Paraneoplastic pemphigus: Diagnosing with a modified criteria – A case report
Snehal Lunge 1, Pallavi Singh1, Arvind Rajbhog Ashwin2
1, Pallavi Singh1, Arvind Rajbhog Ashwin2
1Department of Dermatology, Bharati Vidyapeeth (DTU) Medical College, Pune, Maharashtra – 411043, India, 2Department of Medical Oncology, Bharati Vidyapeeth (DTU) Medical College, Pune, Maharashtra – 411043, India
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Paraneoplastic pemphigus is a rare autoimmune blistering disorder which presents with polymorphous cutaneous lesions and recalcitrant stomatitis. The disorder has a 100% association with an underlying neoplasia, primarily lymphoproliferative disorders. We report a patient who presented with oral mucosal lesions resistant to treatment with bullous cutaneous lesion and an underlying NHL-B cell lymphoma. The condition since its inception has been diagnosed using the criteria by Anhalt et al, which still is the most standard one. The criterion has been revised and updated every now and then. A current update has been proposed by Svoboda SA et al, which is a more relaxed one making diagnosis easier in a patient of Paraneoplastic pemphigus. Our patient was confidently diagnosed with Paraneoplastic pemphigus using this criterion. A quick diagnosis with fewer investigations allowed early and aggressive institution of treatment, to which patient responded well.
Key words: Paraneoplastic pemphigus; NHL-B cell Lymphoma; Rituximab; Bendamustine
INTRODUCTION
Cutaneous paraneoplastic syndromes comprise of those skin conditions which have an association with underlying neoplasia in variable frequencies. Paraneoplastic pemphigus (PNP) is one such condition wherein the cutaneous disease has a 100% association with an underlying malignancy and is a life-threatening condition. It was first described in 1990, and since then roughly 500 cases have been reported [1]. The skin features are not due to tumor invasion or metastasis [2] but due to antibodies against various autoantigens like plakins, Dsg 1 and 3, BP antigen 1and plectins. The condition in has a poor prognosis and requires aggressive treatment. Therefore, early identification and treatment can have a positive bearing on patient’s clinical condition, underlying neoplasm, and quality of life. PNP has classically been diagnosed with the criteria described by Anhalt et al. [3] The criteria by Camisa and Helm [4] is another revised version. Further revision after reviewing 265 cases of paraneoplastic pemphigus has been updated by Svoboda SA et al. [5].
We report a case of Paraneoplastic pemphigus which successfully verifies this criterion.
CASE REPORT
A 67-year-old female patient presented with painful ulcers over lips and within oral cavity since last 3 months, insidious in onset and progressive in nature, making patient shift completely to liquid diet.
After a period of two and half months, oral lesions were followed by an acute onset bullous skin lesions over trunk and extremities which progressed rapidly over the next 10 days.
Patient also gave history of a swelling on the right side of the neck since last 3 years with an increase in size in last 4 months. She had been investigated for it 2 years ago and the swelling was diagnosed as a lymphoproliferative disorder. She took treatment for it in form of alternative medicine, with no response.
There was no history of any recent fever, or any new oral medication intake before the onset of mucocutaneous lesions.
On examination, multiple tense and flaccid bullae were present over the chest, trunk, glutei, thighs, and arms. Their size varied from 1cm to 6 cm in diameter. Many bullae showed an erythematous to violaceous surrounding ring suggestive of targetoid lesion (Fig. 1a). Nikolsky sign was negative.
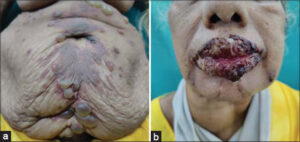 |
Figure 1: (a) Multiple bullae over trunk, with surrounding violaceous ring. (b) Adherent hemorrhagic and purulent crust over lips. |
Patient had adherent purulent to hemorrhagic crust over upper and lower lips (Fig. 1b). The buccal mucosa, tongue and gingivae had diffuse erosions and ulcers with overlying yellowish-white slough.
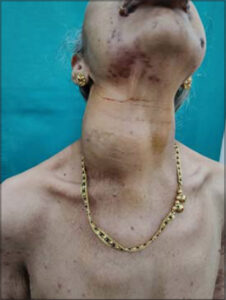
A single hemispherical swelling, with smooth surface, measuring 15cm by 12 cm was present on right side of neck, anterolaterally (Fig. 2). There was no associated lymphadenopathy or organomegaly on systemic examination.
Tzanck smear performed from a bulla showed acantholytic cells.
Biopsy done from a newly developed bulla showed a suprabasal cleft with acantholytic and few inflammatory cells and was suggestive of pemphigus vulgaris (Fig, 3a).
 |
Figure 3: (a) Lesion biopsy showing suprabasal cleft with acantholytic cells. (b) Direct immunofluorescence showing IgG deposition in intercellular spaces of epidermis. |
A direct immunofluorescence test done from a perilesional skin biopsy showed IgG +++ in the intercellular spaces of epidermis (Fig. 3b). IIF and Immunoprecipitation was not performed because of cost restraints.
The swelling in the neck was evaluated by oncology department. A USG guided biopsy followed by Immunohistochemistry reported it as non-Hodgkin B-cell Lymphoma.
The laboratory tests done showed raised serum CRP levels and serum LDH levels, with no other abnormalities.
As per criteria by Svoboda SA et al [5], patient was diagnosed as Paraneoplastic pemphigus.
She was started on systemic corticosteroids, oral and topical antibiotics. For the mucosal care, patient was given povidone iodine gargles and was advised frequent Chlorhexidine mouthwash. A syrup preparation containing oxetacaine was given before food for anesthesia and pain relief.
2 weeks later, she received injection Rituximab and Bendamustine. In 4 weeks since the systemic steroid was started and in 2 weeks after a single dose of Rituximab and Bendamustine, all cutaneous lesions had resolved showing post inflammatory hyperpigmentation (Fig. 4). The oral lesions showed improved but did not resolve completely.
DISCUSSION
Paraneoplastic pemphigus is a life-threatening autoimmune disorder, always associated with an underlying neoplasia, primarily lymphoproliferative disorders. The most common one being Non-Hodgkin B-cell lymphoma.
The condition classically presents with recalcitrant stomatitis and polymorphous cutaneous lesions in form of bullous lesion, erythema multiforme, lichenoid dermatitis and graft vs host disease.
Our patient described also presented with a recalcitrant mucositis of 3 months duration with bullous and targetoid lesions and an underlying NHL B-cell lymphoma.
The classical diagnostic criterion for PNP is the one given by Anhalt et al. [3] which comprises of 5 features:
-
1) Painful mucosal erosions and polymorphic cutaneous lesions with an underlying occult or diagnosed malignancy;
-
2) Histopathogical features corresponding to the cutaneous lesions;
-
3) Direct immunofluorescence showing IgG and C3 deposition in the epidermal intercellular spaces and granular/linear complement along basement membrane;
-
4) Indirect immunofluorescence showing serum IgG binding to skin, mucosa, simple, columnar, and transitional epithelium;
-
5) Immunoprecipitation showing desmoplakin, periplakin, envoplakin, desmoglein 1 and 3 and BP antigen 1.
Ideally all 5 features should be present for diagnosis of PNP.
In any patient, demonstrating all the 5 features can be challenging, given the limitations of cost, restricted availability of facilities providing immunoprecipitation.
In our patient too, the first 3 criteria were fulfilled but the last 2 could not be achieved due to cost limitations.
This can limit early diagnosis and treatment initiation. For this reason, the criteria by Anhalt et al has been revised several times.
A popular modified criteria is given by Camisa and Helm [4] which has further been revised and simplified.
One such revision has been done by Svoboda SA et al. [5] which was done after reviewing 265 cases of PNP. It comprises of following features.
Major criteria
-
1) Mucous membrane lesion with or without cutaneous involvement;
-
2) Accompanying internal neoplasm;
-
3) Evidence of anti-plakin antibodies by ELISA, indirect immunofluorescence on transitional epithelium, immunoblot or immunoprecipitation.
Minor criteria
-
1) Acantholysis and/or lichenoid interface dermatitis on biopsy;
-
2) Intercellular and/or basement membrane staining with direct immunofluorescence.
Paraneoplastic pemphigus can be diagnosed with above criteria if:
- All 3 major criteria are met, or
- If 2 major and both minor criteria are met
This criterion improves the sensitivity of Camisa and Helm’s criterion [4] from 71.2% to 89.4%.
Our patient had 2 major and both minor criterion present, and hence was confidently diagnosed with PNP.
It is known that both auto-antibodies and cell mediated immunity plays a role in pathogenesis of the disease. Therefore, a treatment tailored to affect both is adopted. Moreover, a multidisciplinary approach by Dermatologists and Oncologists is needed for the patient. High dose systemic steroids are first line treatment for cutaneous lesions. Commonly, systemic steroids with Rituximab are used to treat PNP with NHL-B cell lymphoma. Additionally, meticulous care for oral lesions is required. Similar approach was taken for our patient too, and it was noticed that both cutaneous and oral lesions responded to a combination of systemic steroids with Rituximab and Bendamustine. However, the cutaneous lesions responded faster and completely compared to the oral lesions.
Alternative treatment options that have been tried including Azathioprine, Cyclosporine, cyclophosphamide, IVIG and plasmapheresis. Daclizumab, a humanized monoclonal antibody against IL-2 receptor of T-cells, is being considered as a promising option [6].
CONCLUSION
Paraneoplastic pemphigus continues to be a rare disorder, which associated high rate of morbidity and mortality. An earlier detection and early initiation of therapy plays vital role in the prognosis of the disease. An increased sensitivity among Dermatologists towards clinical suspicion of autoimmune mucocutaneous blistering disorder with systemic associations can enhance case detections. It must be emphasized that this condition requires a multidisciplinary approach from Dermatologists, oncologists, ophthalmologists, and surgeons for optimal treatment.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCE
1. Yee MD, Seline A, Young K, Wanat KA. Paraneoplastic pemphigus secondary to neuroendocrine carcinoma. JAAD Case Rep. 2021;15:22-5.
2. Anhalt GJ. Paraneoplastic pemphigus. J Investig Dermatol Symp Proc. 2004;9:29-33.
3. Anhalt GJ, Kim SC, Stanley JR, Korman NJ, Jabs DA, Kory M, et al. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med. 1990;323:1729-35.
4. Camisa C, Helm TN. Paraneoplastic pemphigus is a distinct neoplasia-induced autoimmune disease. Arch Dermatol. 1993;129:883-6.
5. Svoboda SA, Huang S, Liu X, Hsu S, Motaparthi K. Paraneoplastic pemphigus:Revised diagnostic criteria based on literature analysis. J Cutan Pathol. 2021;48:1133-8.
6. Paolino G, Didona D, Magliulo G, Iannella G, Didona B, Mercuri SR, et al. Paraneoplastic Pemphigus:Insight into the Autoimmune Pathogenesis, Clinical Features and Therapy. Int J Mol Sci. 2017;18:2532.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.