Two subcutaneous cold abscesses after accidental bacillus Calmette–Guérin revaccination in an adult with urothelial carcinoma of the bladder
Fatima Ezzahra Amakha 1, Fatima Ezzahra Ghlalou2, Anas Fakhri2, Hanane Rais2, Said Amal1, Ouafa Hocar1
1, Fatima Ezzahra Ghlalou2, Anas Fakhri2, Hanane Rais2, Said Amal1, Ouafa Hocar1
1Department of Dermatology and Venereology, Mohammed VI University Hospital Center, Bioscience and Health Laboratory, Cadi Ayyad University, FMPM, Marrakech, Morocco, 2Department of Anatomical Pathology, Mohammed VI University Hospital Center, Bioscience and Health Laboratory, Cadi Ayyad University, FMPM, Marrakech, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
The complications of bacillus Calmette–Guérin (BCG) revaccination are poorly described. The objective was to report a rare case of two subcutaneous abscesses caused by accidental BCG revaccination. A 63-year-old patient, followed for non-invasive urothelial carcinoma of the urinary bladder resected on two occasions with a recurrence, was scheduled for BCG immunotherapy. One month before admission, the patient, accidentally, received two subcutaneous injections of BCG in the left arm and periumbilical area. Three weeks later, the patient presented two subcutaneous cold abscesses at both injection sites. Ziehl–Neelsen stain found an acid-alcohol resistant bacillus. A culture showed Mycobacterium bovis. The patient received local isoniazid for two months with good evolution. Although adverse reactions are rare after BCG revaccination, it is crucial to continue monitoring to learn more and choose timely treatment if they occur.
Key words: Bacillus Calmette–Guérin immunotherapy, BCG vaccination, BCG revaccination, Subcutaneous cold abscesses, Urothelial carcinoma of the bladder
INTRODUCTION
Bacillus Calmette–Guérin (BCG) vaccine is a live-virus vaccine with attenuated strains of Mycobacterium bovis [1,2] employed in tuberculosis vaccination with an excellent safety profile. The local and systemic complications of BCG vaccination were well described in the literature. The frequency of these complications is low in relation to the large number of vaccinations performed. They are common in cases of overdosing and with poor vaccination techniques. They are mostly benign. The complications of revaccination, as in this observation, are much less described. The objective was to report a case of complications resulting from accidental BCG revaccination.
CASE REPORT
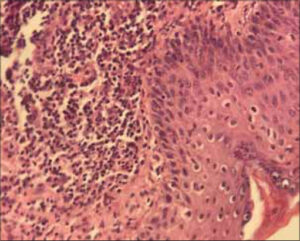
Herein, we report the case of a 63-year-old patient followed for non-invasive low-grade papillary urothelial carcinoma of the bladder, resected on two occasions with a recurrence. A decision was reached to treat the patient with BCG immunotherapy. The procedure consisted of administering BCG in liquid form into the bladder through a catheter once a week for six weeks in two-hour sessions. One month before admission, the patient received two subcutaneous injections of BCG (powder for intravesical suspension) in the left arm and periumbilical area following a misinterpretation of the prescription by the dispensing pharmacy. Three weeks after the injections, the patient presented two nodular and erythematous lesions, painless, of soft consistency, measuring 3 x 2.5 cm for the lesion of the arm and 5 x 5 cm for the periumbilical lesion, not improving under well conducted antibiotic therapy. The physical examination was normal, including pleuro-pulmonary, lymph node examination. Everything was evolving in a context of apyrexia and the conservation of the general state. Puncture of the lesions yielded frank pus. A search for pyogenic germs was negative. Ziehl–Neelsen stain found an acid-alcohol resistant bacillus. A culture showed Mycobacterium bovis. A skin biopsy from both sites revealed polymorphic granulation tissue rich in neutrophil with vascular neogenesis (Fig. 1). The two lesions ulcerated secondarily (Figs. 2a and 2b). Taking into account the risks of oral isoniazid monotherapy in a tuberculosis-endemic country such as ours, we decided to treat the patient with local isoniazid combined with local care (Figs. 3a and 3b) for two months with a good progression.
DISCUSSION
Over the past several decades, BCG therapy for non-muscle invasive bladder cancer has become more widely accepted, especially for intermediate- and high-risk patients. Intravesical BCG instillation continues to be the primary setting for the high-risk population at this time [3,4]. Our patient was a candidate for this therapeutic strategy, and by mistake, he received the BCG vaccine as a subcutaneous injection in the left arm and periumbilical area. In countries with high tuberculosis endemicity, localized BCG vaccine side effects, such as injection site abscesses, hypersensitivity reactions, and localized lymphadenopathy, are typically self-limiting [5]. BCGitis is a specific reaction to the BCG vaccine, described mainly in children. Depending on the location in relation to the injection site, a distinction is made between local, locoregional, distant, and disseminated forms. The WHO no longer recommends BCG revaccination since it is thought to have minimal or no efficacy [6–10]. The most frequently described complications following revaccination are subcutaneous abscesses and lingering ulcerations. In a retrospective study by Ouazzani et al. conducted in 2007 over a period of five years (between January 2000 and March 2005) including twelve patients presenting complications following revaccination with BCG, the most frequently noted complication was a subcutaneous abscess in two-thirds of the cases, followed by persistent secondary ulcerations in around one-third of the cases, including one case of osteitis [11,12]. Complications related to revaccination were reported in Brazil in thirteen children and adolescents, dominated by the occurrence of persistent ulcerations [12]. The mechanism of these accidents after revaccination has been poorly studied in the literature. Two pathophysiological mechanisms have been proposed: infectious and immunological. However, the presence of Mycobacterium bovis in the wounds is compatible with an immunological phenomenon at the origin of these skin lesions. It may be a type III hypersensitivity reaction or a local Arthus phenomenon with excess antigen in an already immunized subject with precipitating circulating antibodies. It may also be a delayed hypersensitivity reaction induced by BCG revaccination with the appearance of an inflammatory erythematous reaction followed by central necrosis. The proportion of responsibility between the two main types of pathophysiological mechanisms—infectious and immunological—is difficult to assess.
In the literature, there is no consensus on the treatment for BCG as per side effects, and the management approach varies between cases and countries. According to some authors, the effectiveness of oral antibiotics, such as isoniazid, erythromycin, and an isoniazid and rifampicin combination, in treating BCG complications is debatable. The use of isoniazid monotherapy for the treatment of local BCG complications may be limited by the development of resistance during treatment [13,14]. Drainage and chemotherapy with erythromycin or isoniazid are typically effective treatments for injection site abscesses [14]. Taking into account the risks of oral isoniazid monotherapy in a tuberculosis-endemic country such as ours, we decided to treat the patient with local isoniazid and local care and noted good evolution. Topical isoniazid may be a reasonable option in this situation given that its use in our case was safe and effective. Future randomized controlled research should explore this hypothesis.
CONCLUSION
Revaccination is no longer recommended by the WHO, and several studies have concluded that revaccination is unnecessary. The favorable evolution of our case may have been related to a low virulence of the strain or the effectiveness of antibiotic therapy. In the case of accidental vaccination, preventive treatment is strongly recommended.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. World Health Organization. BCG vaccines:WHO position paper. Weekly Epidemiological Record. 2018;93:73-96.
2. Andersen P, Woodworth JS. Tuberculosis vaccines-rethinking the current paradigm. Trends Immunol. 2014;35:387-95.
3. Liu G, Li B, Xu Z, Wang J, Ma S, Kan Y, et al. Bacillus Calmette–Guerin for the treatment of non-muscle invasive bladder cancer:History and current status. Discov Med. 2022;33:85-92.
4. Saluja M, Gilling P. Intravesical bacillus Calmette–Guerin instillation in non-muscle-invasive bladder cancer:A review. Int J Urol. 2018;25:18-24.
5. Sellami K, Amouri M, Kmiha S, Bahloul E, Aloulou H, Sfaihi L, et al. Adverse reaction due to the bacillus Calmette–Guerin vaccine:Twenty Tunisian cases. Indian J Dermatol. 2018;63:62-5.
6. Roth AE, Benn CS, Ravn H, Rodrigues A, Lisse IM, Yazdanbakhsh M, et al. Effect of revaccination with BCG in early childhood on mortality:Randomised trial in Guinea-Bissau. BMJ. 2010;340:671.
7. Glynn JR, Fielding K, Mzembe T, Sichali L, Banda L, McLean E, et al. BCG re-vaccination in Malawi:30-year follow-up of a large, randomised, double-blind, placebo-controlled trial. Lancet Glob Health. 2021;9:1451-9.
8. Barreto ML, Pereira SM, Pilger D, Cruz AA, Cunha SS, Sant’Anna C, et al. Evidence of an effect of BCG revaccination on incidence of tuberculosis in school-aged children in Brazil:Second report of the BCG-REVAC cluster-randomised trial. Vaccine. 2011;29:4875-7.
9. Bolursaz MR, Lotfian F, Velayati AA. Bacillus Calmette–Guérin vaccine complications in Iranian children at a University Hospital. Allergol Immunopathol. 2017;45:356-61.
10. D’Aleo F, Bananno R, Costantino ALP, Arena S, Midiri A, Mancuso G, et al. A case of abscess after BCG vaccine in an immunocompetent child without other clinical signs. JMM Case Reps. 2015;2:1-3.
11. Bannister S, Sudbury E, Villanueva P, Perrett K, Curtis N. The safety of BCG revaccination:A systematic review. Vaccine. 2021;39:2736-45.
12. Gyldenlove M, Andersen AB, Halkjaer LB. Cutaneous necrotic ulceration due to BCG revaccination. Human Vacc Immunother. 2012;8:423-4.
13. Alrabiaah AA, Alsubaie SS, Bukhari EI, Gad A, Alzamel FA. Outbreak of bacille Calmette–Guérin-related lymphadenitis in Saudi children at a university hospital after a change in the strain of vaccine. Ann Saudi Med. 2012;32:4-8.
14. Cuello-García CA, Pérez-Gaxiola G, Jiménez Gutiérrez C. Treating BCG-induced disease in children. Cochrane Database Syst Rev. 2013:CD008300.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0006-8788-0988 http://orcid.org/0009-0006-8788-0988 |






Comments are closed.