Recurrent panniculitis in a patient with myelodysplastic neoplasms: A case of neutrophilic lobular panniculitis
Olivo Emmanuel Vilchis-Flores , Fanny Carolina López-Jiménez, Silvia Méndez-Flores, Israel Rojas de Ita
, Fanny Carolina López-Jiménez, Silvia Méndez-Flores, Israel Rojas de Ita
Dermatology Department, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, CDMX, México.
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Neutrophilic dermatoses (ND) encompass a diverse group of inflammatory skin disorders characterized by sterile, predominantly neutrophilic infiltrates. Herein, we present the case of a 38-year-old male with very high-risk hypocellular myelodysplastic neoplasms (MDS) exhibiting recurrent neutrophilic panniculitis (NP) involving the lower extremities. The patient underwent hematopoietic progenitor cell transplantation (HPCT) resulting in lesion remission. This case emphasizes the importance of considering NP in ND diagnoses, especially in the context of hematological disorders. Diffusion of such cases is essential for healthcare professionals to enhance their ability to recognize and effectively address this rare condition.
Key words: Neutrophilic dermatoses, Myelodysplastic neoplasms, Neutrophilic panniculitis
INTRODUCTION
Neutrophilic dermatoses (ND) are a group of inflammatory skin disorders characterized by a sterile, predominantly neutrophilic infiltrate on histopathology. The neutrophilic infiltrate may extend from the epidermis to subcutaneous tissue, leading to uncommon clinical-pathological entities and complex overlapping conditions [1,2]. ND manifests as deep, erythematous, tender, and painful nodules or plaques that typically affect the arms, legs, and trunk [1,3,4]. The lesions typically persist for approx. two weeks and usually result in post-inflammatory hyperpigmentation. Myelodysplastic neoplasms (MDS) have been associated with these groups of dermatoses. First-line treatment involves oral corticosteroids. Some dermatoses may resolve spontaneously, although recurrence is common [2,3,5–7].
CASE REPORT
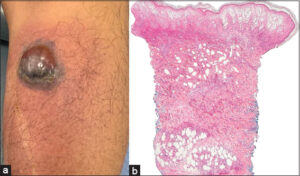
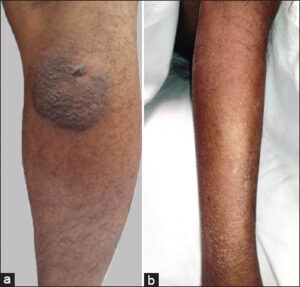
A 38-year-old male from Mexico City, diagnosed with very high-risk hypocellular MDS (IPSS-R score of 6.5 points) and without any known comorbidities, was evaluated two years after his MDS diagnosis by our dermatology department. He had been actively receiving medical treatment with darbepoetin alfa, filgrastim, and eltrombopag. The patient presented an intermittently and slightly painful nodule with a localized increase in temperature in the right lower extremity in the previous 48 hours, which was not associated with fever or other systemic symptoms. He improved after treatment with indomethacin, and the nodule resolved within several weeks. Two months later, he developed a blistering plaque without fever or additional symptoms. A skin biopsy was performed, and the results revealed superficial and deep neutrophilic dermatosis with microabscesses of neutrophils and neutrophilic lobular panniculitis (Fig. 1). At this point, he received therapy with amoxicillin/clavulanate, which resulted in the involution of the lesion, leading to residual post-inflammatory hyperpigmentation (Fig. 2a). Three months later, a nodule with overlying erythema and increased local temperature reappeared, resolving within 72 hours without any treatment. Another biopsy indicated septal and lobular panniculitis without vasculitis, and stains and cultures for bacteria and fungi were negative. Laboratory studies showed the interferon-gamma release assay to be negative multiple times throughout the evaluation, no leukocytosis, neutrophils fewer than 5,000 and below 50%. The patient was scheduled for hematopoietic progenitor cell transplantation (HPSCT). After the transplant, he was evaluated by the dermatology team, presenting only grade II mucositis, which was managed with analgesia. There was no relapse of the lesions after the HPSCT during follow-up (Fig. 2b).
DISCUSSION
This was a patient with recurrent bilateral lower extremity panniculitis. In his approach, it was crucial to exclude the possibility of an infectious source to exclude cellulitis; all cultures and stains were negative. Two biopsies indicated an abundant neutrophilic infiltrate, which led to the presumption of classic Sweet’s syndrome; however, the patient did not meet the necessary criteria for diagnosis. Classic Sweet’s syndrome is typically defined by the presence of two major criteria and two minor criteria [8]. Our patient did meet the two major criteria, which were the abrupt onset of tender nodules and a dense neutrophilic infiltrate in the biopsy. However, out of the four minor criteria, our patient only met one, which was the association with a hematologic disease. After excluding other potential diagnoses, we reached the conclusion of neutrophilic (lobular) panniculitis (NP). As mentioned earlier, NP has been associated with MDS. A study by Sutra-Loubet et al. demonstrated a strong association between NP and MDS. Out of the eight reported cases of NP, MDS was identified in six, that is, in 75% of the patients [2]. The mechanisms by which HPSCT induced remission of the lesions remain unknown. Nevertheless, we propose that the treatment of the underlying disease (in this case, MDS) may act as a protective factor against recidivism.
CONCLUSION
NP is a rare condition within the ND group, named lobular because the inflammation predominates in the fat lobules. Hematological malignancies should be investigated in patients in whom NP is found [9]. NP is a diagnosis of exclusion, and it must be known that overlapping is a frequent feature within the ND spectrum, making diagnoses even more difficult. The differentiation of NP from other NDs is relevant since there is no standardized protocol for its diagnosis or approach. Healthcare professionals may only consider the suspicion of this condition if they are familiar with it, which is why we believe the diffusion of these cases is so important.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki. The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal.
REFERENCES
1. Delaleu J, Lepelletier C, Calugareanu A, De Masson A, Charvet E, Petit A, et al. Neutrophilic dermatoses. Rev Med Interne. 2022;43:727-38.
2. Sutra-Loubet C, Carlotti A, Guillemette J, Wallach D. Neutrophilic panniculitis. J Am Acad Dermatol. 2004;50:280-5.
3. Ichiki T, Sugita K, Goto H, Shindo M, Yamamoto O. Localized pegfilgrastim-induced neutrophilic dermatosis with tissue G-CSF expression:A mimicker of Sweet’s syndrome. Acta Derm Venereol. 2019;99:685-6.
4. Becherer K, Golda N, Feldman M, Diaz-Arias A, Caldwell C. Neutrophilic panniculitis associated with myelodysplastic syndrome with abnormal nuclear forms. J Cutan Pathol. 2009;36:1024-6.
5. Qian L, Shen J, Cen J, Yin W, Ma Y. Myelodysplastic syndrome with neutrophilic panniculitis:A report of two cases and a literature review. Oncol Lett. 2015;9:1954-6.
6. Kim H, Youn H, Shin H, Yahng A, Lee E, Kwon C. Neutrophilic panniculitis following azacitidine treatment for myelodysplastic syndromes. Leuk Res. 2012;36:146-48.
7. Suzuki Y, Kuroda K, Kojima T, Fujita M, Iseki T, Shinkai H. Unusual cutaneous manifestations of myelodysplastic syndrome. Br J Dermatol. 1995;133:483-6.
8. Agrawal A, Arif SH, Kumarasan K, Janjua D. Sweet’s syndrome:An update. Curr Pediatr Rev. 2022;18:265-73.
9. Matsumura Y, Tanabe H, Wada Y, Ohta K, Okamoto H, Imamura S. Neutrophilic panniculitis associated with myelodysplastic syndromes. Br J Dermatol. 1997;136:142.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0006-3522-0806 http://orcid.org/0009-0006-3522-0806 http://orcid.org/0000-0003-3312-5953 http://orcid.org/0000-0003-3312-5953 |




Comments are closed.