Psychiatric comorbidities among patients of Prurigo nodularis: A cross sectional study in tertiary care hospital south India
Soumya G Hegde 1, YR Niranjan Hebbar2, Swathi2
1, YR Niranjan Hebbar2, Swathi2
1Department of Dermatology, SUIMS, Shivmogga, India, 2Department of Psychiatry, SUIMS, Shivmogga, India
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Prurigo nodularis (PN) is a dermatologic itchy condition which affects the normal day to day life activities. Due to its chronic condition psychiatric comorbidities are regularly seen in these patients. Due to scarcity of literature in Indian background this study was conducted in our tertiary care centre.
Materials and methodology: It was a descriptive, cross sectional study conducted at department of dermatology during May 2021 to April 2022 where all diagnosed PN patients were screened for psychiatric comorbidities using MINI- International Neuropsychiatric interview.
Results: We found Generalised Anxiety Disorder among 27.2% and Major Depressive Disorder among 15.8% of study population. Also Social phobia among 16.8% of males. Majority of 61% in both males and females didn’t had any psychiatric disorders in our study sample.
Conclusion: Higher incidences of anxiety, depression, somatization were found in our study sample thus highlighting the importance of psychiatric consultation liaison for chronic skin conditions.
Key words: Prurigo Nodularis; Anxiety; Somatization; Depression
INTRODUCTION
Owing to the same ectodermal embryonic origin, Skin and Nervous System share many similar connections throughout the life [1]. Prurigo nodularis (PN) is one of the common skin conditions which due to its chronicity and difficulty to respond to plethora of treatments available, poses a significant implications in the psychological aspect of living [2]. Emotional instabilities with chances in inflammatory markers like cytokines, neuropeptides etc can trigger or perpetuate the course of PN [3]. Although there are some evidences in the literature of having increased psychiatric morbidities like depression and anxiety among patients with Prurigo Nodularis, there is limited literature among Indian population [4–6]. This study was conducted to assess psychiatric comorbidities among patients of PN which helps for the comprehensive management including expertise from both the departments of psychiatry and dermatology.
MATERIAL AND METHODS
A cross sectional study was conducted in the department of dermatology in a tertiary care hospital, south India after the approval of ethical committee. All diagnosed patients of PN aged between 18-60 years, who visited dermatology outpatient department, irrespective of their gender were included in the study. This study was conducted during May 2021 to April 2022. Patients with significant medical illness or intellectually retarded are excluded from the study. Socio demographic details were entered in a semi structured format. Psychiatric morbidities were assessed using Mini international neuropsychiatric interview (MINI): It is a brief, validated and reliable structured diagnostic interview to assess psychiatric morbidities [7]. Data were analysed using Statistical Package for Social Sciences software, version 18.0 (SPSS) [8].
RESULTS
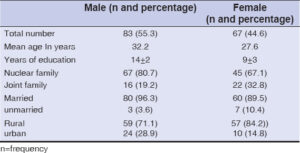
A total of 150 patients were included in the study. Out of which majority of 83 were males and rest 67 were females. Mean age for males was 32.2years. Mean years of education among males were 14±2 and for females were 9±3. A total of 67 males and 45 females were from joint family background and majority of 80 males and 60 females were married during the time of our study. 59 males and 57 females were from rural area of living and the rest from urban background (Table 1).
Social phobia was found to be higher in males (16.8%) and generalised anxiety disorder among females (16.4%) in our study sample. Major Depressive Disorder was found in 8.4% males and 7.4% in females. Whereas 2 of the males had somatisation disorder and majority of (61%) in both males and females didn’t had any psychiatric symptoms (Table 2).
DISCUSSION
Psychiatric morbidities were found to be significantly higher in many patients of PN compared to general population. Similar findings were found in many of the studies in the literature [9–15]. Mean age in our study sample was 29.9 years. In many of the studies the mean age was found 10±2 years [12]. Generalised anxiety disorders were found among 27.2% in our study group and MDD in 15.8% which are in line with studies conducted. Hypochondriasis was found in 2.4% of PN patients in our study. Similarly in another study they found higher prevalence of alexithymia, hypochondriasis, anxiety and depression in patients of Prurigo Nodularis [12–16]. Smaller sample size and single centre study were one of the limitations in our study. As significant psychiatric morbidities were found in many patients of Prurigo Nodularis the importance of cross consultation is highlighted here in our study.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Augustin M, Gieler U, Zschocke I. Psychodermatology has come out of its infancy. Dermatol Psychosom. 2004;5:3-4.
2. Dazzi C, Erma D, Piccinno R, Veraldi S, Cassialansa M. Psychological factors involved in prurigo nodularis:A pilot study. J Dermatolog Treat. 2011;22:211 4.
3. Radmanesh M, Sharifi M, Shafiei S. Lichen simplex chronicus, neurotic excoriation and nodular prurigo and their correlation with atopy:A case-control study. Iran J Dermatol. 2011;14:25-8.
4. Coşkun BK, Atmaca M, Saral Y, Coskun N. Prevalence of psychological factors in chronic dermatoses. Int J Psychiatry Clin Pract. 2005;9:52 4.
5. Jørgensen KM, Egeberg A, Gislason GH, Skov L, Thyssen JP. Anxiety, depression and suicide in patients with prurigo nodularis. J Eur Acad Dermatol Venereol. 2017;31:106 7.
6. Dhawan L, Singh SM, Avasthi A, Kumaran MS, Narang T. The prevalence of psychiatric comorbidity in patients with prurigo nodularis. Indian Dermatol Online J. 2018;9:318-21.
7. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P,Janavs J, Weller E, et al., The mini-international neuropsychiatric interview (M.I.N.I.):THE development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22-33;quiz 34-57.
8. SPSS Inc. SPSS for Windows. Chicago, IL;2009.
9. Schneider G. Psychosomatic aspects and psychiatric conditions. In:Pruritus. London:Springer-Verlag. 2010;211-5.
10. Ranjan JK, Asthana HS. Prevalence of mental disorders in India and other South Asian countries. Asian J Epidemiol. 2017;10:45-53.
11. Boozalis, E, Tang, O, Patel S, Semenov YR, Pereira MP, Stander S,et al. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol. 2018;79:714–9.
12. Zeidler C, Tsianakas A, Pereira M, Ständer H, Yosipovitch G, Ständer S. Chronic Prurigo of Nodular Type:A Review. Acta Derm Venereol. 2018;98:173-9.
13. Singam V, Patel KR, Silverberg JI. Association of prurigo nodularis and lichen simplex chronicus with hospitalization for mental health disorders in US adults. Arch Dermatol Res. 2020;312:587-93.
14. Williams KA, Huang AH, Belzberg M, Kwatra SG. Prurigo nodularis:Pathogenesis and management. J Am Acad Dermatol. 2020;83:1567-75.
15. Zeidler C, Yosipovitch G, Ständer S. Prurigo Nodularis and Its Management. Dermatol Clin. 2018;36:189-97.
16. Lanza G, Cosentino FII, Ferri R, Lanuzza B, Siragusa M, Tripodi M,et al. Cognitive impairment in inpatients with prurigo nodularis and psychiatric comorbidities. Int J Environ Res Public Health. 2021;18:62-5.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.