Cutaneous leishmaniasis: The frequency according to geographical distribution in Al-Ramadi, Iraq
Abdullah Mancy 1, Khalid Mohammed Awad2, Zainab Hafedh2
1, Khalid Mohammed Awad2, Zainab Hafedh2
1Private Clinic of Dermatology and Venereology, Al-Ramadi City, Al-Anbar Governorate, Iraq, 2Department of Dermatology and Venereology, Al-Ramadi Teaching Hospital, Al-Anbar Health Directorate, Ministry of Health/Iraq
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Cutaneous leishmaniasis (CL) is a protozoal disease endemic in most cities of Iraq. The disease is caused by different species of the Leishmania genus via the bite of an infected female sandfly. Different species of the sandfly act as a vector for the parasite to the different mammalian host, and the human is considered as an incidental host for these parasites. This study was arranged to clarify the distribution of the disease in different regions of Al-Ramadi, Iraq.
Materials and Methods: An observational descriptive study for cutaneous leishmaniasis in Al-Ramadi was conducted for two years (2020 thru 2021). The disease was diagnosed depending on its cutaneous manifestations, while tissue smear and histopathology were done as a confirmatory test especially in atypical cases. Geographically, the city was divided into four regions: region A, region B, region C, and region D, each consisting of numerous districts. All patients were asked about their residence, houses construction, living within their farms, and animal breeding.
Results: Three hundred and ninety-one patients were examined at the Dermatology Clinic of Al-Ramadi Teaching Hospital during a period of two years (2020 thru 2021). There was a variation in the number of cases during the two years. 53.70% and 46.30% of the cases occurred during the year 2020 and 2021, respectively. The mainly affected part of the city was along the left side of the Euphrates River (region A, constituting 36.57%). Within this region, Albu-Ali Jassim district was mostly involved (29%). On the right side of the river, the City Centre, region C, was the least one affected (16.88%). The Al-Thalia district within the region C was mostly involved (14.3%).
Conclusion: CL is an endemic disease in Al-Ramadi and represents a public health problem. A high rate of infection was recorded alongside the Euphrates River, especially the rural district, while it was low in the urban side of the city. Any parts of the city may be affected, yet Albu-Ali Jassim, Al-Tamim, Al-Sufia, and Al-Thalia were the most frequently involved regions of the city.
Key words: Leishmaniasis, Old World, Sandfly, Amastigote, Ramadi
INTRODUCTION
Leishmaniasis is a disease caused by obligate intracellular parasites of the genus Leishmania [1]. These parasites are transmitted by the bite of an infected female sandfly [2]. They exist in two forms: the amastigote and the promastigote [3].There are mainly three clinical types of leishmaniasis: visceral, cutaneous an, mucocutaneous [4,5].
The incidence of cutaneous leishmaniasis (CL) is estimated to be 1.0 – 1.5 million cases a year [6]. The disease possesses a substantial risk for residents, military personnel, and those working or traveling to the endemic areas [7]. CL is classified geographically into the old-world and new-world leishmaniasis [8]. Old-world CL is caused by L. tropica, L. major, and L. aetiopica [9]. New-world leishmaniasis is caused by L. mexicana complex species and L. brasiliensis complex [8]. Regarding CL in Iraq, the main species of Leishmania are L. tropica and L. major, which cause the anthroponetic and the zoonotic type, respectively [10]. The virulence of the parasite, the host defense mechanisms, and some environmental factors determine the clinical features and the course of infection [11].
The disease has been endemic in Iraq since a long time, yet from now and then, runs outbreaks or epidemics according to environmental factors. The frequency of the disease has increased so it may be seen in many cities from north to south of Iraq [12]. CL manifests with various morphologies that range from small papules with a central crater to large and disfiguring ulcers [13]. The lesion usually appears on the exposed parts of the body, especially the face and extremities [14] (Figs. 1a – 1d). In endemic regions, the diagnosis of the infection may be established easily depending on its clinical presentation [15]. In unusual cases, tissue smear, culture, histopathological examination, and polymerase chain reaction (PCR) tests may be performed for confirmation of the infection [16]. CL is an endemic disease in Al-Ramadi [1]. This study was arranged to shed light on the distribution of the disease in different regions of the city.
MATERIALS AND METHODS
This study was an observational, descriptive study on CL in Al-Ramadi. This city is the capital of Al-Anbar governorate that lies west of Iraq. The city is divided by the Euphrates River into two halves, right and left. The right side is subdivided into two parts by a water drain that originates from the right side of the Euphrates. This water drain evacuates excess water from that river.
Geographically, the city was divided into four regions. Region A is the part that lies on the left side of the Euphrates River. The area on the right side of the Euphrates is further subdivided into three regions. Region B lies to the west of the water drain. Region C includes the part to the east of this drain, which resembles the city center. Region D is the east of the city. Each one of these regions consists of numerous districts (Fig. 2).
Throughout the city and its surroundings, there are numerous agriculture farms. Also, animal breeding is distributed alongside the Euphrates River and about periphery of the city. The inhabitants of Al-Ramadi are around 900,000 people [1]. Patients affected with CL were examined at the Dermatology Department of Al-Ramadi Teaching Hospital.
Three hundred and ninety-one patients infected with CL were included in this study during the period from the first of January 2020 to the end of December 2021. Depending on at least two dermatologists, the patient who had clinical manifestations of CL was included in the study. In an uncertain infection, a tissue smear was taken from the affected site, and if the amastigotes were not seen, it was excluded from the study. Full information was obtained from all patients regarding their social state, lifestyle, cultural behavior, housing construction, farming, and animal breeding. Informed consent was taken from all patients. An approval for the study was obtained from the ethical committee.
Statistical Analysis
We depended on SPSS, version 22. Statistical analysis of efficacy was completed by chi-squared test. p values < 0.05 were considered significant, while p values < 0.01 were considered highly significant.
RESULTS
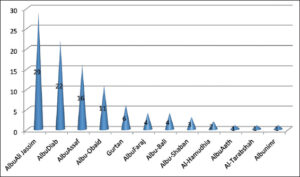
A total of 391 patients affected by CL were examined at the Dermatology Clinic for a period of two years (2020 thru 2021). Most cases of CL were found in region A (36.57%) while the least were recorded in region C (16.88%) (Table 1). Within region A, the most commonly affected area was Albu-Ali Jassim (29%) (p value < 0.01), and the least commonly affected was Albunimr (1%) (Fig. 3).
 |
Table 1: Patients affected with cutaneous leishmaniasis in different regions of Al-Ramadi during the two-year period (2020 thru 2021). |
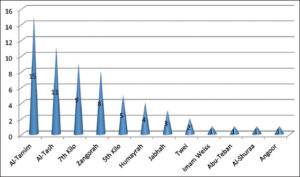
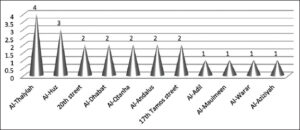
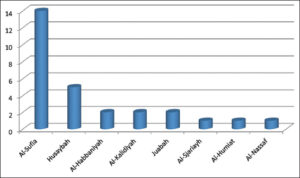
In region B, Al-Tamim district was the most involved (24.6%) (p value < 0.01), and Al-Angor district was the least affected (1%) (Fig. 4). Al-Thaila district was mostly involved in region C (14.3%) (p value < 0.05), while Al-Aziziya was the least involved (1%) (Fig. 5). Al-Sufia was the most involved in region D (50%) (p value < 0.01), while Al-Nassaf was the least involved (Fig. 6).
DISCUSSION
CL has been one of the communicable diseases endemic in Iraq since a long time ago, yet its frequency varies according to numerous environmental factors that affect the breeding of the sand fly as a vector and reservoir animals. This disease represents a major public health problem [17]. The disease was reported in most cities of the country from south to north [18]. In the south (Al-Diwaniya and Al-Rhamania), 300 and 400 cases, respectively, were recorded in 2009 [7,19]. In the north (Kirkuk and Rabeea), 571 and 1482 cases, respectively, were recorded for one year [17]. In Kurdistan provinces, 228 and 257 cases of CL were reported during 2015 and 2017, respectively [7]. Thus, the infections were spread all over Iraqi cities, with some variation in the number of cases. There are numerous factors that play a role in the outcome of the infection, such as availability of the vector and reservoirs for the parasite and health services planning for eradication and control of the vectors, in addition to the cultural behavior of the population that resides in these particular regions.
There was a difference in rate of infection during the years 2020 (53.7%) and 2021 (46.3%). This variation may be explained by two factors. The first one may be related to an improvement in the public health services. These services will control the source of the infections and provide a perfect management for the patients. The second reason behind this variation may be due to the disease itself. CL is characterized by an instability in its behavior, sometimes presenting with high and unsuspected epidemics and with a low rate in others [19].
Due to presence of the Euphrates River, there are widespread areas of agricultural farms, particularly on the right side (region A). These areas resemble a rural district, where most people engage in a farming work as a main source of their income. This farming job by itself increases the risk of CL, as described by Alzahrani et al. [20] and Yadon et al. [21].
In rural areas, most people are used to build their houses inside or nearby their farms. This will expose them more to the insect bites [18]. Animal breeding is distributed through the regions. The presence of animals close to the houses will increase the risk of infection, as mentioned by Votýpka et al. [22]. These animals will represent a reservoir for the parasites [23,24].
The risk of infection will increase especially when these animals are put in a clay-made building with multiple fissures in their walls especially, during rainfall [22]. This will create a hot and humid weather that resemble an ideal environment for the spread of the sand fly [25].
The recorded cases within the city center (Region C), in comparison with other regions, were the lowest rate (16.88%). This is because the living conditions in region C resemble an urban district. The presence of regular house construction and arrangement will decrease the risk of infection, as described by Rojas et al. [26]. The availability of nearby health services with good housing and domestic sanitary conditions will limit the disease spread [25].
The outbreak of CL occurs when many non-immune people migrate to regions where transmission is high [17].This occurred when the city was prone to a terrorist attack. This forced people to leave their houses and migrate to different parts of the country. Also, most of them had difficult living conditions and bad health services within camps.
Numerous factors determine the risk of infection with CL, such as poverty, malnutrition, and population migration [19,27]. Environment and climate changes may affect the disease activity as described by Hakkour et al. [25]. When these factors are applied to the main parts of the city, a difference in the rate of infection from region A to region C will be noticed. Also, these variations will determine the risk of infection in different parts of the same region. Accordingly, we find that Albu-Ali Jassim area is the most involved within region A and the same may apply to other regions.
CONCLUSION
Numerous factors determine the endemicity of cutaneous leishmaniasis in a particular area. Therefore, determination of the focus and sources of the infection through geographical study of the area is the first step in order to control outbreaks and epidemics of the disease and to provide protection for the community.
ACKNOWLEDGMENTS
The authors would like to thank Professor Khalifa E. Sharquie, Department of Dermatology, College of Medicine, University of Baghdad, Iraqi and Arab Board of Dermatology and Venereology, Center of Dermatology and Venereology, Baghdad Teaching Hospital, Medical City, and Dr. Thamer A. Kubaisi, Consultant Dermatologist, Department of Dermatology and Venereology, Medical college, Al-Anbar University, for their kindly and critically reviewing this paper and providing valuable comments.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Mancy A, Awad KA, Abd-AL-Majeed T, Jameel NF. The epidemiology of cutaneous leishmaniasis in Al-Ramdai, Iraq. Our Dermatol Online J. 2022;13:402-7.
2. Sharquie KE, Noaimi AA, Saleh BA. Cutaneous leishmaniasis as imitator of skin diseases and a diagnostic challenge. J Cosm Dermatol Scien Applicat. 2018;8:158-77.
3. AL-Aubaidi I, Al Bayati N, Al Haidari S, Al-Azzawi M. Some histopathological features of cutaneous leishmaniasis-in Iraqi patients. Int J Pharm Tech Res. 2016;9:640-5.
4. Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, Brooker S. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-96.
5. Barkati S, Ndao M, Lib M. Cutaneous leishmaniasis in the 21st century:From the laboratory to the bed. Curr Opin Infect Dis. 2019;32:419-25.
6. El-Deen LD, Abul-Hab J, Abdulah SA. Clinico-epidemiological study of cutaneous leishmaniasis in a sample of Iraqi Armed Forces. Iraqi J Comm Med April. 2006;19:98-103.
7. Abdulla QB, Shabila NP, Al-Hadithi TS. An outbreak of cutaneous leishmaniasis in Erbil Governorate of Iraqi Kurdistan Region in 2015. J Infec Dev Ctries. 2018;12:600-7.
8. Bailey MS, Lockwood DNJ. Cutaneous leishmaniasis. Clin Dermatol. 2007;25:203-11.
9. Masmoudi A, Hariz W, Marrekchi S, Amouri M, Turki H. Old World cutaneous leishmaniasis:Diagnosis and treatment. J Dermatol Case Rep. 2013;7:31.
10. Al-Warid HS, Al-Saqur IM, Al-Tuwaijari SB, Zadawi KAMAL. The distribution of cutaneous leishmaniasis in Iraq:Demographic and climate aspects. Asian Biomedicine. 2017;11:255-60.
11. Aytekin S, Ertem M, Yağdıran O, Aytekin N. Clinico-epidemiologic study of cutaneous leishmaniasis in Diyarbakir Turkey. Dermatol Online J. 2006;12:14.
12. Al-Obaidi M, Yassen M, Al-Saqur IM. Survey study on the prevalence of cutaneous leishmaniasis in Iraq. Iraqi J Scien. 2016;57:2181-7.
13. Khan SJ, Muneeb S. Cutaneous leishmaniasis in Pakistan. Dermatol Online J. 2005;11:4.
14. James WB, Berger TG, Elastone DM. Parasitic infestations, bites and stings:In Andrews diseases of the skin, clinical dermatology. 13th ed. Vol. 1. Philadelphia:WB Saunders company;2020. 491-526 p.
15. Thakur S, Joshi J, Kaur S. Leishmaniasis diagnosis:An update on the use of parasitological, immunological and molecular methods. J Parasit Dis. 2020;44:253-72.
16. Singh S. New developments in diagnosis of leishmaniasis. Indian J Med Res. 2006;123:311.
17. Al-Bajalan MMM, Al-Jaf SMA, Niranji SS, Abdulkareem DR, Al-Kayali KK, Kato H. An outbreak of Leishmania major from an endemic to a non-endemic region posed a public health threat in Iraq from 2014-2017:Epidemiological, molecular and phylogenetic studies. PLoS Negl Trop Dis. 2018;12:e0006255.
18. Al-Hayali HL. Overview on epidemiology of leishmaniasis in Iraq. Rafidian J Scien. 2021;30:28-37.
19. AlSamarai AM, AlObaidi HS. Cutaneous leishmaniasis in Iraq. J Inf Develop Coun. 2009;3:123-9.
20. Alzahrani MJ, Elfaki N, Abdalla YHA, Alkhadher MA, Ali MHM, Ahmed WAM. Cutaneous leishmaniasis:Associated risk factors and prevention in Hubuna, Najran, Saudi Arabia. Int J Gen Med. 2023;16:723-31.
21. Yadon ZE, Rodrigues LC, Davies CR, Quigley MA. Indoor and peridomestic transmission of American cutaneous leishmaniasis in northwestern Argentina:A retrospective case-control study. Am J Trop Med Hyg. 2003;68:519-26.
22. Votýpka J, Kasap OE, Volf P, Kodym P, Alten B. Risk factors for cutaneous leishmaniasis in Cukurova region, Turkey. Trans R Soc Trop Med Hyg. 2012;106:186-90.
23. De Araujo AR, Portela NC, Feitosa APS, da Silva OA, Ximenes RAA, Alves LC, et al. Risk factors associated with American cutaneous leishmaniasis in an endemic area of Brazil. Rev Inst Med Trop. 2016;58:86.
24. Alsamarai AM, Alobaidi AH, Aljumaili ZKM, Jasim MM, Qatal S. Cutaneous leishmaniasis in Iraq:A continuing endemic disease. J Drug Des Res. 2016;3:1204.
25. Hakkour M, Hmamouch A, Mahmoud El Alem M, Bouyahya A, Balahbib A, El Khazraji A, et al. Risk factors associated with leishmaniasis in the most affected provinces by leishmania infantum in Morocco. Interdiscip Perspect Infect Dis. 2020;2020:694⇊.
26. Rojas CA. An ecosystem approach to human health and the prevention of cutaneous leishmaniasis in Tumaco, Colombia. Cad Saude Publica. 2001;17:S193-200.
27. Ngere I, Boru WG, Isack A, Muiruri J, Obonyo M, Matendechero S, et al. Burden and risk factors of cutaneous leishmaniasis in a peri-urban settlement in Kenya, 2016. PLoS One. 2020;15:e0227697.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3688-6953 http://orcid.org/0000-0002-3688-6953 |






Comments are closed.