Chronic leg ulcers in Senegal: Epidemiological and etiological study on 154 cases
Saër Diadie , Moussa Diallo, Patrick Mendy, Ibrahima Diokhané, Mamadou Sarr, Niar Ndour, Boubacar Ahy Diatta, Mame Thierno Dieng, Suzanne Oumou Niang
, Moussa Diallo, Patrick Mendy, Ibrahima Diokhané, Mamadou Sarr, Niar Ndour, Boubacar Ahy Diatta, Mame Thierno Dieng, Suzanne Oumou Niang
Dermatology of Aristide Le Dantec Hospital, Cheikh Anta Diop University of Dakar, Senegal
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Our aim was to establish the epidemiological and etiological profile of chronic leg ulcers (CLUs) in Senegal.
Methodology: We conducted a retrospective, descriptive, analytical study at the Dermatology Department of Aristide Le Dantec University Hospital Center (HALD) in Dakar from January 2008 to January 2018 (10 years). Data was entered in Excel and analyzed with Epi Info 7.
Results: We recorded 154 cases. The sex ratio was 1.75. The main causes were vascular in 69 cases (44.8%), infectious in 29 (18.8%), and sickle cell disease in 15 (9.7%). Etiology has not been identified in 23 patients (15.1%). Vascular origin was venous in 64 cases (92% of vascular causes) without any statistical link with sex (p = 0.408), arterial in 3 (4%), and mixed in 2 (3%).
Conclusion: In Senegal, LCUs are predominantly observed in young males. Causes are dominated by venous insufficiency, followed by infection.
Key words: Chronic leg ulcer, Venous insufficiency, Senegal
INTRODUCTION
Chronic leg ulcer (CLU) is a major concern for dermatologists because of its frequency and difficulty in management [1,2]. In Europe, it affects older women, in contrast to younger patients in Africa, who are predominantly male [2–4].
In addition to causing a considerable deterioration of the quality of life, treatment is expensive, estimated on average at 10,000 EUR per person per year in direct and indirect costs [5]. Its causes are multiple and dominated by venous insufficiency in the European population and recently in Africa [1–5]. In the context of a change in the etiological profile of CLUs in this area [2–4], we considered it appropriate to pursue the aim of determining the new epidemiological and etiological profiles of CLU in Senegal.
METHODOLOGY
We conducted a retrospective, descriptive, analytical study at the Dermatology Department of Aristide Le Dantec University Hospital Center (HALD) in Dakar from January 2008 to January 2018 (10 years). This service is the reference structure for skin pathologies in Senegal. We included all records of patients followed for chronic ulcers between the knee and ankle progressing for at least six weeks [6]. Investigations for etiological purposes were oriented by the clinic. Data was entered in Excel and analyzed with Epi Info 7.
RESULTS
Epidemiological and Clinical Aspects
We recorded 154 cases, with an annual frequency of 15.4 cases. These represented 0.2% of consultants and 3.8% of hospitalized patients during the period. The sex ratio (male-to-female) was 1.75. Fifty cases (32.4%) were sellers, 17 were housewives (11%), and 16 were teachers (10%). The other most represented professions were workers in 6 cases (3.89%), and military and agricultural professions in 4 cases (2.59%) each. The average duration of ulcer development was thirty months (2 months to 28 years). The ulcer was in the right leg in 53 patients (33%) and in the left leg in 75 patients (49%). It was bilateral in 26 patients (18%). Regarding number, the ulcer was single in 101 patients (64%) and multiple in 53 patients (35%), including 26 unilateral cases (17%).
Etiology of Ulcers
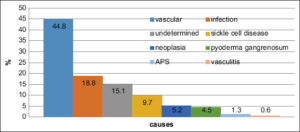
Causes were vascular in 69 cases (44.8%), infectious in 29 (18.8%), and sickle cell disease in 15 (9.7%). Pyoderma gangrenosum was observed in seven patients (4.5%) and neoplasia in eight (5.2%). Antiphospholipid syndrome (APS) was found in two patients (1.3%) and vasculitis in one female (0.6%). Etiology was not identified in 23 patients (15.1%) (Fig. 1).
Vascular ulcers were observed predominantly in males (69%), with a mean age of 44 years and living in urban areas. Vascular origin was dominated by venous insufficiency in 64 cases (92% of vascular causes), which was unrelated to sex (p = 0.408). Arterial disease was the cause in three patients (4%). Origin was mixed in two patients (3%).
Venous ulcers occurred in all sellers in the sample (n = 50), six housewives, four from the military personnel, three workers, and one farmer (Figs. 2a and 2b). The ulcer was located on the left leg in 21 patients (32%), and bilaterally in 18 (25%). Ulcers were mostly single (61%). Ochre dermatitis was found in 20 patients (31%). Varicose veins and edema of the lower extremities were found in 19 (29%) and 15 (23%) patients, respectively. Doppler ultrasonography, performed in 68 patients, detected superficial and deep venous damage in 42 patients (65%) and 4 patients (6%), respectively. The two territories were affected in 7 patients (10%).
Sickle cell disease was the cause in 15 patients (12%), among whom 11 cases were the homozygous form (SS). The sex ratio was 1.1. The 16–40 age group was the most represented (80%). The ulcer was the circumstance of discovery of sickle cell disease in nine cases.
Infectious causes were represented by necrotizing bacterial dermo-hypodermatitis (NBHD) in 22 cases, ecthyma in three, ecthyma gangrenosum in two. Other causes were one case of a Buruli ulcer in an eighteen-year-old male and one case of leishmaniasis.
Neoplastic ulcers were due to squamous cell carcinoma in 6 patients (75% of neoplastic causes). We noted one case of leg-type B lymphoma in a 71-year-old patient and extra-nasal TNK lymphoma of the leg in a 47-year-old patient.
DISCUSSION
We reported a series of 154 cases of CLU over a ten-year period. It provided information on the frequent occurrence in young patients, mostly male, and the predominance of vascular causes dominated by venous insufficiency.
In Africa, the occurrence of CLU is usually reported in young males. A series in sub-Saharan Africa and the Maghreb noted a preferential occurrence in males (60–64%) aged between 33 and 38 years [2,7–9]. This was in contradiction with results in the European population, in which the disease was the exclusive domain of older women. Several European studies have shown an increasing frequency of CLU with age [10]. In London, the prevalence is estimated at 0.045% in the general population, while it is 0.33% in subjects aged 65–74 years, 0.52% in subjects between 75–84 years of age, and 1.64% in subjects older than 85 years [10]. The same was noted in Spain, Australia, where the peak frequency was observed at 75 years old [11,12]. In the United Kingdom and Brazil, CLU occurs in females aged between 73 and 64 years, respectively [10,13]. The early occurrence of the disease in Africa could be explained by the youth of the population and the frequency of the hemoglobin disease, unlike in the European series [9,11,12]. Moreover, the delay in managing the risk factors of CLUs secondary to poverty and the lack of medical coverage is one of the reasons for its early occurrence in Africa.
In Senegal, CLUs are predominantly of vascular origin (44.8%) and dominated by venous insufficiency. This is similar to the etiologic profile in industrial countries.
In the Maghreb and in most series from sub-Saharan Africa, the predominance of vascular causes was clearly established [4,8,11,13,14], except in Mali, where CLUs were mainly due to infectious origin (67.8%) and dominated by necrotizing bacterial dermo-hypodermatitis. They were also the main infectious causes in our series yet corresponded to the second etiological group [9].
Unknown causes were noted in 15.1%. Neoplastic origin was dominated by squamous cell carcinoma, which is the first skin cancer of phototype VI with a preferential location on the leg [15].
CONCLUSION
CLUs are common reasons for hospitalization in dermatology in Senegal, where they predominate among young males. Causes are dominated by venous insufficiency, followed by necrotizing bacterial dermo-hypodermatitis.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Haute autoritéde santéRecommandations pour la pratique clinique Prise en charge de l’ulcère de jambe àprédominance veineuse hors pansement. Argumentaire juin 2006 P20.
2. Benchikhi H. Ulcère de jambe au Maghreb:résultats préliminaires d’une enquête multicentrique. Ann Dermatol Venereol. 2003;130:29.
3. EL Fekih N, Chtourou O, Fazaa B, ZouarI B, Kamoun M. Particularités épidémioclinique des ulcères de jambe en Tunisie, àtravers une série Hospitalière. Ann Dermatol Venereol. 2005;132:182.
4. Vasileva M, Brishkoska Boshkovski V, Drakalska Sersemova E. Comorbidities as prognostic factors in the healing of venous ulcers. Our Dermatol Online. 2023;14:177-9.
5. Purwins S. Purwins S, Herberger K, Debus ES, Rustenbach SJ, Pelzer P, et al. Cost-of-illness of chronic leg ulcers in Germany. Intern Wound J. 2010;7:97-102.
6. New Zealand Guidelines Group, Royal New Zealand College of General Practitioners, College of Nurses. Care of people with chronic leg ulcers. An evidence-based guideline 1999. [Consultéle 19-03-2017].
7. CisséF. Ulcères chroniques des membres inférieurs:Possibilitédiagnostique et thérapeutique. Thèse Med Bamako. 1990:N°74.
8. Souissi A, Ben Tekaya N, Youssef M, Cherif F, Mokni M, El Euch D, et al. [Leg ulcers:clinical and epidemiological study of hospital patients in Tunis]. Ann Dermatol Venereol. 2005;132(12 Pt 1):1010-2.
9. Traore I. Ulcères chroniques des membres inférieurs au C.N.U.A.M. de Bamako:115 cas. Thèse med Bamako. 2013;N°19.
10. Moffatt C. Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. QJM. 2004;97:431-7.
11. Berenguer Pérez M, López-Casanova P, Sarabia Lavín R, González de la Torre H, Verdú-Soriano J. Epidemiology of venous leg ulcers in primary health care:Incidence and prevalence in a health centre:A time series study (2010–2014). Int Wound J. 2019;16:256-65.
12. Baker S. Stacey M, Singh G, Hoskin S, Thompson P. Aetiology of chronic leg ulcers. Eur J Vasc Surg. 1992;6:245-51.
13. Frade M, Cursi I, Andrade F, Soares S, Ribeiro W, Sandro V, et al. Úlcera de perna:um estudo de casos em Juiz de Fora-MG (Brasil) e região;Investigação clínica, epidemiológica, laboratorial e terapêutica. An Bras Dermatol. 2005;80:41-6.
14. Andreas K, Andreas K, Joachim K, Samy A, Caroline W, Dirk S, et al. Etiology of chronic leg ulcers in 31,619 patients in Germany analyzed by an expert survey. JDDG;2011;9:116-21.
15. Dieng MT, Diop NN, Déme A, Sy TN, Niang SO, Ndiaye B. [Squamous cell carcinoma in black patients:80 cases]. Ann Dermatol Venereol. 2004;131:1055-7.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-9770-1118 http://orcid.org/0000-0001-9770-1118 http://orcid.org/0000-0002-8245-6372 http://orcid.org/0000-0002-8245-6372 http://orcid.org/0000-0003-4550-3704 http://orcid.org/0000-0003-4550-3704 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0001-8923-0790 http://orcid.org/0000-0001-8923-0790 |





Comments are closed.