Madura’s foot: A disabling evolution
Imane Kacimi Alaoui , Hanane Baybay, Sara El-Ammari, Zakia Douhi, Meryem Soughi, Sara Elloudi, Fatima-Zahra Mernissi
, Hanane Baybay, Sara El-Ammari, Zakia Douhi, Meryem Soughi, Sara Elloudi, Fatima-Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Mycetomas are pathological processes in which fungal or actinomycotic agents emit seeds. It is a chronic infectious disease, endemic in tropical countries, that affects the soft tissues and the skeleton with sometimes fatal visceral damage. Foot involvement is by far the most common, occurring in 80% of cases. The treatment of mycetomas depends on their etiology, medical or surgical. Herein, we report a rare case of a foot and leg eumycetoma. The purpose of this work was to recall this rare condition, often overlooked by practitioners, remaining a source of therapeutic difficulties.
Key words: Mycetomas, Madura’s foot, Actinomycetomas
INTRODUCTION
Mycetomas are chronic infections responsible for inflammatory pseudo-tumor lesions due to fungal agents (eumycetomas) or aerobic bacteria (actinomycetomas). They evolve slowly. In addition to developing at the subcutaneous level, they may affect the bone structure, complicating management. Eighty percent of cases are located on the foot, thus known as Madura’s foot [1,2].
CASE REPORT
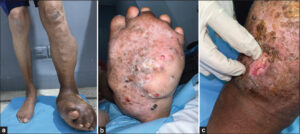
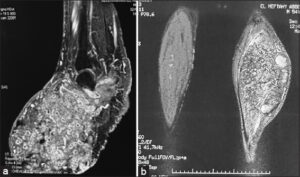
A 53-year-old day laborer with the concept of walking barefoot as an antecedent was traumatized eleven years earlier by a sharp object at the level of the sole of his left foot, causing a wound, for which he was given undocumented local treatment without success. Four years later, a swelling of the foot gradually increased in size. He sought the trauma department, which performed MRI and an initial bone biopsy revealing subacute osteitis. He was given antibiotics. In response to the persistent nature of the disease and the disabling clinical worsening, as well as the appearance of new lesions, the patient sought multiple consultations at the traumatology department before being referred for additional care to our training. An examination preceding admission found that the patient was in good general condition yet had inflammatory pain in the left lower extremity responsible for lameness, with a pseudo-tumor swelling of the left foot, polyfistulized (Fig. 1a), dotted with multiple yellowish and reddish papules (Fig. 1b), and emitting pus and small, yellowish-white grains (Fig. 1c) associated with a painless mass under the skin of the ipsilateral leg. A long anatomopathological examination performed on a local sample from the foot led to the diagnosis of eumycetoma with positive PAS staining. A radiological assessment consisted of standard X-ray of the foot, an ultrasound of the lymph node areas objectifying bilateral inguinal and iliac lymph node formations, and MRI of the foot highlighting a bony extension of the lesions with multiple lacunae affecting all bony structures of the foot and leg, with infiltrations of the subcutaneous tissues, creating a point-in-the-circle appearance (Figs. 2a and 2b). MRI of the left leg showed an 8 cm mycetoma pedicle. The therapeutic decision was to perform a left trans-femoral amputation and to administer an antifungal. The patient unfortunately refused any treatment.
DISCUSSION
Mycetomas are indolent and deforming inflammatory pseudotumors often polyfistulized due to fungi (eumycetoma) or aerobic bacteria (actinomycetoma) [1]. It most commonly affects young, male subjects engaged in manual labor, such as farmers and breeders in humid tropical climates [2].
Sixty percent of cases in the literature indicated anterior trauma. In general, the preferred site is the foot [3], as was the case in our patient. Nevertheless, various extrapodal locations have been described in the literature, including the trunk, hands, and knees [2,4].
Initially, eumycetoma manifests as a firm and painless subcutaneous nodule that evolves into an infiltration with fistulizations, from which intermittent pus and black or yellowish-white grains appear. It is essential to have an accurate biological diagnosis in order to confirm the diagnosis and guide treatment. The procedure is divided into several stages: direct examination and culture of the grains when these are emitted, followed by a biopsy and anatomical pathology examination [1,5].
Generally, mycetomas spread superficially, as well as in depth, gradually engulfing the surrounding tissues, particularly the bones and joints [5–7]. It is common for them to develop slowly and remain painless for a number of months, even years once they have appeared [8,9], which explains the delayed consultations [10,11].
The extent of the pathogenesis must be documented immediately after diagnosis. Plain radiographs may show non-specific lesions (geodes, reactive osteosclerosis), ultrasound or MRI may identify the mycelium by its characteristic morphology: single or multiple small grains appearing on hyperechoic images with posterior shadow cones confirming the context of a point in a circle that is pathognomonic [12–14]. The treatment of fungal infections depends on their etiology. Although there is no established consensus, treatment should be continued over a long period of time [15]. Eumycetoma is usually treated with the antifungal drugs itraconazole, amphotericin B, voriconazole, and terbinafine for a prolonged period of 12 to 15 months. Surgery remains the solution of choice for initial lesions and is strongly indicated in cases of bone lysis [1,10]. Lymph nodes are a route for the spread of pathogens with the possibility of inguinal localization [16,17]. There are no satisfactory criteria to confirm healing. The risk of postoperative recurrence is always present. Only long-term monitoring over several years may confirm the cure. In this case, the treatment should be continued at a reduced dose for several months [18]. Prevention is of great interest. It consists of wearing protective shoes, thoroughly and systematically disinfecting wounds, and avoiding injuries, especially thorns [16].
CONCLUSION
Fungal mycetomas are rare and recurring infections that may make them difficult to recognize. Treatment depends on the pathogen and the extent of the lesion. Immediate and early treatment is indicated to improve prognosis and avoid disabling sequelae.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Traore T, Toure L, Diassana M, Niang M, Ballo E, S Coulibaly B, et al. [Medico-Surgical treatment of mycetoma in the Somine Dolo hospital of Mopti (Mali)]. Med Trop Sante Int. 2021;1:mtsi.2021.170.
2. Ndiaye D, Ndiaye M, Sène PD, Diouf MN, Diallo M, Faye B, Sakho MG, Ndiaye JL, Tine R, Kane A, Ndir O. [Mycetomas diagnosed in Senegal from 2008 to 2010]. J Mycol Med. 2011;21:173-81.
3. Sigera LSM, Narangoda KUL, Dahanayake MY, Shabri ULF, Malkanthi MA, Somarathne V, et al. Mycetoma due to Madurella mycetomatis. IDCases. 2020;30;21:00857.
4. Dikhaye S, Afifi Y, Aoufi S, Tligui H, Mirrane H, Senouci K, et al. [Mycetoma]. Ann Dermatol Venereol. 2008;135:626-8.
5. Daghfous M, Mokhtar I, Fazaa B, Kamoun MR. [Anatomo-clinical study of mycetomas]. Tunis Med. 1993;71:529-34.
6. Omer RF, Seif El Din N, Abdel Rahim FA, Fahal AH. Hand mycetoma:The Mycetoma Research Centre experience and literature review. PLoS Negl Trop Dis. 2016;2;10:e0004886.
7. Gupta M. Maduromycosis of foot. Our Dermatol Online. 2017;8:92-3.
8. N’diaye B, Dieng MT, Perez A, Stockmeyer M, Bakshi R. Clinical efficacy and safety of oral terbinafine in fungal mycetoma. Int J Dermatol. 2006;45:154-7.
9. Ait Essi F, Akbari I, Najeb Y, Latifi M, Hokar O, Amal S. Le myce-tome tumoral du pied. Med Chir Pied. 27:9-11.
10. Aounallah A, Boussofara L, Ben Saïd Z, Ghariani N, Saidi W, Denguezli M, et al. [Analysis of 18 Tunisian cases of mycetoma at the Sousse hospital (1974-2010)]. Bull Soc Pathol Exot. 2013;106:5-8.
11. Baha H, Khadir K, Hali F, Benchikhi H, Zeghwagh A, Zerouali K, et al. [Actinomycosic mycetoma of the foot in Morocco due to Actinomycetes viscosus]. J Mycol Med. 2015;25:76-80.
12. Dieng MT, Sy MH, Diop BM, Niang SO, Ndiaye B. [Mycetoma:130 cases]. Ann Dermatol Venereol. 2003;130(1 Pt 1):16-9.
13. Messoudi A, Fnini S, El Andaloussi Y, Charafeddine A, Marouane S, Ouarab M, et al. [Madura foot:A rare pathology in Morocco (about 15 cases)]. Bull Soc Pathol Exot. 2013;106:9-12.
14. Fuentes-Nava AG, Fierro-Arias L, Araiza J, Benitez-Barradas MI, Peláez González HE, Bonifaz A. Actinomycetoma due to Actinomadura madurae:A therapeutic challenge. Case report. Our Dermatol Online. 2018;9:399-403.
15. Asly M, Rafaoui A, Bouyermane H, Hakam K, Moustamsik B, Lmidmani F, et al. Mycetoma (Madura foot):A case report. Ann Phys Rehabil Med. 2010;53:650-4.
16. Sarr L, Niane MM, DiéméCB, Diatta BA, Coulibaly NF, DembéléB, et al. [Surgery in black grain mycetoma:About 44 patients treated at aristide le dantec hospital (Dakar, Senegal) from December 2008 to March 2013]. Bull Soc Pathol Exot. 2016;109:8-12.
17. Salim AO, Mwita CC, Gwer S. Treatment of Madura foot:A systematic review. JBI Database System Rev Implement Rep. 2018;16:1519-36.
18. Brufman T, Ben-Ami R, Mizrahi M, Bash E, Paran Y. Mycetoma of the foot caused by Madurella mycetomatis in immigrants from Sudan. Isr Med Assoc J. 2015;17:418-20.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (contact@odermatol.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-0582-321X http://orcid.org/0000-0003-0582-321X http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0001-6330-2856 http://orcid.org/0000-0001-6330-2856 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |




Comments are closed.