Basal cell carcinoma of the external auditory canal: Case report and literature review
Kaoutar Soussy 1, Chaymae Jroundi2, Soukaina Lahmer1, Nawal Hammas3, Zenab Alami1, Fatima Zahra Mernissi2, Touria Bouhafa1
1, Chaymae Jroundi2, Soukaina Lahmer1, Nawal Hammas3, Zenab Alami1, Fatima Zahra Mernissi2, Touria Bouhafa1
1Radiation Oncology Department, Oncology Hospital, Hassan II University Hospital, Fes, Morocco, 2Dermatology Department, Hassan II University Hospital, Fes, Morocco, 3Anatomopathology Department, Hassan II University Hospital, Fes, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Basal cell carcinoma is a common, slowly growing, locally aggressive, and rarely metastatic skin cancer. Primary BCCs of the external auditory canal are extremely rare. A 67-year-old patient presented chronic otitis media associated with a mass in the concha and the external auditory canal of the left ear. The patient was diagnosed with basal cell carcinoma of the EAC. Locoregional assessment on a CT scan revealed thickening of soft tissues in the external left auricle and external auditory canal. She underwent surgery. Given the insufficient margins, adjuvant radiotherapy was indicated. Radiotherapy was performed with the intensity-modulated radiation therapy technique in order to the overcome anatomical complexity of the region, cover the tumor bed, and preserve the organs at risk. BCC of the EAC is a rare and challenging entity, whose management is multidisciplinary. The main goal is to avoid local recurrence, as well as to improve the patient’s quality of life.
Keywords: Basal cell carcinoma; External auditory canal; IMRT; Local control
INTRODUCTION
Basal cell carcinoma (BCC) is the most common cancer worldwide and is a slowly growing, locally aggressive, and rarely metastatic cancer. BCC accounts for approx. three-quarters of all non-melanoma skin cancers, and the incidence is increasing at an exponential rate among regions in which white-skinned people are predominant, such as North America, Europe, and Australia [1].
Primary carcinomas of the external auditory canal are extremely rare. These include squamous cell carcinoma, basal cell carcinoma, melanoma, adenoid cystic carcinoma, and adenocarcinoma [2].
Because of the rarity of BCC of the external auditory canal (EAC), there are no randomized clinical trials and the management of these tumors is difficult and not standardized.
Herein, we report a case of BCC of the EAC and review the literature.
CASE REPORT
Our patient was a 67-year-old female with no previous medical history. The symptoms began one year before her consultation in our department for chronic otitis media and the progressive increase of a nodule at the concha of the left ear, which extended to the EAC and retro-auricular region.
She consulted in the ENT (ear–nose–throat) Department of the Hassan II University Hospital in Fez, Morocco, for a budding lesion of the concha of the left ear extending into the EAC, which obstructed it completely with purulent otorrhea. A biopsy was performed and a CT scan was requested.
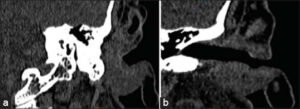
A CT scan of the left temporal bone showed an infiltrating process in the inferior portion of the external auditory canal, 16 mm in diameter and extending for 25 mm, with irregular contours, in contact with the tympanic bone, without any adjacent bone reaction. It infiltrated the external surface of the superficial lobe of the parotid gland, tragus, antitragus, antihelix, and retroauricular groove. The facial nerve was intact (Figs. 1a and 1b).
A biopsy of the tumor revealed infiltrating basal cell carcinoma. The case was discussed by the multidisciplinary tumor (MDT) board and the decision was upfront surgery. The patient underwent surgery with tumor resection reaching deeply into the eardrum, with the removal of the skin of the EAC and overlapping of the upper part. As a postoperative complication, she had left facial paralysis.
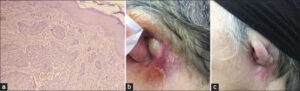
A pathology report of the surgical specimen confirmed the diagnosis of infiltrating BCC. The resection limits were 5 mm from the medial border, 7 mm from the superior border, and 4 mm from the retroauricular border (Fig. 2a).
Given that the resection limits were insufficient, adjuvant radiotherapy was indicated by the MDT board in consultation with dermatologists and ENT specialists (Fig. 2b).
After the complete healing of the wound, she was scheduled for a total dose of 64 Gy of RT in 32 fractions, at a daily dose fraction of 2 Gy over 6.5 weeks with the IMRT technique. We were able to keep the tolerance doses of the organs at risk within normal limits and, at the same time, deliver the intended dose of radiation to the tumor bed (Figs. 3a and 3b).
 |
Figure 3: (a) Disposition of multiple IMRT beams on the three plans (axial, sagittal, and coronal). (b) Dosimetry images in three planes showing the 95% isodose conforming to PTVs (in red). |
She was able to receive her RT as planned and was seen weekly with good tolerance, with no side effects noted except for grade 2 radiodermatitis, which was managed with topical steroids by the dermatologist (Fig. 2c).
After eighteen months of follow-up, the patient was seen every three months for a clinical examination and CT scan every six months without evidence of disease.
DISCUSSION
The majority of BCCs occur in the head and neck [3]. Carcinomas of the external auditory canal (EAC) are rare tumors. They occur every year in 1 out of 5000–15000 patients with otological diseases. It is known to have a locally aggressive nature and no regional lymph node metastasis, and, therefore, to have a better prognosis [4].
CT scans are helpful in detecting bone involvement beyond the external canal, yet could miss soft tissue extension. MRI might be more beneficial in evaluating the extensive lesions [2].
As for the management of these tumors, the literature on carcinoma of the external auditory canal suggests that surgery is the primary treatment. Crabtree et al. demonstrated that, in localized tumors, it is possible to perform a wide en bloc resection of the bony and cartilaginous external auditory canal, including the tympanic membrane and malleus and, if necessary, the superficial lobe of the parotid [5].
In the case of localized tumors, en bloc resection of the external auditory canal offers a high curing rate. In extensive lesions, en bloc dissection removing the bulk of the tumor mass followed by irradiation seems to offer at least as good of a prognosis as more radical surgery [5]. An update of this study by Shih et al. [2] showed that the prognosis for localized tumors treated by en bloc resection remains excellent, whereas the prognosis for extensive lesions might be more dependent on the histological subtype and grade of the tumor.
Surgery on BCC of the EAC is quite challenging. Due to the particular location of these tumors, the ability to perform a wide excision remains difficult, in addition to the aggressiveness of certain histological subtypes [3].
BCC is generally considered radioresponsive, and both adjuvant radiation therapy and primary radiation therapy have been employed successfully for head and neck BCC [6]. Therefore, postoperative RT is indicated in situations in which the probability of residual disease after surgery is high and the chance of successful curative treatment is modest (perineural invasion or positive margins). As for definitive RT, it is recommended for treating the early stages in locations where resection would result in a significant cosmetic and/or functional deficit [7].
CONCLUSION
It has been demonstrated that BCC that impinges upon or invades the external auditory canal is associated with a higher risk of local recurrence [6]. Moreover, it is a rare tumor with a particular and hidden localization, which makes it difficult to diagnose, even at a locally advanced stage, as was the case in our patient. The treatment is multidisciplinary based on surgery and radiotherapy, with the main goal to avoid local recurrence, as well as to improve the patient’s quality of life.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Devine C, Srinivasan B, Sayan A, Ilankovan V. Epidemiology of basal cell carcinoma:A 10-year comparative study. Br J Oral Maxillofac Surg. 2018;56:101-6.
2. Nyrop M, Grøntved A. Cancer of the external auditory canal. Arch Otolaryngol Head Neck Surg. 2002;128:834–7.
3. Gill AS, Nittur VR, Moore MG, Farwell DG, Bewley AF. Oncologic outcomes after surgery for locally aggressive basal cell carcinoma of the head and neck. Laryngoscope. 2020;130:115 9.
4. Ogawa K, Nakamura K, Hatano K, Uno T, Fuwa N, Itami J, et al. Treatment and prognosis of squamous cell carcinoma of the external auditory canal and middle ear:A multi-institutional retrospective review of 87 patients. Int J Radiat Oncol Biol Phys. 2007;68:1326-34.
5. Gidley PW. Squamous cell carcinoma and basal cell carcinoma of the ear canal and temporal bone. In:Gidley PW, DeMonte F, éditeurs. Temporal Bone Cancer [Internet]. Cham:Springer International Publishing;2018
6. Breen JT, Roberts DB, Gidley PW. Basal cell carcinoma of the temporal bone and external auditory canal. Laryngoscope. 2018;128:1425 30.
7. Mendenhall WM, Amdur RJ, Hinerman RW, Cognetta AB, Mendenhall NP. Radiotherapy for cutaneous squamous and basal cell carcinomas of the head and neck. Laryngoscope. 2009;119:1994-9.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.