Paul M. Friedman, Arash Kimyai-Asadi, Friedman ES, Hymes SR, Goldberg LH, Lupus Miliaris Disseminatus Faciei. Treatment With the 1450-nm Diode LaserArch Dermatol 2005; 141: 143-5.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.