Usefulness of ultrasonography in the assessment of skin lesions of cutaneous t-cell lymphoma
Hanna Cisoń 1, Zdzisław Wożniak2, Rafał Białynicki-Birula1
1, Zdzisław Wożniak2, Rafał Białynicki-Birula1
1Department of Dermatology, Wroclaw Medical University, Wroclaw, Poland, 2Department of General and Experimental Pathology, Wroclaw Medical University, Wroclaw, Poland
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Cutaneous T-cell lymphoma (CTCL) poses a challenge in terms of diagnosis and assessment of disease progression. High-frequency ultrasound (HFUS) is a non-invasive imaging modality used for evaluating dermal changes, including the assessment of infiltrative intensity in CTCL. HFUS encompasses the assessment of infiltrative intensity, visualization of tumor characteristics, and monitoring of disease progression and treatment response. By providing detailed and precise information regarding the affected skin layers, HFUS contributes to the diagnostic process and aids in the management of this complex disease. Herein, we present the case of a 79-year-old male diagnosed with mycosis fungoides (MF), whose disease was confirmed by HFUS examination during PUVA therapy.
Key words: Ultrasonography, Diagnostic imaging, CTCL, Mycosis fungoides, MF, Skin diseases
INTRODUCTION
Cutaneous T-cell lymphoma (CTCL) accounts for approx. 4% of all non-Hodgkin lymphomas and represents 75–80% of all primary cutaneous lymphomas [1]. It exhibits a male predominance, with a male-to-female ratio of 2:1 [2,3].
The incidence of CTCL rises with advancing age, with an average age at diagnosis ranging from 50 to 60 years old [3]. The etiopathogenesis of CTCL remains unclear. Several theories have been proposed, including viral infections such as Epstein–Barr virus (EBV) and human T-cell lymphotropic virus type 1 (HTLV-1), which may lead to a chronically dysregulated immune state. Genetic factors, such as specific human leukocyte antigen (HLA) types precisely the upregulation of HLA-G, in conjunction with the expression of interleukin-10 (IL-10) [4], as well as exposure to certain chemicals and medications, have also been implicated [5]. The cutaneous manifestations of CTCL may be patches papules, plaques, nodules, and/or tumors, which have the potential to ulcerate and undergo necrosis, leading to the formation of varioliform scars upon healing [6]. Approx. 10% of individuals with CTCL experience extracutaneous spread, indicating the involvement of organs or tissues beyond the skin.
High-frequency ultrasound (HFUS) is a non-invasive imaging technique employed for the evaluation of dermal alterations. Its utilization encompasses the assessment of infiltrative intensity in CTCL.
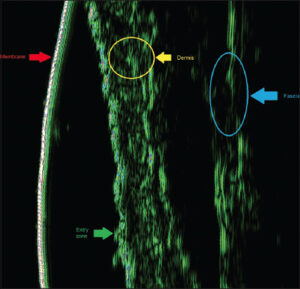
Skin sonographic examinations were conducted at the Department of Dermatology in Wroclaw using a taberna pro medicum (tpm) GmbH device manufactured in Lüneburg, Germany. The device operates at a frequency of 22.5 MHz. The transducer allows for tissue penetration up to a depth of 8 mm, offering a vertical (axial) resolution of 80 μm and a horizontal (lateral) resolution of 200 μm. For data acquisition and storage, the DUBmicro®tpm software was employed. This software facilitates the recording and storage of ultrasound data obtained during the examinations. Echogenicity measurements of structures were evaluated using both the A mode and B mode.
CASE REPORT
A 79-year-old male presented for the first time at the Department of Dermatology in Wrocław in 2018. At that time, he exhibited scattered, well-demarcated erythematous and scaling lesions on the skin of the upper and lower extremities, as well as the trunk. It was accompanied by pruritus (4/10 on the NRS scale). Treatment with PUVA (psoralen and UVA) (27 sessions) and clobetasol propionate ointment 0.5 mg/mL b.i.d led to partial improvement of the skin lesions. Laboratory tests revealed elevated levels of beta-2-microglobulin (2.62 mg/I, normal: 2.5 mg/l) and total IgE (3210 IU/mL, normal: 100 IU/mL).
During hospitalization in 2020, the treatment plan included the addition of subcutaneous methotrexate (20 mg/p.w.).
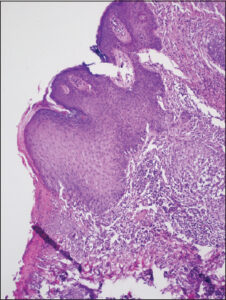
During hospitalization in January 2021, immunophenotyping of peripheral blood revealed CD4+/CD7-: 8%, CD4+/CD27-: 23.0%, and CD4+/CD8+: 1:4:1. Furthermore, the histopathological result of the temporal tumor biopsy obtained during the previous hospitalization indicated diffuse infiltration of lymphocytes, plasma cells, histiocytic cells, some neutrophils, eosinophils, and occasional multinucleated giant cells in the dermis. Elastolysis was observed. The lymphocyte population mainly consisted of CD3+ T cells, with very few CD20+ B cells. A relatively small number of cells expressed CD5 and CD7 (partial loss of expression), while scattered and small clusters of cells showed CD30 expression. CD68 expression was observed in numerous cells (macrophages), and MUM-1 expression was detected in several cells (Fig. 1). The histological findings in conjunction with the clinical presentation supported the diagnosis of MF. The diagnosis was once again confirmed by an immunohistochemical examination, which detected CD30+ cells in the epidermis as well as a Ki67 expression of 10%. Additionally, features of epidermotropism were observed, which may correspond to the progressive phase of MF. In January 2022, new erythematous and infiltrated lesions appeared. Peripheral lymph node ultrasonography did not reveal any abnormalities. The patient underwent treatment with bexarotene initiated in May 2022. Since then, the patient has been under the care of the dermatology clinic for completion of the mSWAT (modified Severity Weighted Assessment Tool) questionnaire, which is a requirement in the bexarotene program. In April 2023, the patient returned to the Department of Dermatology in Wrocław. Upon physical examination, diffuse erythematous and infiltrated lesions were observed on the cervical region, hairy scalp, trunk, and extremities (Figs. 2 and 3). These cutaneous manifestations were accompanied by prominent epidermal desquamation and xerosis. Notably, the affected areas on the hairy scalp exhibited follicular miniaturization.
Following the patient’s admission, a successive evaluation utilizing the mSWAT was undertaken. The score was 61. Subsequently, an HFUS examination was conducted.
The HFUS depiction of healthy skin showcased a conventional profile in accordance with the attributes commonly observed in a 79-year-old individual (Fig. 4).
The assessment of the patient’s cutaneous condition unveiled the presence of massive dermal infiltrates, accompanied by a notable augmentation in dermal thickness (Fig. 5).
Hematological consultation confirmed the compatibility of PUVA phototherapy with concurrent bexarotene chemotherapy. The total dose of phototherapy was 20.9 mJ/m2 during eighteen sessions resulting in favorable clinical outcomes.
DISCUSSION
HFUS represents a non-invasive and cost-effective diagnostic modality that finds application in the evaluation of dermatological treatments. Furthermore, HFUS exhibits potential in the monitoring of disease progression in specific dermatoses. This imaging technique offers valuable insights into the efficacy of interventions and aids in the assessment of tissue characteristics, facilitating a comprehensive understanding of the underlying pathophysiology and treatment response [7]. There are still only several reports in the literature on the investigation of CTCL’s patients with HFUS [7–11].
Yukun Wang et al. [8] conducted a study involving 26 patients, consisting of 2 individuals diagnosed with Sézary syndrome, 2 with folliculotropic mycosis fungoides (fMF), and 22 with the classical variant of mycosis fungoides (cMF). Among the cohort, a subgroup of 16 individuals presented with early-stage manifestations characterized by the presence of patches or plaques. Ultrasonographic examination revealed a subepidermal, hypoechoic band in these cases, with only three lesions at the plaque stage exhibiting partial extension into the superficial dermal layer. Conversely, in the advanced-stage group of seven patients with tumor formations, infiltrative changes involving the deep dermis or subcutaneous tissue were observed. Furthermore, notable observations were made in two instances of fMF lesions and one case of Sézary syndrome. These particular lesions exhibited distinctive features, including well-defined, subepidermal, hypoechoic bands accompanied by heterogeneous hypoechoic regions surrounding hair follicles in the dermal layer. Anita Mandawa et al. [9] conducted a retrospective multicenter study utilizing data from centers in Spain, Italy, India, and Chile to assess the ultrasonographic characteristics in patients with both B-cell and T-cell cutaneous lymphomas. HFUS was utilized for the evaluation of primary cutaneous lesions, consistently demonstrating dermal thickening across the entire cohort. The lesions exhibited a hypoechoic echotexture characterized by the absence of calcifications or central necrosis. Classification based on ultrasonographic features identified focal infiltrative, nodular, pseudonodular, and diffuse infiltrative patterns. Notably, T-cell lymphomas exhibited a higher propensity for diffuse infiltrative changes relative to the other discerned patterns.
Polanska et al. [10], used a 20 MHz HFUS probe to study MF patients and found SLEB thickness decreased with phototherapy, suggesting it could monitor treatment response.
According to research by Iris Wohlmuth-Wieser et al. [11], HFUS measured thicker skin in CTCL and psoriasis compared to AD patients.
CONCLUSIONS
In summary, HFUS is a valuable and non-invasive diagnostic tool for assessing skin conditions and dermatological treatments. It may also help monitor disease progression and treatment effectiveness in cutaneous lymphomas such as mycosis fungoides and T-cell lymphomas. HFUS is known for its ability to provide precise diagnostic information and track treatment responses in different stages and types of the lymphomas.
REFERENCES
1. Keto J, Hahtola S, Linna M, VäkeväL. Mycosis fungoides and Sézary syndrome:A population-wide study on prevalence and health care use in Finland in 1998-2016. BMC Health Serv Res. 2021;21:166.
2. Korgavkar K, Xiong M, Weinstock M. Changing incidence trends of cutaneous T-cell lymphoma. JAMA Dermatol. 2013;149:1295-9.
3. Rodd A, Ververis K, Karagiannis T. Current and emerging therapeutics for cutaneous t-cell lymphoma:Histone deacetylase inhibitors. Lymphoma. 2012;2012:290685.
4. Urosevic M, Willers J, Mueller B, Kempf W, Burg G, Dummer R. HLA-G protein up-regulation in primary cutaneous lymphomas is associated with interleukin-10 expression in large cell T-cell lymphomas and indolent B-cell lymphomas. Blood. 2002;99:609-17.
5. Mirvish JJ, Pomerantz RG, Falo LD Jr, Geskin LJ. Role of infectious agents in cutaneous T-cell lymphoma:Facts and controversies. Clin Dermatol. 2013;31:423-31.
6. Bagherani N, Smoller BR. An overview of cutaneous T cell lymphomas. F1000Res. 2016;5:F1000 Faculty Rev-1882.
7. Levy J, Barrett DL, Harris N, Jeong JJ, Yang X, Chen SC. High-frequency ultrasound in clinical dermatology:A review. Ultrasound J. 2021;13:24.
8. Wang Y, Niu Z, Liu J, Zhu Q, Liu Z, Liu Y, et al. Value of high-frequency ultrasound in accurate staging of mycosis fungoides/Sézary syndrome. J Ultrasound Med. 2020;39:1927-37.
9. Mandava A, Koppula V, Wortsman X, Catalano O, Alfageme F. The clinical value of imaging in primary cutaneous lymphomas:Role of high resolution ultrasound and PET-CT. Br J Radiol. 2019;92:20180904.
10. Polańska A, Dańczak-Pazdrowska A, Olek-Hrab K, Osmola-Mańkowska A, Bowszyc-Dmochowska M, Żaba R, et al. High-frequency ultrasonography:New non-invasive method in assessment of skin lymphomas. Skin Res Technol. 2018;24:517-21.
11. Wohlmuth-Wieser I, Ramjist JM, Shear N, Alhusayen R. Morphologic features of cutaneous t-cell lymphomas using dermoscopy and high frequency ultrasound. J Clin Med. 2020;10:17.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3901-8876 http://orcid.org/0000-0003-3901-8876 http://orcid.org/0000-0001-6735-8494 http://orcid.org/0000-0001-6735-8494 http://orcid.org/0000-0002-2603-4220 http://orcid.org/0000-0002-2603-4220 |







Comments are closed.