Profile of post-herpetic neuralgia – A clinico-epidemiological study
1Department of Anesthesiology, Government Medical College, Jammu, India, 2Consultant Dermatologist, Treatwell Skin Centre, Jammu, India
Corresponding author: Dr. Mrinal Gupta
Submission: 01.03.2020; Acceptance: 06.04.2020
DOI: 10.7241/ourd. 2019e.36
Cite this article: Gupta H, Gupta M. Profi le of post-herpetic neuralgia – A clinico-epidemiological study. Our Dermatol Online. 2019;10(e):e36.1-e36.3
Citation tools:
Copyright information
© Our Dermatology Online 2020. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Post herpetic neuralgia (PHN) is one of the most common complications of herpes zoster which can have a significant impact on the quality of life.
Aims and objectives: This study was carried out to study the clinic-epidemiological features of PHN.
Materials and Methods: It was a prospective, observational study carried out over a period of one year in which fifty patients with PHN were included and their epidemiological and clinical features were noted in a predesigned pro forma.
Results: The age range of the study group (M: F 31:19) ranged from 17-84 years with a mean age of 59.8±4.2 years. The duration of PHN varied from 1 month to 13 months with a mean of 2.4 months. The most common dermatomes of involvement were thoracic in 42% (n=21), ocular in 22% (n=11), cervical in 18& (n=9) and lumbar in 12% (n=6). In our study group, 38% (n=19) did not take any medication for herpes zoster, 16% (n=8) took delayed treatment and 24% (n=12) took incomplete treatment and only 22% (n=11) respondents took timely and complete treatment. There was a history of application of indigenous medications over herpes zoster in 68% (n=34) respondents. Associated comorbidities were present in 34% (n=17) of the respondents.
Conclusion: PHN is a common complication of Herpes Zoster, common among elderly and its incidence increases when Herpes Zoster is left untreated or with incomplete treatment.
Key words: Herpes zoster; Post herpeticneuralgia; Pain; Dermatomes.
INTRODUCTION
Post herpetic neuralgia (PHN) is defined as the debilitating, chronic pain lasting at least three months after resolution of herpes zoster. It is characterized by a constant burning, stabbing or shooting pain or lancinating pain, but some patients may present with features of numbness, itching, tingling, or allodynia [1,2]. It has been associated with sleep disturbances, anorexia, chronic fatigue and weight loss. It causes significant reduction of quality of life and can cause significant suffering both for the patient and the caregiver [3]. The estimates of prevalence of PHN vary but researchers have reported that PHN may develop in 10-20% of the patients, which tends to increase markedly with age and in the presence of associated comorbidities [4,5]. Timely initiation of antiviral therapy has been associated with significant reduction in the development of PHN [6].
We carried out this study to assess the clinical and epidemiological characteristics of patients with PHN in our setup.
MATERIALS AND METHODS
It was a prospective, observational study carried out over a period of one year in which fifty patients with PHN were included and their epidemiological and clinical features were noted in a predesigned pro forma after taking an informed consent.
RESULTS
The clinic-epidemiological characteristics of respondents in our study are given in Table 1. The age range of the study group (M: F 31:19) ranged from 17-84 years with a mean age of 59.8±4.2 years. The duration of PHN varied from 1 month to 13 months with a mean duration of 2.4 months. The most common dermatomes of involvement were thoracic in 42% (n=21), ocular in 22% (n=11), cervical in 18& (n=9) and lumbar in 12% (n=6). Majority of patients in our study belonged to a rural background (68%, n=34) and were either illiterate (24%, n=12) or had a schooling upto high school (42%, n=21). In our study group, 38% (n=19) did not take any medication for herpes zoster, 16% (n=8) took delayed treatment and 24% (n=12) took incomplete treatment and only 22% (n=11) respondents took timely and complete treatment. None of the respondents in our study had varicella vaccination. There was a history of application of indigenous medications over herpes zoster in 68% (n=34) respondents, with ayurvedic and herbal preparations being the most common medications. Associated comorbidities were present in 34% (n=17) of the respondents with diabetes mellitus being the most common, present in 18% (n=9), followed by hypertension in 12% (n=6), systemic malignancy in 6% (n=3) and chronic kidney disease in 4% (n=2).
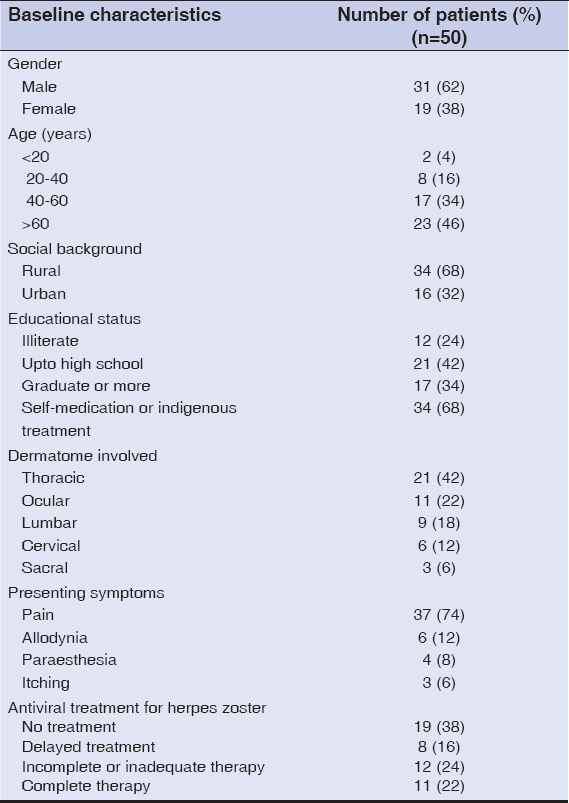 |
Table 1: Clinico-epidemiological characteristics of the study group |
DISCUSSION
PHN is a chronic debilitating complication of Herpes zoster which is caused due to damage to the sensory nerves which lead to activity of primary afferent neurons resulting in their spontaneous activity which causes continuous pain in the absence of any continuous tissue damage. The pain in PHN may be intermittent or continuous and is usually does not correlate with any external stimuli. Some patients also present with allodynia with a light touch causing a severe lancinating pain. Pain may not be the presenting feature in a few patients, where PHN presents as persistent itching, sensory loss or a persistent tingling sensation [1–3].
Many researchers have reported a female predominance in the incidence of PHN but in our study, males outnumbered females (M: F 31:19). Increasing age and greater extent of rash are risk factors for the development of PHN [7,8]. Researchers have reported that both the frequency and severity of PHN is increased in patients aged 60 years or more.The risk of PHN has been reported to be 2% in patients younger than 50 years of age,which increases to 20% in those older than 50 years andis maximum (35%)in those aged above 80 [9]. We also reported a higher incidence among elderly in our study. The localization of herpes zoster has also been reported to be a risk factor for development of PHN with thoracic localization having a higher risk of developing PHN, which was also seen in our study with thoracic predominance [7–9]. The timely and adequate therapy with antivirals has been seen to reduce the incidence of PHN, but in a developing country like India, the limited availability and the lack of awareness among the general population are major factors due to which a large number of patients do not take proper treatment which, in turn, may lead to an increased incidence of PHN.
Our study had certain limitations. We had less number of patients and all of them were from a single centre, which may not represent the whole population. Moreover, we could not follow up the patients, so were unable to assess the course of PHN in the patients.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med.2002;347:340-6.
2. Oxman MN. Immunization to reduce the frequency and severity of herpeszoster and its complications. Neurology. 1995;45:S41-6.
3. Oster G, Harding G, Dukes E, Edelsberg J, Cleary PD. Pain, medicationuse, and health-related quality of life in older persons with postherpeticneuralgia:results from a population-based survey. J Pain. 2005;6:356-63.
4. Arani RB, Soong SJ, Weiss HL, Wood MJ, Fiddian PA, Gnann JW, et al. Phase specific analysis of herpes zoster associated pain data:a newstatistical approach. Stat Med. 2001;20:2429-39.
5. Desmond RA, Weiss HL, Arani RB, Soong SJ, Wood MJ, Fiddian PA, et al.Clinical applications for change-point analysis of herpes zoster pain. J PainSymptom Manage. 2002;23:510-6.
6. Dworkin RH. Post-herpetic neuralgia. Herpes. 2006;13 Suppl 1:21A-7.
7. Costache C, Costache D. A study of the dermatoses in herpes zoster. BullTransilvania Univ Braşov Ser VI Med Sci. 2009;2:19-24.
8. Jung BF, Johnson RW, Griffi n DR, Dworkin RH. Risk factors for postherpeticneuralgia in patients with herpes zoster. Neurology. 2004;62:1545-51.
9. Gupta V, Mittal A, Rai G. Risk factors for post herpetic neuralgia:A longitudinal study. Int J Sci Stud. 2014;2:79-82.
Notes
Source of Support: Nil.
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.