Vulvar vestibular papillomatosis: All genital lesions are not sexually transmitted diseases
Deeptara Pathak Thapa
Nepal Medical College and Teaching Hospital, Department of Dermatology, Kathmandu, Nepal
Corresponding author: Deeptara Pathak Thapa, MD
How to cite this article: Thapa DP. Vulvar vestibular papillomatosis: All genital lesions are not sexually transmitted diseases. Our Dermatol Online. 2021;12(e):e43.
Submission: 24.02.2021; Acceptance: 23.04.2021
DOI: 10.7241/ourd.2021e.43
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Vulvar vestibular papillomatosis (VVP) is considered as normal anatomical variant of the vulva. A 19-year-old female presented with asymptomatic pinkish filliform papules symmetrically distributed on vulva. She denied having any sexual exposure. Clinical differential diagnosis included genital wart and vestibular papillomatosis, however biopsy was consistent with Vestibular papillomatosis. PAS stain was negative. Application of 5% acetic acid did not show any change in color. We report this case to create awareness about normal variant of vulva and unnecessary exaggerated treatment and proper counseling of patient to decrease psychological trauma and associated venereophobia.
Key words: Histopathology; human papilloma virus; Vulva
INTRODUCTION
Vulvar vestibular papillomatosis (VVP) is known to be a normal anatomical variant of the vulva [1]. It was first described by Altmeyer in 1981 as pseudocondylomata of the vulva. In the past there are studies which quoted rare association of VVP with human papilloma virus but recently studies have found no relation of HPV with VVP [2,3]. Prevalence rates range from 1% to 33% [4].
Vulvar Vestibular papillomatosis (VVP) are considered the female equivalent of pearly penile papules [5]. VVP have been called with different names in the literature, such as hirsutoid papiloma of vulva, vulvar squamous papillomatosis, micropapillomatosis labialis and squamous vestibular micropapilloma [6]. HPV had been thought to be the etiological agent of VVP in the past but diagnostic techniques with PCR and in situ hybridization revealed no association with HPV [3,7,8].
Clinically, lesions of vestibular papillomatosis are symmetrical and have linear array in distribution, soft pink as adjacent mucosa, bases of which remain separated with no circumscribed whitening on applying 5% acetic acid. While Genital warts are irregular, hard, flesh colored to pink and greyish with projections can coalesce in common base [6,7,9].
VVP is considered by few authors as an asymptomatic clinical entity. In few patients, however premonitory vulvar vestibular pruritus, pain or burning and dyspareunia were observed [5]. According to Growdon et al. patients with VVP can be divided into two groups as asymptomatic patients and those with symptoms like vulvar pruritus, burning and dyspareunia.[10] On the basis of diagnostic tool like histological and in situ hybridization data, they proposed that symptomatic VP was HPV-induced and asymptomatic VP a variant of normal mucosa [5].
CASE REPORT
A 19-year-old female presented with filiform genital lesions which she noticed over the last 2 years. Patient denied having any sexual exposure in the past. On clinical local examination there were multiple filiform papules of sizes 1 to 2mm on the labia minora; more over vestibule but symmetrically distributed. The papules were pinkish in colour resembling colour of the labia minora as shown in Figure 1. Acetic acid 5% was spread on the lesions but there was no change of any color. Laboratory investigation to rule out other sexually transmitted diseases, like HIV serology, VDRL, TPHA, Hepatitis B, C were all found to be negative. Biopsy was performed. The histopathology revealed acanthotic epidermis with multiple vacuolated cells with round to oval nuclei with irregular nuclear contours in areas, visible nucleoli and abundant cytoplasm in epidermis as shown in Figure 2. To differentiate it being glycogen or koilocytes, PAS stain was done which was found to be negative. Biopsy report was suggestive of Vestibular papillomatosis with recommendation to do further PCR for Human papilloma virus (HPV).
 |
Figure 1: Multiple filliform papules symmetrically seen on labia minora. |
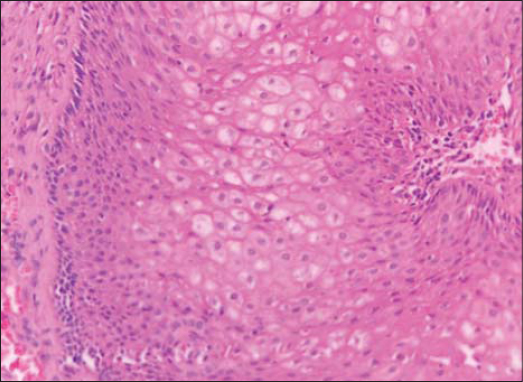 |
Figure 2: Multiple vacuolated cells with prominent nucleoli with abundant cytoplasm seen in the epidermis. |
Patient denied for PCR for HPV or IHA for HPV due to financial constraints. Patient was counselled for the disease and no further treatment was done. She was advised for regular follow-up.
CONCLUSION
Awareness about VVP as a normal anatomical variant among dermatologists and gynecologists is warranted to avoid any unnecessary exaggerated treatment in the form of topical or surgical modality should be avoided. Proper counseling of patient should be done to decrease psychological trauma and venereophobia associated with this condition.
ACKNOWLEDGEMENTS
Dr Moushami Singh, M.D (Pathology) Nepal Cancer Hospital and Research Centre
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Welch JM, Nayagam M, Parry G, Das R, Campbell M, Whatley J, et al. What is vestibular papillomatosis?A study of its prevalence, aetiology and natural history. Br J Obstet Gynaecol. 1993;100:939-42.
2. Gozales JMD, Luna EM, Romero AP, Hemandez AM, Cherit JD. Vestibular papillomatosis as a normal vulvar anatomical conddition. Dermatol Online J. 2013;19:20032.
3. Beznos G, Coates V, Focchi J, Hatim AO. Biomolecular study of the correlation between papillomatosis of the vulvar vestibule in adolescents and human papillomavirus. Scien World J. 2006;6:628-36.
4. Wollina U, Verma S. Vulvar vestibular papillomatosis. Indian J Dermatol Venereol Leprol. 2010;76:270-2.
5. Sarifakioglu E, Erdal E, Gunduz C. Vestibular pappilomatosis:acse report and lierature reveiw. Acta Derm Venereol. 2006;86:177-8.
6. Orgun A, Dogru HY. Vestibular pappilomatosis mimicking genital warts in a pregnant women. Turkerm-Turk Arch Dermatol Venerol. 2019;53:122-4.
7. Moyal-Barracco M, Leibowitch M, Orth G. Vestibular papillae of the vulva. Lack of evidence for human papillomavirus etiology. Arch Dermatol. 1990;126:1594-8.
8. Kakkar S, Sharma PK. Benign vulvar vestibular papillomatosis:An underreported condition in Indian dermatological literature. Indian Dermatol Online J. 2017;8:63-5.
9. El Kadiri S, Bay Bay H, Chaoui R, Douhi Z, Elloudi S, Mernissi FZ. Two soulmates !!!Our Dermatol Online. 2020;11(e):e55.1-e55.2.
10. Growdon WA, Fu YS, Lebherz TB, Rapkin A, Mason GD, ParksG. Pruritic vulvar squamous papillomatosis:evidence for human papillomavirus etiology. Obstet Gynecol. 1985;66:564–8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-1602-415X http://orcid.org/0000-0002-1602-415X |



Comments are closed.