Mycosis fungoides: The great imitator
Vijaya Sajjan, Manisha Chandela, Ashok Maharudrayya Pandit, Basavapurada Manjunathswamy
ABSTRACT
Introduction: Mycosis fungoides although a cutaneous T-Cell lymphoma can immitate many dermatological disorders. A 60 year old man presented to our hospital with generalized annular plaques, few with verrucous surface. The annular lesions imitated Psoriasis, Tinea, Syphilis and the diagnosis was in dilemma. Histopathology gave the light and path to diagnosis. Case report: A 60 year old man presented with complains of erythematous scaly lesions since 20 year, Lesions were initially flat and erythematous which later became ulcerated, crusted and painful. H/O exacerbation and remission was present. Conclusions: Mycosis Fungoides is a great imitator both clinically and histopathologically. We are presenting a case report of patient with Mycosis Fungoides, Stage IIA.
Key words: Cutaneous T cell lymphoma; lymphoma; NB-UVB
INTRODUCTION
In the ocean of similar dermatological manifestations it is very important to keep an eye of eagle to diagnose a case. A patient presenting as chronic plaques psoriasis, which on investigation turned out to be Mycosis Fungoides.
CASE REPORT
A 60 year old man presented with multiple erythematous scaly plaques with ulcerations all over the body since 20 years. There was history of exacerbation and remission. Patient was treated by various doctors on the lines of Psoriasis and Tinea corporis without any improvement in patient condition. No history of recurrent fever or weight loss.
Mucocutaneous examination
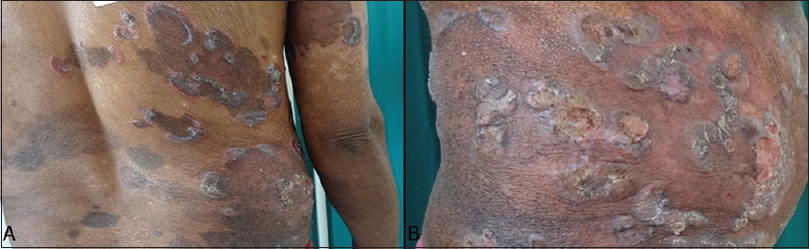
Multiple erythematous scaly plaques with circinate margins present over extremities and trunk with ulcerations (Figs 1A and B). Hyperpigmented patches were present over the trunk in bathing trunk pattern (Fig. 2).
Figure 1: (A and B) Multiple erythematous annular plaques with hyperpigmented patches and ulcerations
Figure 2: Hyperpigmented patches were present over the trunk in bathing trunk pattern
Multiple verrucous plaques present over the palms with ulceration and over dorsal aspect of feet (Figs 3A and B). Auspitz sign was negative. Lymph nodes.
Figure 3: (A and B) Multiple verrucous plaques were present over the palms and dorsal aspect of feet
Left inguinal lymph nodes enlarged approx 1 × 1 cm, soft and mobile with no dermopathic changes.
The patient’s informed consent was obtained.
INVESTIGATIONS
Complete blood count, Liver function test, Renal function test-were within normal limits. Peripheral Smear – Normal blood picture, no evidence of Sezary cells. KOH MOUNT – Negative for fungal filaments; V.D.R.L – Negative; H.I.V-I AND II – Negative; CT and M.R.I was advised but was deferred as the patient was not affordable. FNAC – Negative for atypical lymphoid cells.
SKIN BIOPSY – Showed moderately dense superficial perivascular patchy lichenoid infiltrate of lymphocytes with mild spongiosis within the epidermis. The epidermis shows slight psoriasiform hyperplasia and infiltration by numerous large lymphocytes without much spongiosis. The stratum corneum shows elongated mounds of parakeratosis. Several lymphocytes are aligned along the basal layer in toy soldier pattern. The papillary dermis shows thickening of collagen bundles that appear wiry. The above features are suggestive of plaque type of mycosis fungoides (Figs 4A and B).
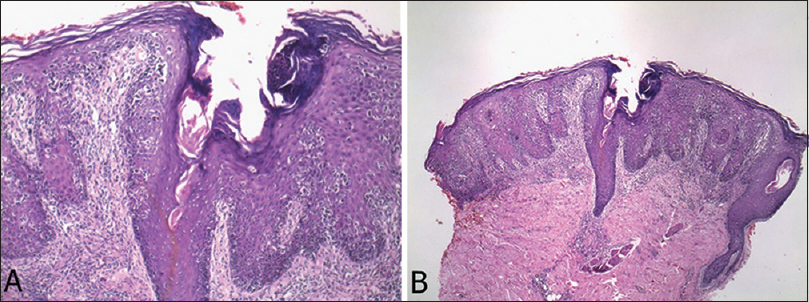
Figure 4: (A, B) Histopathological pictures showing moderately dense superficial perivascular patchy lichenoid infiltrate of lymphocytes with mild spongiosis within the epidermis. The epidermis shows slight psoriasiform hyperplasia and infiltration by numerous large lymphocytes without much spongiosis. The stratum corneum shows elongated mounds of parakeratosis. Several lymphocytes are aligned along the basal layer in toy soldier pattern. The papillary dermis shows thickening of collagen bundles that appear wiry
Prior to the study, every patient gave written consent to the examination and biopsy after having been informed about the procedure.
Differential diagnosis
- Tinea Corporis
- Chronic Plaques Psoriasis
- Secondary Syphilis
- Mycosis fungoides
Treatment
Patient was started on radiation therapy (NB-UVB), with topical steroids.
Outcome and follow-up
The lesion stopped spreading and improved but the patient was lost for the follow up.
DISCUSSION
Mycosis fungoides (MF) and the Sezary syndrome are a group of extranodal non-Hodgkin’s lymphomas of T-cell origin with primary cutaneous involvement. The group differs from other primary cutaneous T-cell lymphomas (CTCL) by its unique clinical features and histopathology [1].
In its early stages, it mimics many common benign dermatoses, and hence a definitive diagnosis can be delayed. The affected T cells are of CD4+ phenotype with loss of CD7 (pan-T-cell antigen) and demonstrate T-cell receptor (TCR) rearrangement. The prognosis of patients with MF is highly dependent on the extent and type of skin involvement. The initial cutaneous presentation of MF can be patches, plaques, tumors, or erythroderma. Patients who present with limited patch/plaque disease have good prognosis with an overall long-term survival that is similar to the expected survival of a matched control population whereas Patients with hypopigmented mycosis fungoides (HMF) present at a younger age in contrast to those with classic MF [2].
Patients presenting with limited or generalized patch/plaque type disease without peripheral lymphadenopathy can rarely exhibit extracutaneous involvement. Therefore, the staging evaluation differs for patients with MF compared to patients with other non-Hodgkin’s lymphomas. Patients with tumorous or erythrodermic type of skin involvement have a less favorable prognosis, while those presenting with extracutaneous disease have a poor prognosis. Myriad of therapeutic options are available for patients with MF and the Sezary syndrome.
Selection of a specific treatment plan is based primarily on the clinical stage of the disease.
Variants and subtypes
Folliculotropic mycosis fungoides – occurs in adults and men are most commonly affected. Presents as grouped erythematous follicular papules, acneiform lesions with severe pruritis, indurated plaques and rarely it is associated with non-scarring alopecia. Characteristic lesions are hairless infiltrated plaques.
Pagetiod Reticulosis-Localized types is characterized by presence of a single asymptomatic, psoriasiform, hyperkeratotic or circinate plaques on the extremities. Granulomatous Slack. Skin-occurs mostly in adult men. The flexure shows area of pendulous lax skin associated with Hogkins Lymphoma has been reported [3].
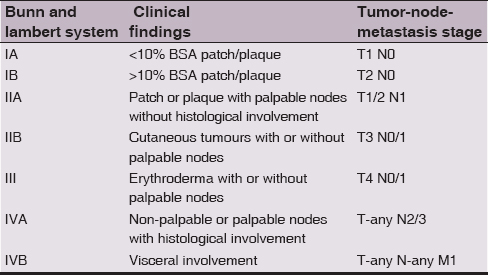
Staging
Various types of staging systems are done for Mycosis Fungoides. Two important once are TNM staging (Table 1) and Bunn and lambert system (Table 2) which involves clinical findings like body surface area involved, lymph node status and erythroderma. Staging of Mycosis Fungoide makes it easier to prognosticate and to make a treatment plan.
Table 1: Stages of Mycosis Fungoides. TNMB Classification of Mycosis Fungoides and Sezary Syndrome
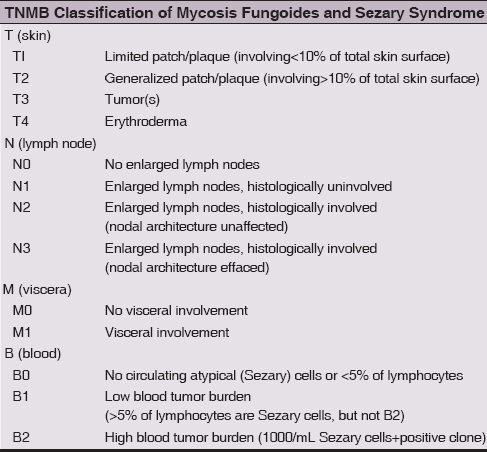
Table 2: Stages of Mycosis Fungoides. Bunn and Lambert system
Differential diagnosis
The differential diagnosis with Tinea corporis was ruled out on the basis of KOH mount as it was negative. Seconadry syphilis was ruled out by V.D.R.L negativity. There was no histopathological correlation with Chronic plaque psoriasis and there is no evidence that early aggressive systemic therapy is preferable to conservative therapy in the management of limited disease. Anticonvulsants such as carbamazepine, phenytoin, phenobarbital and valproic acid are the major offenders [4]. Out of these Carbamazepine induced pseudo-MF is the common one [5,6]. Drugs like Gleevec, protein tyrosine kinase inhibitor used in the treatment of chronic myelogenous leukemia, melanoma and gastrointestinal stromal tumor are also implicated [7].
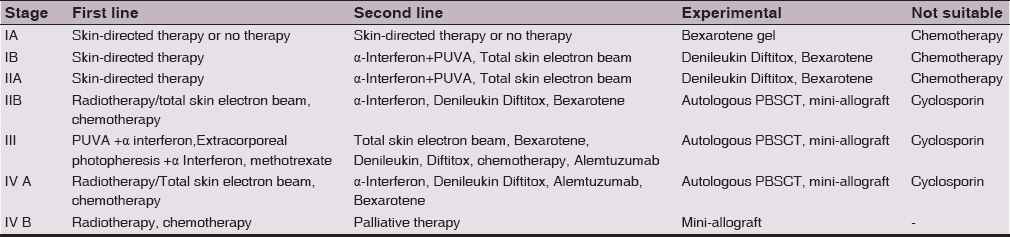
Treatment
Topical therapy is the main stay of treatment for patch/plaque type without extracutaneous involvement, whereas chemotherapy and other aggressive systemic regimens are reserved for recalcitrant disease or extracutaneous involvement [8]. Various treatment modalities (Table 3) are available for treatment of Mycosis Fungoides. Our patient was treated with topical steroids and Radiation therapy in the form of NB-UVB which led to improvement of lesions.
Table 3: Treatment of mycosis fungoides/Sezary syndrome
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. The examination of patients is conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Kim YH, Hoppe RT, Department of Dermatology, Stanford University School of Medicine, CA 94305, USASeminars Oncol 1999; 26: 276-89.
2. Castano E, Glick S, Wolgast L, Naeem R, Sunkara J, Elston D, Hypopigmented mycosis fungoides in childhood and adolescence: A long-term retrospective studyJ Cutan Pathol 2013; 40: 924-34.
3. Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, WHO- EORTC classification for cutaneous lymohomasBlood 2005; 105: 3768-85.
4. Choi TS, Doh KS, Kim SH, Jang MS, Suh KS, Kim ST, Clinicopathological and genotypic aspects of anticonvulsant induced pseudolymphoma syndromeBr J Dermatol 2003; 148: 730-6.
5. Gul U, Kilic A, Dursun A, Carbamazepine – induced pseudomycosis fungoidesAnn Pharmacother 2003; 37: 1441-3.
6. Miranda-Romero A, Pérez-Oliva N, Aragoneses H, Bastida J, Raya C, González-Lopez A, Carbamazepine hypersensitivity syndrome mimicking mycosis fungoidesCutis 2001; 67: 47-51.
7. Clark SH, Duvic M, Prieto VG, Mycosis fungoides- like reaction in a patient treated with GleevecJ Cutan Pathol 2003; 30: 279-81.
8. Journal of the National Comprehensive Cancer Network 2008; April6: Number 4
Notes
Source of Support: Nil
Conflict of Interest: None declared.


Comments are closed.