Dermatologists and burnout: Myth or reality?
Hali Fouzia1, Mahdar Yasmine 1*, Battas Yasmine2, Chiheb Soumiya1, Battas Omar2
1*, Battas Yasmine2, Chiheb Soumiya1, Battas Omar2
1Department of Dermatology and Venereology, University Hospital Center Ibn Rochd, Casablanca, Morocco, 2Department of Psychiatry, University Hospital Center Ibn Rochd, Casablanca, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Although dermatologists are known to have a good level of job satisfaction, they no longer rank among the happiest healthcare professionals. Our study aimed to estimate the prevalence of burnout among dermatologists and define its risk factors and methods of prevention.
Materials and Methods: This was a multicenter, cross-sectional study conducted in Morocco over five months from February to June 2022.
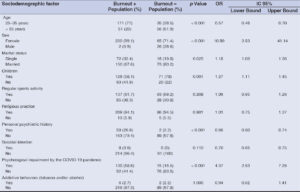
Results: A total of 313 responded to the survey, among which 70.95% suffered from burnout. The risk factors associated with burnout were the female sex (p < 0.001), being married (p = 0.025), having children (p = 0.001), full-time work (p = 0.05), lack of time for research (p < 0.001), excessive documentation (p < 0.001), confrontation with aggressive patients (p < 0.001) as well as insufficient remuneration at work (p < 0.001).
Conclusion: Burnout among dermatologists is pervasive and costly for professional life. Institutions need to provide stress management interventions, and dermatologists must balance patient care with other interests such as research and teaching.
Key words: Burnout, Psychology, Dermatology, Risk factors, Prevention and control
INTRODUCTION
Burnout is a state of emotional exhaustion, depersonalization, and low personal accomplishment leading to low productivity [1]. It is a major problem among healthcare professionals, affecting not only the quality of life of doctors yet also the quality of care provided [2].
Burnout among dermatologists has received particular attention in the last decade [3]. Although known to have a good job satisfaction level, dermatologists no longer rank among the happiest health professionals [4]. A limited number of publications have treated burnout among dermatologists and no studies have been conducted in the Maghreb before.
Our study aimed to estimate the prevalence of burnout among dermatologists in Morocco and to define its risk factors and methods of prevention.
MATERIALS AND METHODS
This was a multicenter, cross-sectional study conducted in Morocco over five months from February to June 2022. Participants were dermatologists in training (interns and residents) and specialists practicing in public and private sectors. We excluded dermatologists not practicing or retired.
Data collection was conducted using an online survey distributed on social media platforms. It consisted of three sections: sociodemographic data, work-related data, and the original version of the Maslach Burnout Inventory (MBI) [5]. The MBI consists of twenty-two items that explore three dimensions: emotional exhaustion (nine items), dehumanization (five items), and personal fulfillment at work (eight items). Each scale gave a score, and the three of them allowed us to situate the state of burnout. We considered the burnout mild when only one dimension was affected, moderate if two dimensions were affected, and severe when all dimensions were affected.
Statistical analyses were performed using IBM SPSS Statistics 26.0. Univariate analysis was performed using the chi-squared test. The multivariate analysis was performed using logistic regression (stepwise descending method). The significance level was at 0.05.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The data collected was anonymous and confidential and informed consent was obtained from all the participants included in the study.
RESULTS
A total of 313 dermatologists responded to the survey. Regarding the socio-demographic characteristics, there was a predominance of females and the 25–35 age group. 71.2% were married and 89.6% had children. 19.5% had a personal psychiatric history of anxiety or depression and 81% were on psychotropic medication. 46.3% were psychologically affected by the COVID-19 pandemic and 2.6% had addictive behaviors, such as smoking and/or drinking alcohol.
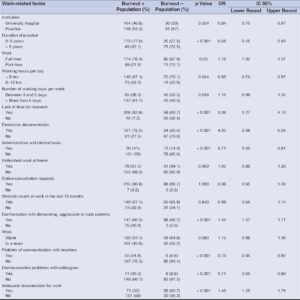
Regarding work-related characteristics, 57.2% were specialists and 66.5% had been practicing for less than five years. All participants practiced in an urban environment (55.9%). 53.7% practiced in a university hospital and 46.3% in the office. 81.2% worked full time, 70.6% worked less than eight hours a day, and 58.1% more than five days a week. Most doctors lacked time to do research, 59.1% found documentation excessive, and a third brought unfinished work home or had a lot of administrative and office tasks. 78.9% received online consultation requests through social networks and mobile phones and 75.1% were confronted with aggressive patients, 42.8% worked in a team, among which 91.04% followed the hierarchical model and only 41.2% felt sufficiently remunerated for their work.
Overall, two hundred and twenty-two dermatologists (70.95%) suffered from burnout in at least one of the subscales of the MBI. Reduced personal accomplishment was found in 42.8% of the participants, emotional exhaustion in 31%, and depersonalization, loss of empathy, and dehumanization in 26.8%. Burnout was classified as mild in 57.2%, moderate in 33.7%, and severe in 9.1% of the participants (Fig. 1).
After statistical analysis, the sociodemographic risk factors significantly associated with burnout among dermatologists were the female sex, being married, having children, and psychological affection by the COVID-19 pandemic. Age between 25 and 35 years and the absence of a personal psychiatric history were considered as protective factors (Table 1). Regarding work-related factors, full-time work, lack of time for research, excessive documentation, confrontation with demanding, aggressive, or rude patients, and insufficient remuneration at work were considered risk factors for burnout. Working in the office for less than eight hours a day, less than five years in practice, in the absence of administrative tasks, or having communication problems with colleagues and teachers were considered protective factors (Table 2).
DISCUSSION
Our study revealed that dermatologists commonly suffer from burnout, with a predominance of the mild form (57.2%). The Medscape National Physician Burnout and Suicide Report published in 2022 reported a lower burnout rate (33%) among dermatologists [6].
In our series, the MBI score revealed that almost 50% of the dermatologists had a low rate of personal accomplishment, while a high rate of emotional exhaustion and depersonalization were found in 31% and 26.8%, respectively. According to Shoimer’s study, the results were similar, with a higher rate of emotional exhaustion [7], which may be explained by the inclusion of residents only in this study.
In our study, the sociodemographic risk factors of burnout among dermatologists were the female sex, being married, having children, and psychological affection by the COVID-19 pandemic. The female sex has long been considered a risk factor due to the burden of childcare responsibilities in their households [6]. The challenges posed by the COVID-19 pandemic also exacerbate existing burnout. In an American study, the most common COVID-19 related burnout factors among dermatologists were uncertainty about the future, teledermatology, fear of exposing loved ones to COVID-19, and reduced remuneration [8]. Age between 25 and 35 years was considered a protective factor in our study. While in another study, women aged between 20–35 and 55 years and over were particularly vulnerable to burnout [9]. In fact, age or work experience may not be the real cause of burnout, yet rather the accumulation of stress problems in modern work life [2].
Regarding work-related factors, full-time work, lack of time for research, excessive documentation, confrontation with aggressive or rude patients, and insufficient remuneration at work were considered risk factors of burnout. These results are consistent with the literature [10,11]. In our series, working in a practice, for less than eight hours per day and less than five years, without administrative and office tasks were considered protective factors. This could be explained by the increased rate of burnout in hospitals due to the high workload. The assessment of burnout among Canadian dermatology residents revealed that they are more prone to burnout and that examinations were the main factor contributing to their burnout (61%). In addition, demanding workloads within the hospital was also a risk factor [7]. The absence of communication problems with colleagues and teachers was also considered as a protective factor. According to Darban et al., the mean burnout score decreased significantly during the follow-up phase after training in communication skills [12].
CONCLUSIONS
Burnout among dermatologists is pervasive, pernicious, and costly for professional and human life. The risk factors are intraindividual, interindividual, and organizational, hence the interest in implementing a prevention program in these different levels.
Institutions should make efforts and provide stress management interventions and training in communication techniques and also involve dermatologists, especially residents, in decision-making and implement better management of administrative tasks. Dermatologists should also seek a balance between patient care and other interests such as research and teaching, learn to work in a team, and adopt a healthier lifestyle.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. De Hert S. Burnout in healthcare workers:Prevalence, impact and preventative strategies. Local Reg Anesth. 2020;13:171 83.
2. Lindblom KM, Linton SJ, Fedeli C, Bryngelsson IL. Burnout in the working population:Relations to psychosocial work factors. Int J Behav Med. 2006;13:51 9.
3. Elsaie ML, Hussein SM, Zaky MS, Hanafy NS, Jafferany M. Therapeutic implications of prevalence and predictor risk factors for burn out syndrome in Egyptian dermatologists:A cross-sectional study. Dermatol Ther. 2020;33:e14327.
4. Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94:1681 94.
5. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory:Third edition. 1997.
6. Physician Burnout and Depression Report 2022:Stress, Anxiety, and Anger [Internet]. Medscape. Available in:https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664. Accessed 16 June 2022.
7. Shoimer I, Patten S, Mydlarski PR. Burnout in dermatology residents:A Canadian perspective. Br J Dermatol. 2018;178:270 1.
8. Shah P, Dorrell DN, Feldman SR, Huang WW. The impact of the coronavirus disease 2019 pandemic on dermatologist burnout:A survey study. Dermatol Online J. 2021;27:1.
9. Marchand A, Blanc ME, Beauregard N. Do age and gender contribute to workers’burnout symptoms?Occup Med Oxf Engl. 2018;68:405 11.
10. Colon A, Gillihan R, Motaparthi K. Factors contributing to burnout in dermatologists. Clin Dermatol. 2020;38:321 7.
11. Nagler AR, Shinkai K, Kimball AB. Burnout among all groups of physicians:Mitigation strategies for dermatologists. JAMA Dermatol. 2020;156:1049 50.
12. Darban F, Balouchi A, Narouipour A, Safarzaei E, Shahdadi H. Effect of communication skills training on the burnout of nurses:A cross-sectional study. J Clin Diagn Res JCDR. 2016;10:IC01 4.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-6868-892X http://orcid.org/0000-0001-6868-892X http://orcid.org/0000-0003-3522-7427 http://orcid.org/0000-0003-3522-7427 http://orcid.org/0000-0002-6206-9981 http://orcid.org/0000-0002-6206-9981 http://orcid.org/0000-0002-1351-0734 http://orcid.org/0000-0002-1351-0734 |





Comments are closed.