Unusual presentation of a rare skin tumor: Glomangioma
Dermatology, Venereology and Leprosy, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Glomus tumor is a benign neuromyoarterial tumor of mesenchymal origin that arises from glomus bodies [1]. It may be of two types: glomangioma and glomangiomyoma depending on the amount of glomus cells, blood vessels, and smooth muscles in the tumor. In 1935, Bailey first described the term glomangioma as those glomus tumors that had wide vascular lumen. On the other hand, the term glomangiomyoma was coined for those tumors in which spindle shaped smooth muscle cells were seen with typical glomus cells [2]. Glomangioma is a rare, slow-growing benign tumor of the dermis or subcutaneous tissue occurring most commonly in the distal phalanx. The extradigital location of the tumor has rarely been reported.
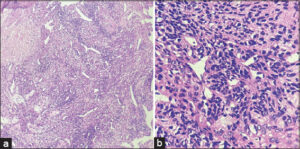
A 64-year-old female presented to the dermatology department on an outpatient basis with a six-year history of a painful, raised lesion on the right leg, which was gradually progressive, not associated with itching or any fluid discharge and had no preceding history of trauma. There was a history of an increase in pain from the lesion on exposure to cold temperature. She had done various home remedies yet never consulted for the same. On examination, a single well-defined, hyperpigmented to erythematous, firm, tender papule measuring nearly 0.5 cm in diameter with surrounding erythema was noted on the lateral aspect of the upper one-third of the right leg (Fig. 1). Routine investigations were within normal limits. An excision biopsy was done to exclude the differentials of painful skin tumors such as dermatofibroma, pyogenic granuloma, neurilemmoma, neuroma, and angiolipoma. The histopathology report demonstrated a non-epithelial neoplasm in the deep dermis made of irregular vascular channels showing monomorphous, rounded cells with abundant pink cytoplasm and oval nuclei in the vessel walls and was consistent with glomangioma (Figs. 2a and 2b). MRI of the leg was conducted and demonstrated a soft tissue mass extending deeper into the extra muscular layer. The patient was then referred to the surgery department for further management.
The incidence of glomus tumors is 1–5% of all soft tissue tumors of the upper extremities, occurring mostly in the nail bed [1]. The various unusual sites reported in the literature to date have been the ankle, foot, knee, thigh, and hip [3]. Histopathology of the tumor shows a variable number of glomus cells, blood vessels, and smooth muscles, depending on which they are classified as glomangioma or glomangiomyoma [4]. Although the previous concept of this classification was widely accepted, subsequent ultrastructural analysis and Masson’s theory on glomus tumors have disproved this categorization of glomus tumors, according to which both glomangioma and glomangiomyoma have only minor quantitative differences [5]. Nonetheless, these terms are still being used as separate entities. A solitary glomus tumor classically presents with the triad of pain, cold sensitivity, and point tenderness [6], and is, therefore, a differential of painful skin tumors [7].
The true incidence of glomus tumors could be higher due to misdiagnosis. Therefore, it is imperative to consider this differential whenever such a patient presents to the OPD to prevent mismanagement. As a dictum, any painful papulo-nodular lesion presenting with a long-standing history, not regressing spontaneously, rather progressively increasing, in size should be considered as a differential for painful skin tumors and subjected to a biopsy.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Rao G, Indira D, Kamal J. Extra digital glomangioma. Indian J Dermatol. 2010;55:397.
2. Chalise S, Jha A, Neupane PR. Glomangiomyoma of uncertain malignant potential in the urinary bladder:A case report. JNMA J Nepal Med Assoc. 2021;59:719-22.
3. Kumar T, Jamal I, Nigam JS, Pandey JK. Malignant glomus tumor of the index finger. Autops Case Rep. 2020;10:e2020184.
4. Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW. Clinical and histopathological diagnosis of glomus tumor:An institutional experience of 138 cases. Int J Surg Pathol. 2015;23:181-8.
5. Senhaji G, Gallouj S, El Jouari O, Lamouaffaq A, Rimani M, Mernissi FZ. Rare tumor in unusual location–glomus tumor of the finger pulp (clinical and dermoscopic features):A case report. J Med Case Rep. 2018;12:1-5.
6. Tang CY, Tipoe T, Fung B. Where is the lesion?Glomus tumours of the hand. Arch Plast Surg. 2013;40:492-5.
7. Cohen PR, Erickson CP, Calame A. Painful tumors of the skin:“Calm hog fled pen and gets back.”Clin Cosmet Investig Dermatol. 2019;12:123-32.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (contact@odermatol.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-0390-6142 http://orcid.org/0000-0003-0390-6142 http://orcid.org/0009-0002-5868-3978 http://orcid.org/0009-0002-5868-3978 |






Comments are closed.