Leprosy in Morocco: A disease not to be forgotten in the twenty-first century
Najoua Ammar , Sara Kerroum, Kawtar Znati, Laila Benzekri, Karima Senouci
, Sara Kerroum, Kawtar Znati, Laila Benzekri, Karima Senouci
Department of Dermatology and Venereology, CHU Ibn Sina, Université Mohammed V Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Leprosy, also known as Hansen’s disease, is a chronic granulomatous disease caused by infection by Mycobacterium leprae. It affects the skin, peripheral nerves, mucosa of the upper airways, and other tissues. The disease shows polar clinical forms depending on the patient’s immune response, as well as other intermediate forms [1]. The diagnosis, based on clinical suspicion, is confirmed by bacteriological and histopathological analyses. The WHO has decided to interrupt the transmission of leprosy globally by 2020. Leprosy is highly rare in Morocco, yet some cases are reported [2].
Herein, we report a case of borderline lepromatous leprosy revealed by a maculopapular rash and successfully treated with multidrug therapy.
A 71-year-old female patient was referred to our department for the etiological assessment of a chronic maculopapular dermatosis evolving since 2017, located on the back and limbs. She had no medical history.
The patient reported sensitivity disorders of the extremities, such as paresthesia with gloves and socks without associated motor disorders.
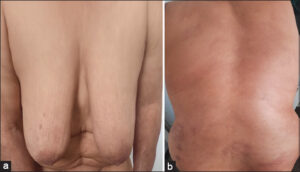
A clinical examination revealed infiltrated, reddish-brown plaques (Figs. 1a and 1b), without hypoesthesia or anhidrosis. A mucosal examination was normal. The general condition was preserved. The examination showed no adenopathy. A neurological examination revealed no peripheral nerve hypertrophy. An ophthalmologic examination was without abnormalities.
The skin histology of a papule revealed a dermal inflammatory infiltrate of lymphocytes and histiocytes with clear perivascular and adnexal cytoplasm. On Ziehl–Neelsen staining, multiple acid-fast bacilli clustered together, suggestive of Hansen’s bacillus, were observed. Bacteriological sampling of the ear lobule was positive, with a bacteriological index of 4 crosses.
As the patient had multibacillary leprosy, the treatment regimen recommended by the WHO in countries with high leprosy endemicity such as Morocco was administered based on a triple therapy, including dapsone, clofazimine, and rifampicin.
Clinical and bacteriological improvement was obtained after six months of treatment (Figs. 2a and 2b).
Active screening of the patient’s close contacts was performed.
Leprosy, or Hansen’s disease, is a chronic infection with cutaneous and nervous tropism caused by Mycobacterium leprae. Although it remains a major public health problem in some countries, it is rare in Morocco and occurs in the rural and remote areas of the north. Clinical expression depends on the quality of the patient’s immune response to M. leprae. It is polymorphic and represents a continuum in which two extreme forms are tuberculoid leprosy and lepromatous leprosy. Tuberculoid leprosy develops when the patient’s immunity is relatively strong and is characterized by a low number of lesions and by the histological presence of a lympho-epithelioid granuloma with a low number of Hansen’s bacilli. In contrast, lepromatous leprosy is marked by low immunity, hence the richness of the clinical-bacteriological picture. In this case, the cutaneous lesions are numerous, small, and not hypoesthetic [3–5].
According to the WHO classification, our patient had multibacillary leprosy as it had more than five symmetrical, poorly limited, confluent skin lesions on the trunk. In the Ridley and Jopling classification, the patient was classified, according to the clinical, bacteriological, and histological criteria, as falling between the polar lepromatous form (LL) and the borderline lepromatous form (BL) [3–6].
The treatment of leprosy has been based on polychemotherapy (rifampicin, dapsone, clofazimine) since the recommendations of the WHO in 1981. The combination and duration of treatment vary depending on the form of leprosy [5–7].
In spite of the progress made at the national level in the fight against leprosy, leprosy is still far from having disappeared. This observation confirms the necessity, in a patient originating from a leprosy endemic country, to evoke the diagnosis of leprosy in front of any unexplained atypical cutaneous lesions associated or not with sensorimotor disorders.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Ridley DS, Jopling WH. Classification of leprosy according to immunity:A five group system. Int J Lepr Other Mycobact Dis. 1966;34:255-73.
2. WHO. Global leprosy update, 2018:Moving towards a leprosy-free world. Wkly Epidemiol Rec 2019;94:389–412 https://www.who.int/publications-detail-redirect/who-wer9435-36/. accessed 15 April 2021.
3. Gupta R, Kar HK, Bharadwaj M. 2012. Revalidation of various clinical criteria for the classification of leprosy:A clinic-pathological study. Lepr Rev 83:354-62.
4. Singh A, Weng X, Nath I. Skin biopsy in leprosy. In:Khopkar U, ed. Skin Biopsy- Perspectives. London:IntechOpen;2011:74-86.
5. Moschella SL. An update on the diagnosis and the treatment of leprosy. J Am Acad Dermatol 2004;51:417-26.
6. World Health Organization. 2013. WHO multidrug therapy (MDT). World Health Organization, Geneva, Switzerland. http://www.who.int/lep/mdt/en
7. De Carsalade G, Wallach D, Spinler E, Pennec J, Cottenot F, Flageul B. Daily multidrug therapy for leprosy:Results of a fourteen-year experience. Int J Lepr Other Mycobact Dis. 1997;65:37-44.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (contact@odermatol.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-6348-4450 http://orcid.org/0000-0001-6348-4450 http://orcid.org/0009-0005-7920-3082 http://orcid.org/0009-0005-7920-3082 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0002-5204-0528 http://orcid.org/0000-0002-5204-0528 |





Comments are closed.