New dermoscopic description of lichenoid keratosis
Aida Oulehri 1, Zakia Douhi1, Hanane Baybay1, Sara Elloudi1, Fatima Zahra Mernissi1, Imane Gouzi2, Layla Tahiri2,3, Hinde El Fatemi2,3
1, Zakia Douhi1, Hanane Baybay1, Sara Elloudi1, Fatima Zahra Mernissi1, Imane Gouzi2, Layla Tahiri2,3, Hinde El Fatemi2,3
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco, 2Departement of Pathological Anatomy, University Hospital Hassan II, Fez, Morocco, 3Biomedical and Translational Research Laboratory, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez, Morocco
Corresponding author: Aida Oulehri, MD
How to cite this article: Oulehri A, Douhi Z, Baybay H, Elloudi S, Mernissi FZ, Gouzi I, Tahiri L, El Fatemi H. New dermoscopic description of lichenoid keratosis. Our Dermatol Online. 2022;13(e):e22.
Submission: 02.03.2021; Acceptance: 16.06.2021
DOI: 10.7241/ourd.2022e.22
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Lichenoid keratosis (LK)—also known as lichen planus-like keratosis, solitary lichen planus, or involuting lichenoid plaque—is a common benign cutaneous lesion [1]. LK is found to represent 1.6% of all skin biopsies reviewed by dermatopathologists [2]. It usually affects adults older than 55 years of age and is more prevalent among females. Although the etiology of LK is not fully understood, LK usually develops over a preexisting skin lesion, such as a solar lentigo lesion or seborrheic keratosis, which might be evident upon examination [3]. LK may appear anywhere on the body but is most commonly seen on the trunk and the upper extremities. It is frequently present as a single lesion [2]. LK may be categorized clinically into six different types: flat pigmented, flat erythematous, plaque-like, papulokeratotic, nodular, and morpheaform. LK may be difficult to differentiate from melanoma and non-melanoma skin cancer, both clinically and dermoscopically.
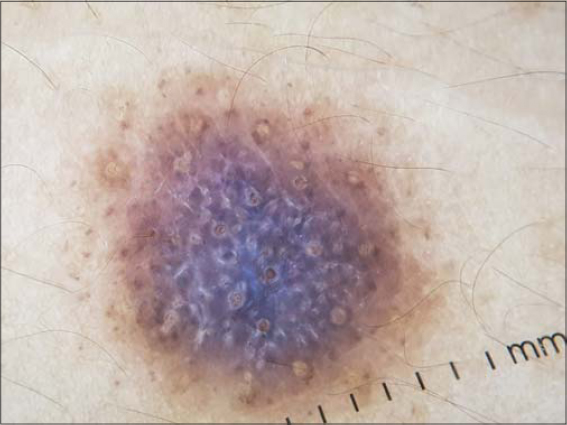
Histologically, LK mimics lichen planus, that is, band-like inflammatory infiltrate with interface involvement, vacuolar degeneration of the basal cell layer, hyperparakeratosis, acanthosis, and the presence of dermal melanophages. Dermoscopy of LK bears no pathognomonic features. Comedo-like openings, a cerebriform appearance, telangiectasias, dotted vessels and bluish-grey granules (peppering), milky red-white areas, spoke-wheel areas, short pigmented lines, eccentric or central hyperpigmentation, blue ovoid nests, and white scar-like areas may be observed in LK [3].
Herein, we report the case of a thirty-year-old female without a medical history who consulted for a solitary, intensely itchy lesion on the upper back (Fig. 1). The patient reported that the lesion had been present for four months. No previous skin lesions had been noted by the patient in the same site. The lesion had been stable in size, color, and shape. A physical examination revealed a solitary, thin, violaceous plaque 2 cm in size. Scalp, mucosa, and nail examinations were normal. The dermoscopic features of the lesion included regular, light-brown, eccentric dots and globules, a central blue-white veil taking two thirds of the lesion, comedo-like openings, subtle gray circles, short and thin bright white linear structures, and no vascular pattern (Fig. 2). A biopsy of the lesion was taken, revealing para- and orthokeratotic hyperkeratosis with interface lymphohistiocytic infiltrate and vacuolar degeneration of the basal cell layer (Fig. 3), confirming the diagnosis of lichenoid keratosis.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Gori A, Oranges T, Janowska A, Savarese I, Chiarugi A, Nardini P, et al. Clinical and dermoscopic features of lichenoid keratosis:A retrospective case study. J Cutan Med Surg. 2018;22:561-6.
2. Vincek V. Lichen planus-like keratosis:Clinicopathological evaluation of 1366 cases. Int J Dermatol. 2019;58:830-3.
3. BinJadeed H, Aljomah N, Alsubait N, Alsaif F, AlHumidi A. Lichenoid keratosis successfully treated with topical imiquimod. JAAD Case Rep. 2020;6:1353-5.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |





Comments are closed.