Do we need new therapeutic agents or should we only improve patients’ compliance?
Dermedic Jacek Zdybski Private Dermatology Outpatients Clinic, Ostrowiec Świętokrzyski, Poland
Corresponding author: Jacek Zdybski, MD
How to cite this article: Zdybski J. Do we need new therapeutic agents or should we only improve patients’ compliance?. Our Dermatol Online. 2022;13(e):e39.
Submission: 23.01.2022 Acceptance: 01.02.2022
DOI:10.7241/ourd.2022e.39
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Treatment outcomes depend on several factors. Adherence to dermatological treatment is especially difficult to achieve due to different ways of application of prescribed meds: oral, intramuscular, subcutaneous or topical. Clinical research mainly focuses on new treatment methodologies with more targeted methods of action with less potential for side effects. The issue of compliance of currently available therapeutic agents seems to attract less attention and the author of this paper tries to establish if by improving compliance physicians may also improve the outcome of treatment.
Methods: patients adherence to treatment protocols was evaluated in three cohorts of patients, treated in dermatology outpatient setting between January 2020 and November 2021 for facial acne, scalp psoriasis or plantar verrucae. Each cohort consisted of 12 patients. Treatment outcomes in each group were analysed and compared against treatment compliance rates. Treatments were the same for patients in each cohort.
Results: patients in facial acne cohort who improved by 2 scores had mean compliance level of 89%, whereas those who improved by 1 score had compliance of 72.6%. Scalp psoriasis patients observed improvement of 2 scores, 1 score or no improvement. Patients who improved by 2 scores sticked to all recommendations (including asking for assistance with applying solution to scalp) more often than in groups who improved by 1 or who saw no improvement (85.7% vs 50% vs 0%). Patients with plantar verrucae, seen at review appointment, demonstrated full treatment success, partial success or no improvement. Treatment compliance was evaluated based on following 4 therapeutic recommendations given at baseline. Full success group compliance was 100%, partial success compliance was 75% and no success group compliance was under 50%.
Conclusions: Preliminary conclusions from the research conducted show that by improving compliance physicians may also improve the outcome of treatment. Employing simple measures that can improve compliance can reduce the need for further treatments or the need for introducing more aggressive meds. Physician patient relationship should be therefore focused on mutual understanding and physicians should try to convince their patients that adherence to treatment plays equally important role as being prescribed correct meds.
Key words: Compliance; Treatment Outcomes; Adherence To Recommendations; Therapeutic Protocol; Physician-Patient Relationship
INTRODUCTION
Compliance is defined as the degree or extent of conformity to the recommendations about day-to-day treatment by the provider with respect to the timing, dosage, and frequency. In order for a physician to be successful at treating a patient three conditions must be met: correct diagnosis, adequate treatment decisions and patients compliance. Diagnosis and treatment choice are primarily dependent on physicians experience and knowledge; however, a patient’s adherence to treatment recommendations is mainly up to the patient’s motivation and the quality of physician-patient relationship [1].
It has to be stressed that a patient’s nonadherence can be extremely dangerous and potentially life-threatening. Patients may sustain significant risks by misunderstanding, ignoring or forgetting the health provider’s recommendations.
According to research, around 40% of patients fail to adhere to their treatment regimens and that figure depends on the complexity of the treatment regime [2].
Compliance drops significantly when therapeutic regimens become more complex and affect patients’ lifestyles, as depicted by Chasney in his article on HIV patients on complex regimes like HAART [3].
The treating physician should encourage his/her patients to adhere to his treatment plan and try to make it as clear and simple to the patients as possible. Patients’ compliance often seems to be the weakest link in the therapeutic process [4,5]. The aim of this study is to determine if treatment success depends on the patient’s compliance and if so how significant is this relationship.
MATERIALS AND METHODS
Patients’ adherence to three therapeutic regimes for acne, scalp psoriasis and plantar verruca have been analysed. Patients with diagnosis of facial acne, scalp psoriasis or plantar verrucae have been identified and treated by the author at his dermatology outpatient clinic in Ostrowiec, using the same therapeutic regime, depending on their diagnosis between January 2020 – November 2021. Detailed treatment plans had been explained and provided in writing for each patient. Each patient from the various cohorts received exactly the same treatment recommendations with regards to timing, dosage and frequency of application. The ordered treatment was considered by the treating physician as the treatment of choice. Patients or patients’ caregivers were also offered alternative treatment options, including an option to not treat at all. Patients who eventually started on the same treatment regime were considered for the purpose of this paper.
Before leaving the consultation room, patients were also asked to confirm if the treatment protocol was entirely clear to them and to verify that, they were asked to explain how they were going to apply meds. Treatment for acne consisted of lymecycline 300 mg oral tablet (brand name tetralysal) daily for 12 weeks. Treatment for scalp psoriasis included topical clobetasol propionate solution once daily to affected areas on scalp until resolution. 50ml of solution was prescribed (brand name Dermovate solution). Treatment for plantar verrucae involved paring down of lesions, topical fluorouracil and salicylic acid (brand name verrumal) followed by occlusion with duct-tape and pressure relief insoles. Maximum treatment duration of 6 weeks or until resolution of lesions. 12 patients were treated in each group.
Facial acne cohort-patients were reviewed at week 12 and were asked to bring all their meds and remaining tablets for the follow-up visit. Remaining tablets were counted. Acne severity was assessed at first visit and at follow-up using simple 0-3 staging (0-no acne, 1-mild acne, 2-moderate acne, 3- severe acne). Each patient was prescribed a total of 96 tablets for his acne and the percentage of tablets actually taken (compliance) was calculated at follow-up by comparing the total number of prescribed tablets with the number of remaining tablets. Each patient’s change in acne score was assessed by comparing his acne score at baseline and follow-up.
Scalp psoriasis patients were reviewed at week 2 and were asked to bring the remaining meds for the appointment. The amount of solution used was assessed by weighing a full 50ml bottle at baseline and the same bottle at week 2. Laboratory pharmaceutical scales were used for measurements. Scalp psoriasis intensity was assessed by treating clinician by employing simple 0-3 staging (0-no scalp psoriasis, 1-mild, 2-moderate, 3-severe scalp psoriasis). Patients were asked if they had applied treatment by themselves or had asked for help. Each patient’s change in scalp psoriasis score was assessed by comparing his scalp psoriasis score at baseline and at follow-up.
Patients with plantar verrucae were reviewed at week 6 and each patient was asked to describe in detail his daily treatment routine. Following treatment steps were checked:
- topical formula application,
- Occlusive dressing,
- Paring down,
- Pressure relief insoles.
Each patient was assessed for his compliance: if 4 steps were undertaken = 100% compliance, 3 steps=75% compliance, 2=50% and 1=25% compliance.
Patients were also grouped into 3 subsets based on treatment success: treatment success with no warts; partial success with less warts; no success with no change in warts number.
RESULTS
Facial Acne Patients
Number of patients: 12, aged 13-19, mean age 16.
Average acne severity at baseline: 2.42 (5 patients with severe acne-score 3 and 7 patients with moderate acne score 2).
Average acne severity at follow-up: 1.34 (6 patients with moderate acne – score 2, 4 patients with mild acne-score 1, 2 patients with no acne-score 0).
Average compliance: 85.56%. (11 patients have returned unused tablets; patient 1: 4 tablets left, 2 -23, 3-30, 4-8, 5-24, 6-6, 7-5, 8-7, 9-11, 10-22, 11-26). Patient 12 claimed to have unintentionally disposed of unused tablets. His compliance was not assessed.
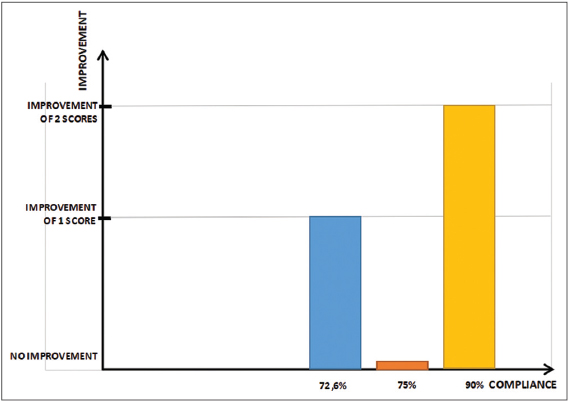
Acne severity change association with level of compliance:
Change of 2 scores: 7 patients (average compliance of these patients: 90%)
Change of 1 score: 4 patients (average compliance of these patients: 72.6%-based on figures available for 3 patients; one has lost his unused tablets).
No change in acne score: 0 (compliance 75%); (Fig. 1).
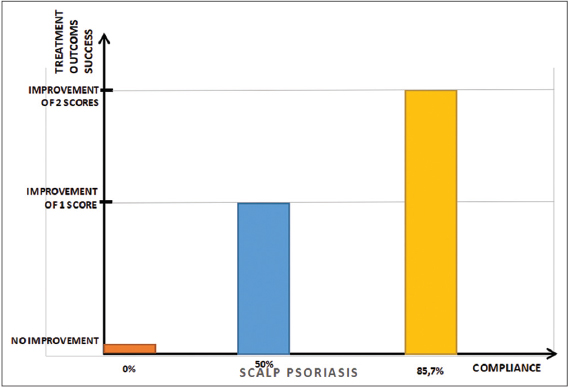
Scalp Psoriasis Patients
Number of patients: 12, aged 18-55, mean age: 31.8
Average scalp psoriasis severity at baseline: 2.59
Average scalp psoriasis severity at follow-up at week 2: 1.1
Change of 2 scores: 7 patients (applied treatment on their own vs with help 1vs6; average use of 38ml per patient-compliance=85.7%
Change of 1 score: 4 patients (applied treatment on their own vs with help 2vs2; average use of 40ml per patient-compliance=50%
No change of score: 1 patient (applied treatment on his own, used 30ml-compliance=0% (Fig. 2).
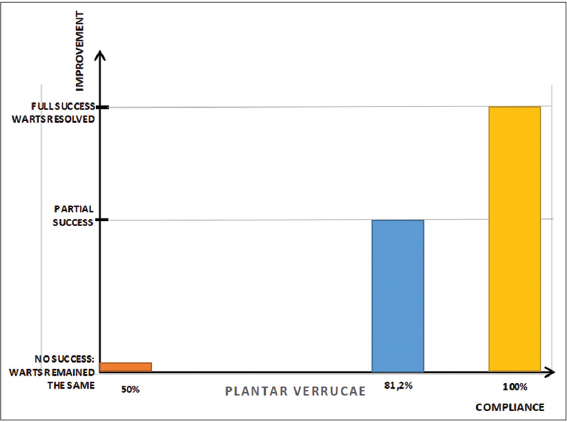
Plantar Verrucae Patients
Number of patients: 12, aged: 6-13, mean age: 10.1
Full treatment success (no warts remaining): 5; compliance in this group=100%
Partial treatment success (less warts than at baseline): 4, mean compliance in this group=81.25%
No success (no change in warts number since baseline): 3, mean compliance=50% (Fig. 3).
Patients compliant with 4 treatment recommendations (topical formula application, occlusive dressing, paring down and pressure relief insoles): 6. 5 patients of these 6 achieved full success and all warts had resolved.
Patients compliant with 3 treatment recommendations: 4. Three patients in this group and 1 from group of patients who were compliant with all 4 recommendations achieved partial success and some lesions had resolved.
Patients compliant with 2 or less treatment recommendations: neither of these two patients, nor one patient compliant with 3 recommendations had any success and warts had remained the same at week 6.
DISCUSSION
There are several studies studying compliance however there are no standardised methods of how to measure it [1,4,6,7–13]. Literature on compliance in dermatology is sparse as dermatology treatment protocols often entail tablets, capsules, injections but also creams, lotions, ointments and very specific application modalities. Complexity of dermatology treatment regimes makes compliance in dermatology difficult to capture [1]. This article reviews different dermatology treatment plans for three dermatological conditions and the author analyses patients adherence to these plans in order to prove if there is any association between compliance and treatment success. The author has identified several limitations while undertaking this research. In facial acne patients the remaining unused tablets count only partially reflects compliance. Patient home diaries should be implemented in which patients would report days when tablet was taken and days when not [14–16]. Such an approach would allow collation of more data, to better understand the level of compliance during different stages of treatment. Additional questions could then be answered, for example do patients tend to be more compliant with the duration of the study or closer to follow-up appointments. Other limitations include the fact that compliance verification in scalp psoriasis and plantar verrucae patients is based on patients’ declarations.
Results of this research demonstrate that treatment outcomes are positively correlated with adherence. Furthermore it has been indicated that the modes of application of topical treatments and third party support also affect treatment outcomes, which is an important finding because physicians tend to pay less attention to such seemingly minor and obvious issues like how exactly to achieve verrucae pressure relief or suggesting third party engagement in applying solution to hard-to-reach areas of scalp etc. Patients’ treatments analysed in this paper were explained in detail with extreme diligence, at a level not normally practised during outpatient consultations. Significantly lower patients compliance should then be expected when consultations take place in busy clinics with limited time for consultation and overbooking of patients. In view of these findings physicians often need to step back and confirm a patient’s compliance when ordered treatments are not successful before embarking on a new therapeutic plan.
According to previous research on compliance there is no single strategy to improve compliance in all patients however a set of key factors have been agreed upon [1,17]. According to Leslie R Martin et al: “These include realistic assessment of patients’ knowledge and understanding of the regimen, clear and effective communication between health professionals and their patients, and the nurturance of trust in the therapeutic relationship” [2]. These factors are mainly physician dependent and suggest that physicians who regularly see their patients and manage to build a good relationship with their patients achieve treatment success more often than those who only rarely see their patients [6,18,19].
Timing of appointments also may play a role in enhancing compliance. Elizabeth Heaton et al. in her work has reviewed literature to assess if timing of appointments can improve adherence. They identified 15 studies on compliance and 13 of these studies demonstrated positive correlations between adherence and clinic appointments. Additionally 3 of these studies demonstrated increased adherence with increased appointments frequency [20,21]. Such correlation would suggest that physicians might consider arranging follow-up appointments sooner to improve compliance. However, more appointments means higher healthcare costs. Telephone follow-up contacts or review appointments conducted by assistant physicians could lower these costs.
According to a clinical trial performed by doctor Steven R Feldman and his team, looking at the impact of office visits on patients adherence to topical psoriasis treatment, adherence rates were significantly higher around the time of office visits. Electronic monitors were used to measure adherence. The author concluded that arranging a follow-up visit shortly after initiating treatment may be an effective tool to upsurge the use of patients’ topical meds and achieve optimal treatment outcomes. If adherence to prescribed topical treatment can be improved, exposure to more costly and aggressive systemic agents may be avoidable [22].
Moreover physicians should seek ways to improve compliance during treatment. Examples of such compliance enhancing methods might include easily accessible youtube educational videos clearly demonstrating how to apply prescribed meds; apps sending reminders to take a pill; storing prescription meds next to the toothbrush or toiletries, which make them less likely to be forgotten etc. [13,23,24].
Further thorough clinical studies should be designed and conducted to better understand the level of compliance among dermatology patients. Funding for such studies may be difficult to obtain as pharmaceutical companies are more interested in inventing new therapeutic agents rather than looking at compliance to existing medicines. Well designed study may entail hidden bottle opening sensors which are activated each time a patient opens them, thus allowing the physician to assume that a tablet/capsule had been taken. Such state of the art devices are already available, for example MEMS-medication event monitoring system which uses a hidden microchip mechanism that records the time and date that a patient opens a pill box, removes a pill from a pack, actuates an inhaler, or dispenses an eye drop [20].
Other measures to collect credible compliance data may include patients’ home diaries, family members reports, electronic monitors, biological markers, pharmacy records or asking the patient to demonstrate his daily treatment routine [12]. Improving adherence to treatment seems to be the cheapest and quickest way to improve treatment outcomes. Healthcare cost-benefit studies focusing on the level of patient compliance impact on treatment success should be undertaken to prove this thesis.
Acknowledgements
The would like to acknowledge his assistant nurse and patient registration clerk who have helped in collecting and analysing the data for the purpose of this paper.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Eicher L, Knop M, Aszodi N, Senner S, French LE, Wollenberg A. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease – strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33:2253-63.
2. Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189-99.
3. Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17:169-77.
4. LindsøAndersen P, Jemec GB, Saunte DML. Treatment adherence and psychosocial impact of tinea capitis in families:Qualitative pilot study. Dermatol Ther. 2020;33:e13570.
5. Vakirlis E, Bakirtzi K, Papadimitriou I, Vrani F, Sideris N, Lallas A, et al. Treatment adherence in psoriatic patients during COVID-19 pandemic:Real-world data from a tertiary hospital in Greece. J Eur Acad Dermatol Venereol. 2020;34):e673-5.
6. Neri L, Peris K, Longo C, Calvieri S, Frascione P, Parodi A, et al;Actinic Keratosis – TReatment Adherence INitiative (AK-TRAIN) study group. Physician-patient communication and patient-reported outcomes in the actinic keratosis treatment adherence initiative (AK-TRAIN):a multicenter, prospective, real-life study of treatment satisfaction, quality of life and adherence to topical field-directed therapy for the treatment of actinic keratosis in Italy. J Eur Acad Dermatol Venereol. 2019;33:93-107.
7. Millán-Cayetano JF, Del Boz J, García-Montero P, García-Harana C, Rivas Ruiz F, de Troya-Martín M. Survival study of treatment adherence by patients given oral oxibutynin for hyperhidrosis. J Eur Acad Dermatol Venereol. 2018;32:1034-7.
8. Del Boz J, García-Souto F, Rivas-Ruiz F, Polo-Padillo J. Survival study of treatment adherence by patients given oral glycopyrrolate for hyperhidrosis following treatment failure with oral oxybutynin. Dermatol Ther. 2020;33:e14210.
9. De Las Cuevas C, Betancort M, de Leon J. The necessity-concern framework in the assessment of treatment adherence of psychiatric patients and the role of polypharmacy in a Spanish sample. Hum Psychopharmacol. 2020;35:e2721.
10. Reich A, StępieńK, Krasowska D, Osmola-Mańkowska A, Owczarek W, Szepietowski J. Assessment of satisfaction, compliance with medical recommendations and quality of life on the basis on the observational, non-interventional, multi-center study to evaluate the efficacy of the therapeutic process with DaivobetŽgel in the treatment of psoriasis as a part of routine medical practice. Dermatology Review. 2020;107:199-209.
11. Di Bona D, MagistàS, Masciopinto L, Lovecchio A, Loiodice R, Bilancia M, et al;AIT Study Group. Safety and treatment compliance of subcutaneous immunotherapy:A 30-year retrospective study. Respir Med. 2020;161:105843.
12. Hascicek AM, Kilinc MF, Yildiz Y, Yuceturk CN, Doluoglu OG. A new checklist method enhances treatment compliance and response of behavioural therapy for primary monosymptomatic nocturnal enuresis:a prospective randomised controlled trial. World J Urol. 2019;37:1181-7.
13. Al-Rubaey MG, Shwaish MI. Impact of hypertension education on treatment compliance among hypertensive patients in Baghdad 2017. J Pak Med Assoc. 2019;69(Suppl 3)(8):S9-S12.
14. Sakr S, Hachem D, Ghaddar A, Taha N. Assessment of knowledge, attitude, and practice toward acne vulgaris among the Lebanese young adult population. Our Dermatol Online. 2020;11:e169.1-6.
15. Marahatta S, Shrestha U. Hospital prevalence and causes of non-adherence to acne treatment:A report from Nepal. Our Dermatol Online. 2021;12:251-6.
16. Kawshar T, Rajesh J. Sociodemographic factors and their association to prevalence of skin diseases among adolescents. Our Dermatol Online. 2013;4:281-6.
17. Rout SK, Gabhale YR, Dutta A, Balakrishnan S, Lala MM, Setia MS, et al. Can telemedicine initiative be an effective intervention strategy for improving treatment compliance for pediatric HIV patients:Evidences on costs and improvement in treatment compliance from Maharashtra, India. PLoS One. 2019;14:e0223303.
18. Broniarczyk-Dyła G, Pajor A, Nowe spojrzenie na współpracępacjenta z lekarzem w chorobach przewlekłych skóry (New insight into medication adherence in chronic skin diseases). Pol Merkuriusz Lek. 2012:33:378-81.
19. Kraepelien M, Blom K, Lindefors N, Johansson R, Kaldo V. The effects of component-specific treatment compliance in individually tailored internet-based treatment. Clin Psychol Psychother. 2019;26:298-308.
20. Farmer KC. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clin Ther. 1999;21:1074-90;discussion 1073.
21. Heaton E, Levender MM, Feldman SR. Timing of office visits can be a powerful tool to improve adherence in the treatment of dermatologic conditions. J Dermatolog Treat. 2013;24:82-8.
22. Feldman SR, Camacho FT, Krejci-Manwaring J, Carroll CL, Balkrishnan R. Adherence to topical therapy increases around the time of office visits. J Am Acad Dermatol. 2007;57:81-3.
23. Gupta M. A study of knowledge, attitude and practices regarding hair dye use among general population. Our Dermatol Online. 2017;9:15-8.
24. Gupta M. Assessment of knowledge, attitudes and practices about sun exposure and sunscreen usage in outpatients attending a Dermatology Clinic in North India. Our Dermatol Online. 2018;10:34-7.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.