New leprosy cases at the Macompo Center in the Dubréka Health District (Guinea)
Moussa Keita 1, Soumah Mohamed Maciré1, Tounkara Thierno Mamadou1, Diané Boh Fanta1, Sako Fodé Bangaly2, Bangoura Mmah Aminata3, Keita Abdoulaye4, Traoré Fodé Amara2, Keita Moussa5, Kaba Mohamed Soufouyane6, Baldé Houleymatou1, Cissé Mohamed1
1, Soumah Mohamed Maciré1, Tounkara Thierno Mamadou1, Diané Boh Fanta1, Sako Fodé Bangaly2, Bangoura Mmah Aminata3, Keita Abdoulaye4, Traoré Fodé Amara2, Keita Moussa5, Kaba Mohamed Soufouyane6, Baldé Houleymatou1, Cissé Mohamed1
1Department of Dermatology-STD, Conakry University Hospital, University Gamal Abdel Nasser of Conakry, Conakry, Guinea, 2Department of Infectious Diseases, Conakry University Hospital, University Gamal Abdel Nasser of Conakry, Conakry, Guinea, 3Department of Pediatry, Conakry University Hospital, University Gamal Abdel Nasser of Conakry, Conakry, Guinea, 4ENT Service and Head and Neck Surgery, Conakry University Hospital, University Gamal Abdel Nasser of Conakry, Conakry, Guinea, 5Macompo Center for Antiseptics, National Leprosy Program, Ministry of Health, Guinea, 6Madina Dispensary, National Leprosy Program, Ministry of Health, Guinea
Corresponding author: Dr. Moussa Keita
How to cite this article: Keita M, Soumah MM, Tounkara TM, Diané BF, Sako FB, Bangoura MA, Keita A, Traoré FA, Keita M, Kaba MS, Baldé H, Cissé M. New leprosy cases at the Macompo Center in the Dubréka Health District (Guinea). Our Dermatol Online. 2021;12(e):e3.
Submission: 06.04.2020; Acceptance: 05.04.2021
DOI: 10.7241/ourd.2021e.3.
Citation tools:
Copyright information
© Our Dermatology Online 2021. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The objectives of this study were to determine the detection rate of new cases of leprosy and to describe the demographic and clinical profiles of the patients in the Macompo Center.
Material and Methods: This was a cross-sectional, retrospective study of a descriptive type carried out in two periods: from January 2000 to December 2002 and from January 2011 to December 2014 based on leprosy records recorded at the Macompo center in Dubréka. All the files with diagnosis of new cases of leprosy have been included.
Results: The prevalence of leprosy varied from one year to the next with a peak of 6 cases in 2000, or 0.04 per 10000 inhabitants, decreasing to 2 cases, or 0.01 per 10000 inhabitants in 2014. In seven years only 22 new cases of leprosy have been detected out of a total of 135 patients with an average detection rate of 0.98 per 10000 inhabitants. The largest number of cases was detected in the rural areas (50%). The average age of our patients was 32 years with extremes of 6 and 65 years. There was a peak in the age group of 27 to 37 years, or 36.4%. The prevalence in children accounted for 13% of cases. The sex ratio was 0.83. Of all new cases reported, 72.7% were multi-bacillary.
Conclusion: This study confirms the elimination of leprosy in Guinea. However, the epidemiological surveillance of this disease, especially at the level of the children population, should always be strengthened.
Key words: New case; Leprosy; Detection; Dubreka; Guinea
INTRODUCTION
Leprosy continues to be endemic in some areas of developing countries despite the organization of control in these areas. This control is characterized by the active (and passive) detection of cases and the introduction of multidrug therapy (MDT), which is distributed free of charge to patients suffering from leprosy [1]. Despite global disease control programs, leprosy remains the second most common mycobacterial disease in the world after tuberculosis, with 21 388 new cases in 2014, compared to 215 656 new cases in 2013 [2]. The elimination of the disease as a public health problem in 2005, when the prevalence was expected to be less than 1 case per 10000 population, was not achieved; even though the global prevalence rate has decreased from 8.4 cases per 10000 inhabitants in 1966 to less than 1 case per 10000 inhabitants at the end of 2000, thanks to the poly-chemotherapy (PCT) instituted since 1981, which has constituted a major turning point in the fight against leprosy and has enabled 16 million leprosy patients to be cured in the last 20 years [1,2]. Guinea, according to the report of the National Leprosy Control Program, has reached the WHO elimination threshold for leprosy, with a prevalence rate going from 12 cases per 10000 in 1990 to 0.58 cases for 10000 inhabitants at the end of 2008 [2]. The objectives of this study were to determine the detection rate of new cases of leprosy and to describe the demographic and paraclinical profiles of the patients in the Macompo Center in Dubreka Health District.
MATERIAL AND METHODS
The study was conducted in the Leprosy Center of Macompo (Leprosy in the local Baga language) located in Dubréka District Health. This District is 42 km from the capital city Conakry and covers an area of 5500 km2. Its population is estimated at 223 774 inhabitants divided between the urban commune and the six sub-district (Tondon, Khorira, Faléssadé, Wassou, Baady and Tanènè). It is also a center for the management of tuberculosis, trypanosomiasis and onchocerciasis. This was a cross-sectional, retrospective study carried out in two periods from January 2000 to December 2002 and from January 2011 to December 2014. It concerned the records of leprosy patients registered in the center. All the files with diagnosis of new cases of leprosy have been included. The data were collected using a survey form. The variables studied were prevalence per year, detection rate, demographic variables (age, sex, occupation, geographical origin), forms of leprosy, degree of disability according to WHO and the bacillary index. A new case of leprosy was considered to be any case diagnosed clinically or on the basis of a smear but not yet started on MDT. The detection rate corresponding to the total number of new cases of leprosy detected during the year compared to that of the total population expressed in rates per 10000 inhabitants.
RESULT
The prevalence of leprosy varied from year to year with 6 cases in 2000, or 0.04 per 10000 inhabitants and 2 cases in 2014, or 0.01 per 10000 inhabitants. In 7 years, only 22 new leprosy cases were detected out of a total of 135 patients detected with an average detection rate of 0.98 per 10000 inhabitants. This annual detection rate was always less than 1 case / 10000, ranging from 0.27 cases per 10000 inhabitants in 2000 to 0.09 cases per 10000 inhabitants in 2014. The year 2011 recorded the lowest detection rate with a single notified case. The prevalence and detection rate are shown in Fig. 1. The largest number of cases was detected in rural areas (50%) of the health district. The average age of our patients was 32 years with extremes of 6 and 65 years. There was a peak in the age group of 27 to 37 years, 36.4%. The proportion of children affected accounted for 13% of cases; 14% of patients had a family history of leprosy. The study population was predominantly young and female (55%) with a sex ratio of 0.83. Housewives (36%) and farmers (23%) were the most represented socio-professional groups. Of all new cases reported, 73% were multi-bacillary leprosy and 27% were paucibacillary with 18.25% grade 2 disease. Smear tests performed on nasal mucus samples and lobes ears was positive in all multibacillary patients.
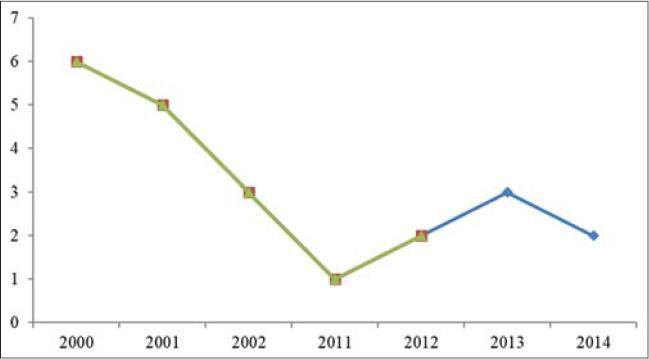 |
Figure 1: Annual evolution of new cases of leprosy between 2000-2002 and 2010-2014. |
DISCUSSION
The analysis of the reports of new cases of leprosy in Dubreka health district in Guinea shows a marked decline in leprosy with a prevalence rate going from 6 cases in 2000, or 0.04 per 10,000 inhabitants to 2 cases in 2014 or 0.01 per 10,000 inhabitants. The reduction in the prevalence rate of less than 1 case per 10,000 inhabitants indicates the elimination of leprosy as a public health problem according to the WHO definition or a decrease in leprosy screening activities in the center. According to the WHO criteria, leprosy has been eliminated from Guinea since 2010 [2]. The same observation was made by M Seydi [3] in Senegal in 2002, where the prevalence rate was 0.99 per 10,000 inhabitants with an average detection rate of 5 cases per 10,000 inhabitants and by Keita M et al. [4] who reported a decrease in the detection rate of new cases of leprosy in 2013 in the city of Conakry with 0.15 cases / 10,000 inhabitants. On the other hand, J Raslan et al [5] report a prevalence rate of 3.70 / 10,000 and a detection rate of 1.8 / 10,000 in Mayotte between 2006 and 2011; and Kofi S et al. [6] a high prevalence rate of 6.99 cases per 10,000 inhabitants in 2007 in south western Burkina Faso. The average age of our patients was close to that of the series of Keita et al [7] in Mali (33.8 ± 16.7 years). Chisi et al [8] reported that leprosy affects young populations. In our study 89.11% of patients were between 15 and 47 years of age. The proportion of children is considered an indicator of transmission of the disease. The rate of children (13%) in our study was close to that of Saka et al [9] in Togo and Koffi M et al [10] in Côte d’Ivoire. Seven years after the elimination of leprosy in Senegal, Seydi et al [3] reported a childhood rate of 14%. In general, leprosy affects men more than women, our study appears to invalidate this classic trend with a sex ratio of 0.8 in favour of women. According to WHO criteria, leprosy has been eliminated from Guinea since 2010 [1]. However, Phaff et al. [11] in Mozambique found three times in a row that detection was higher in the years of “elimination campaigns” than in traditional screening years. Moreover, in our study, prevalence of multibacillary leprosy among new cases was significantly elevated, with 73% of cases. In Senegal, where leprosy is no longer a priority public health problem, Seydi et al [3] also observed a predominance of multibacillary leprosy. Other studies [12,13] have also suggested a certain predominance of multibacillary forms in relation to a decrease in prevalence. Indeed, the proportion of paucibacillary leprosy would reflect the intensity of contacts with leprosy in the population; with the reduction in the number of cases and therefore contacts, only the very receptive subjects would be able to contract the disease and to make serious forms. Leprosy is an important cause of physical disability in countries where it is endemic. These disabilities are partly the consequence of the disabilities and nervous damage caused by leprosy reactions when they are not treated very early. Our degree 2 of 18.25% disability rate was higher than that reported by De Carsalade et al [14] in Mayotte. Smear examination is not necessary for the diagnosis of leprosy, however, its interest lies in the confirmation of non-obvious multibacillary forms and the suspicion of relapse cases [1,15]. In our study smear was strongly positive in all multibacillary patients whereas it was less positive in paucibacillary patients.
CONCLUSION
The encouraging results currently achieved should not diminish the activities of the national leprosy control program in order to eradicate this disease. Epidemiological surveillance should be strengthened, especially at the level of the children population.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Organisation Mondiale de la Santé. La dernière ligne droite vers l’élimination de la lèpre. Plan stratégique 2000-2005;WHO/CDS/CPE/CEE/2001.
2. Programme National de Lutte contre la lèpre en Guinée. Rapport de synthèse 2010.
3. Seydi M, ManéI, SoumaréM, Faye O, Badiane C, Coly SL, et al. Évaluation de l’endémie lépreuse au Sénégal en 2002. Med Ma Inf. 2005;35:225-7.
4. Keita M, Soumah MM, TraoréFA, DianéBF, Camara AD, A Camara et al. Lèpre dans la ville de Conakry :étude rétrospective de 423 cas. Bull de L’ALLF. 2013;482:313.
5. Raslan-LoubatiéJ, Achirafi A, Oussaïd D, Saïdy H, De Montera A-M, Lernout T, et al. La lèpre, une maladie endémique àMayotte:état des lieux en 2006-2011. Bull Epidémiol Hebd. 2013;41:541-6.
6. Konfe S, Sanon M, Dofini L. Résultat d’une campagne d’élimination de la lèpre dans la Région du Sud-ouest au Burkina Faso. Méd Afr Noire. 2007;54:476-80.
7. Keita S, Tiendrebeogo A, KonaréH, CisséBS, Faye O. Nouveaux cas de lèpre àl’Institut Marchoux. Étude comparative 1988-1997. Ann Dermatol Venereol. 2001;128:217-9.
8. Chisi J E, Nkhoma A, Zverev Y, Misiri H, Komolafe OO. Leprosy in Nkhotakota District Hospital. East Afr Med J. 2003;80:635-9.
9. Saka B, Koumbate K, Mouhari Toure A, Amegan Aho KH, Tchangai Walla K, PitchéP. Lèpre àLomé(Togo) ;étude rétrospective de 383 cas. Med Trop. 2008;68:496-8.
10. Koffi M, N’Guessany, Ekra D, Diarra-Nama J. Cinq ans de notification des cas de lèpre dans le district sanitaire de Yamoussoukro, région des lacs en Côte d’Ivoire. Med Afrique Noire. 2001;48:346-50.
11. Phaff C, Van Den Broek J, Mac Arthur A Jr, Ndeve A, Stuip Y. Characteristics and treatement out comes of leprosy patients detected during a leprosy elimination campaign in Mozambique compared with routinely detected patients. Lepr Rev. 2003;74:229-39.
12. Ogbeiwi OI. Progress towards the elimination of leprosy in Nigeria:a review of the role of policy implementation and operational factors. Lepr Rev. 2005;6:65-76.
13. Groenen G. Trends in prevalence and case finding in the ALERT leprosy control programme, 1979-1999. Lepr Rev. 2002;73:29-40.
14. De Carsalade GY, Achirafi A, Flageul B. La maladie de Hansen dans la collectivitéterritoriale de Mayotte (Océan Indien) :étude rétrospective de 1990 à1998. Acta Leprol. 1999;11:133-7.
15. Tiendrebeogo A, Adrianarisoa SH, Andriamitantsoa J, Vololoarinosinjatovo MM, Ranjalahy G, Ratrimoarivony C et al. Enquête sur la qualitédu diagnostic de la lèpre àMadagascar. Ann Dermatol Vénérol. 2008;135:645-50.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|



Comments are closed.