Characterization of isolated and integrated clinical and dermoscopic features of topical steroid-dependent/damaged face: A study from central India
Sanskriti Chauhan , Rochit Singhal, Vivek Choudhary, Shyam G Rathoriya
, Rochit Singhal, Vivek Choudhary, Shyam G Rathoriya
Department of Dermatology Venereology and Leprosy, Chirayu Medical college & Hospital, Bhopal (MP), India
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Topical steroid-dependent/damaged face (TSDF) is defined as semi-permanent or permanent damage to the skin of the face due to unsupervised or prolonged application of topical corticosteroids to the face. Dermoscopy is widely practiced as a non-invasive, effective technique to analyze the immediate or delayed features of TSDF.
Objectives: The objective was to evaluate the clinical profile along with dermoscopic features of clinically diagnosed cases of TSDF.
Materials and Methods: The study was conducted on seventy-five patients attending the Department of Dermatology, Venereology, and Leprosy between April 2021 and September 2022 with clinical symptoms and signs suggestive of TSDF. Thorough history taking, clinical evaluation, and dermoscopic examination were performed, and data was recorded in a structured proforma with a sixteen-point questionnaire.
Results: Sixty-eight percent of the patients were females, yielding a female-to-male ratio of 2.1:1. The most frequently affected age group was 26–35 years (48%), with a mean age of 31.8 years. The most common topical steroid employed was beclomethasone dipropionate 0.25% (33.33%), followed by clobetasol propionate 0.05% (29.33%). The most common clinical findings observed were erythema with hyperpigmentation (74.66%), followed by erythema with telangiectasia (34.66%). The most often observed dermoscopic findings were red, diffuse areas with vessels (61.33%), red, diffuse areas with an exaggerated pigment network (52%), and clustered vellus hairs with white vellus hair (44%).
Conclusion: Topical corticosteroids are commonly abused drugs seen in modern clinical practice, resulting in a plethora of symptoms and creating a paramount dermatological concern. Dermoscopy plays a cardinal evaluating role in the early discernment and establishment of TSDF besides determining the gravity of damage.
Key words: Topical steroid-dependent/damaged face (TSDF), Topical corticosteroids, Dermoscopy
INTRODUCTION
The landmark of the modern era of dermatotherapy was set in 1952 with the revelation of the first topical corticosteroids (TCs) by Sulzberger and Witten [1]. Topical corticosteroids have beneficial anti-inflammatory, immunosuppressive, anti-pruritic, and vasoconstrictive actions; on the other hand, their melanopenic and atrophogenic actions have proved to be a double-edged sword. The face is the most common site of TC use for various equitable and illicit indications, hence becomes the most common site of misuse. Prolonged and recurrent TC application to the face results in steroid addiction, causing a phenomenon of cutaneous damage known as topical steroid-dependent/damaged face (TSDF) [2].
TSDF is defined as permanent or semi-permanent damage to the facial skin caused by unsupervised, prolonged, indiscriminate, and irrational use of topical corticosteroids on the face for a multitude of ailments, pertaining to its potent and rapid anti-inflammatory action on the skin [3].
The use of TCs on the face produces a constellation of signs and symptoms, such as acneiform eruption, facial hypertrichosis, cutaneous atrophy, and demodicosis, whose treatment becomes a battle for both the patient and the dermatologist. Although, early subtle changes of steroid-induced damage to the face may not be visible initially with the bare eye, yet there is a need for the early identification of the marked signs of TSDF before they become clinically apparent and eventually progress reversibly or irreversibly.
Dermoscopy or epiluminescence microscopy is a non-invasive imagining technique that was first used by Lean Goldman in the 1950s to evaluate melanocytic nevi and melanomas. It is a rapid and effective technique of analyzing various dermatological conditions and helps to visualize various layered and subsurface skin structure changes comprehensively. Dermoscopy may also be employed for the visual identification of immediate and delayed features of TSDF by observing characteristic dermoscopic features, such as polygonal vessels and telangiectasias, erythema, structureless, white areas, hypertrichosis, and scales, as well to monitor the patient’s compliance to treatment with serial evaluation [4].
The present study was conducted due to limited previous studies despite tremendous injudicious use of topical corticosteroids among the general population, to gain proficiency in detecting the earliest changes of TSDF, and to bring awareness regarding the mishaps of unrestricted availability and consumption of over-the-counter topical steroids.
OBJECTIVES
The present study was conducted to assess the clinical profile of patients presenting with TSDF, encompassing the indications and potency of TCs, and to evaluate and correlate the dermoscopic features of TSDF.
MATERIALS AND METHODS
A hospital-based, observational, cross-sectional study was conducted on seventy-five patients attending the Department of Dermatology, Venereology, and Leprosy between April 2021 and September 2022 after taking approval from the institutional ethical committee. After taking written informed consent, patients aged eighteen years and above with clinical symptoms and signs suggestive of TSDF, including redness, burning, itching, photosensitivity, atrophy, and pigmentation, and with a history of the application of topical corticosteroids to the face for a period of more than one month were enrolled in the study. Patients taking oral corticosteroids and with pre-existing comorbidities such as polycystic ovarian syndrome, Cushing’s syndrome, and pregnancy were excluded from the study.
Demographic details including age, sex, occupation, education, marital status, and details of TC application, including duration, frequency, cause of application, and source of recommendation, were documented in a preformed questionnaire containing sixteen questions. After elaborate clinical history taking, cutaneous examination was done on all patients. Dermoscopic examination was done by DINO-LITE™ Premier Digital Microscope (AM4113/AD4113) with polarized light, and findings were captured by Dinocapture 2.0 and analyzed. The collected data was tabulated and described in terms of descriptive statistics and frequency with SPSS and Microsoft Excel.
RESULTS
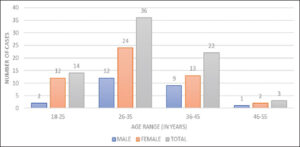
A total of seventy-five patients with TSDF were enrolled, with 24 (32%) males and 51 (68%) females, giving a female-to-male ratio of 2.1:1. Young and middle-aged adults comprised the most common age groups affected (77.33%), with a mean age of 31.8 years (Fig. 1).
A majority of the patients were educated (81.3%) and aware of their condition and the related possible reasons. Thirty-five percent knew that the withdrawal of such causative agents/topical agents would improve their current problem. A majority of the enrolled patients were housewives (45.33%), while fieldworkers constituted 18.66%, skilled workers 13.33%, manual laborers 12%, and students 10.66%. A significant number of the patients presented with redness (62.66%), followed by burning (52%), itching (44%), pigmentation (36%), acne (38.66%), photosensitivity (25.33%), dryness (16%), and increased facial hair (10.66%). These isolated complaints were exclusively recorded with the subsequent inclusion of features in the individual as well as a combination basis with the exclusion of the previous indication of use.
Almost all patients employed a combination formulation of TCs with other agents (96%), while few (4%) employed TCs as monotherapy, most probably due to the easy and affordable over-the-counter availability. The most frequently used combination therapy was betamethasone valerate 0.1% and neomycin sulphate 0.5% in 17.33% of the cases. Around 70% of the patients stuck to one TC for the whole duration of the application, whereas the rest of the patients switched to more than one type of TC. The TC switch was interestingly observed from high to low potency, and it was betamethasone valerate to mometasone furoate (9.33%), followed by clobetasol propionate to beclomethasone dipropionate (6.66%).
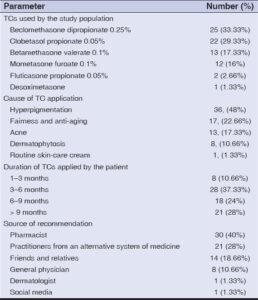
The most common topical steroid used was beclomethasone dipropionate 0.25% (33.33%), followed by clobetasol propionate 0.05% (29.33%). These were used because of their frequent occupancy among the topmost combination corticosteroid formulations on the market and the relatively higher potency that eases isolated or combined induced ailments on the face. The most frequent indication for which steroids were used by the patients was hyperpigmentation (48%), followed by fairness cream (22.66%). This was usually due to an increased aesthetic concern among the affected age group (Table 1). A majority of the patients (37.33%) used TCs for 3–6 months and the source of recommendation for TC use was the pharmacist (40%). Surprisingly, social media played an imperceptible role (1.33%), contrary to preconceived notions about its role in the existing times (Table 1).
Clinical Features of TSDF
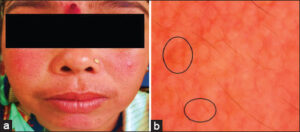
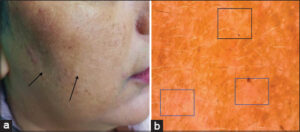
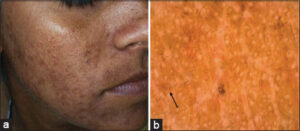
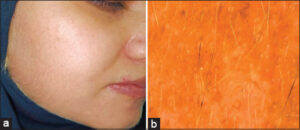
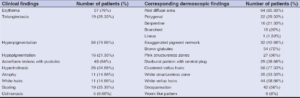
The most common clinical findings in TSDF were erythema with hyperpigmentation (74.66%), followed by erythema with telangiectasia (34.66%) (Fig. 2), acneiform lesions (Figs. 3 and 4) with hypertrichosis (25.33%) (Fig. 5), and hypopigmentation with hyperpigmentation (21.33%) (Fig. 3). These features were a blend of diverse, correlated presenting complaints and use indications as unaided afflictions were thin on grounds in the real-time scenario.
Dermoscopic Features of TSDF
The most common dermoscopic findings were red, diffuse areas with an exaggerated pigment network (61.33%), red, diffuse areas with vessels (52%) (Fig. 2b), and clustered vellus hairs with white vellus hair (44%) (Fig. 5), followed by clustered vellus hair with desquamation (33.33%) observed in a statistically higher proportion of cases dermoscopically. The most frequently observed vessels were polygonal (40%) (Fig.2b), serpentine (29.62%), branched (27.77%), and linear (1.85%). The appearance of white vellus hair on dermoscopy was seen in patients using topical steroids mainly for melasma (30%). The visibility of vellus hair was increased twofold upon dermoscopy; in contrast, the peculiar dermoscopic features of acneiform eruption were reduced to 60%. The corresponding dermoscopic features were out of proportion with the majority of individual morphological features, such as erythema, telangiectasia, and hyperpigmentation, while they were equivocal in ochronosis and hypopigmentation and smaller in acneiform lesions. This disparity was shortened to a remarkable scale by analyzing these features in an integrated approach. Thus, we were able to comprehend the real-time ailments of the patients in a problem-solving manner and on an authentic framework. Table 2 sums the isolated clinical and dermoscopic features, while Figs. 2 – 5 show clinical images with corresponding dermoscopic images.
DISCUSSION
The face is the most visible subunit of the human body, making it the most prominent part aesthetically. Environmental factors such as UV rays, dust, pollution, and injudicious use of a multitude of cosmetics and medicated topicals make facial skin more vulnerable to these detrimental effects. Any minor change makes the patient anxious, and they frequently seek for a cure. Topical corticosteroid misuse is a daunting concern globally as multiple countries face the same nuisance [5]. A majority of people have a common perception that the pharmacist has knowledge about most of the ailments. On top of it, the rampant sale of over-the-counter medications leads to the expanding contingencies of such formulations. This never-ending chain of demand and supply with the apprehensive nature of facial concern and reluctancy on the patient’s part to realize the adverse effects of TCs has led to the vicious cycle.
TC abuse produces complex symptoms of copious side effects, that is, steroid acne, steroid atrophy, and telangiectasia, occurring due to unrestrained use of TCs, leading to an increased molecular threshold, eventually leading to drug dependence. When initially TCs are applied, they cause vasoconstriction, which on withdrawal, leads to fixed vasodilatation, being responsible for the rebound effect seen after TC withdrawal [3]. According to Rapaport, the constant application of TCs inhibits the effect of nitric oxide causing chronic vasoconstriction, which on withdrawal, leads to the release of endothelial nitric oxide, inducing vasodilatation with subsequent erythema [6], and abnormal dilatation of capillaries ensues the formation of telangiectasias.
In the age distribution pattern, we found that almost half of the studied population was in the age group of 26–35 years (48%) and 36–45 years (29.33%). A similar age-specific representation was reflected in a study by Nyati et al. on 670 patients, in which 48.20% were in the 21–30 year age range, followed by 31–40 years (25.22%) [7]. The possible reason might have been their consciousness toward appearance due to the acquisition of marriageable age, beginning a career, and participation in society and social media much more actively.
A female predominance (68%) was noted in our study, which was in concordance with the study by Manchanda et al. in which 70% of 100 patients were females [8], which may be explained by a higher cosmetic concern as well as the societal stigma of ideal presentation among females.
In the present study, 81% of the cases were educated, which coincided with the study by Surya et al. in which 78% of patients were educated [9]. This contradicted their ideal representation among society vs. the time-based altered perception of cosmetic use and concern. The most common presenting complaints after TC abuse were redness (62.66%), followed by burning (52%), itching (44%), pigmentation (36%), and acne (38.66%). Meanwhile, Dey observed acne (37.99%), followed by plethoric face, and telangiectasia (18.99%) as the most frequent adverse effects after TC abuse [10].
The most commonly abused TC was beclomethasone dipropionate 0.25% (33.33%), followed by clobetasol propionate 0.05% (29.33%), which was in collision with the study conducted by Surya et al. on 189 patients, among whom betamethasone valerate (34%) was found to be the most common topical steroid used, followed by mometasone furoate (28%) [9]. The discordance could be attributed to the area-specific availability and unregulated dispense of preparations with subjective reference to the particular agent.
The longest duration for which topical steroids were used in our study was less than six months (47.99%), followed by more than nine months (28%). These findings were mirrored in an Indian study by Ambika et al., in which 55% of patients used topical steroids for less than six months [11]. These co-occurrences were not merely destined yet to designate the peak point of acceptability with the eventual emergence of symptoms afterward.
Topical steroids have transpired as major skin lighteners owing to their bleaching action and possibly due to their anti-inflammatory activity, which curtails the risk of dermatitis [12]. We found pigmentation (48%), followed by fairness and anti-aging creams (22.66%), as the most frequent indication for which steroids were used and these findings differed from the study by Saraswat et al., in which 249 out of 433 patients used TCs for acne alone [13].
We found that pharmacists (40%) constituted the largest number of sources of prescription followed by practitioners from an alternative system of medicine (28%), which was in unanimity with a study by Pal et al. in which 39.85% of patients had the pharmacist as their most common source of recommendation, followed by friends or relatives (30.25%) [14].
Erythema (76%), followed by hyperpigmentation (74.66%) and acneiform lesions with pustules (64%), were the most common clinical findings in the present study. On dermoscopic evaluation, red, diffuse areas (85.33%) were the most consistent finding, followed by clustered vellus hairs (77.33%), with an equal number of vessels and brown globules in 72%. This was in harmony with a study by Sethi et al., in which erythema (81.1%), followed by hyperpigmentation (80.3%) and hypertrichosis (68.2%), were the common clinical findings, whereas dermoscopically, it was brown globules (96.2%), followed by red, diffuse areas (92.4%) and vessels (87.1%) [15].
In our study, we also witnessed the unique observation that erythema (33%), followed by hypopigmentation (21%), were the first to recede on dermoscopic examination while withdrawing steroids.
We employed a questionnaire containing sixteen questions to assess the prior knowledge of the patient about the effects due to misuse of TCs and their attitude toward its further use after learning about the adverse effects. We observed that 66.66% of the patients did not have previous knowledge about the adverse effects of the misuse of TCs. However, after the implementation of a questionnaire with added education and counseling, 98.6% of the patients became well-versed with the mishaps of TCs, while 96% showed a positive attitude toward avoiding such topical preparations, and 94.6% were disinclined to the use of the culprit TCs in the future and committed to follow good practices that we offered.
We believe that the impairments and late sequels owing to TC abuse are not merely meager innoxious manifestations yet complex series of activities being sequentially expressed on the facial surface and subsurface in accordance to the precise timespan of contact to specific TCs with idiosyncratic potencies.
The present study provided isolated and consolidated clinical and dermoscopic features, and such compendious information has not been published earlier. We experienced that integrated clinical and dermoscopic findings were more pivotal as the patients presented with more than one complaint at any particular given point in time. Also, the combined features, although superimposed, were elementarily recognized both clinically and dermoscopically. With an adequate regimen, a decrease in prominent vessels, scaling, hypertrichosis, white hair, and red, diffuse areas would be expected, and the analogous dermoscopic changes may also be serially analyzed.
CONCLUSION
Topical corticosteroids are misused on the face for numerous dermatological conditions such as acne, hyperpigmentation, and even for the purpose of general fairness creams and bleaching agents. Our study highlighted the onus of facial topical steroid misapplication and the elements contributing to the poor attitude toward TCs. Dermoscopy of TSDF may help in a multitude of ways, from validating the diagnosis to predicting the stretch of TC abuse. Furthermore, it may also help in forecasting disease severity, thus explaining abysmal consequences to the patient in all possible ways. As medical professionals, we may further develop multifaceted therapeutic options available on the basis of the integrated clinical and dermoscopic findings. The education of the general population by increasing awareness and providing pamphlets on the adverse effects of TC misuse may also be an important step to prevent this hazard. The enforcement of strict laws on the sale of over-the-counter topical corticosteroids and prescribing physicians to put forth such molecules for further prevention of this epidemic is the need of today’s time. In the future, the substantial exploration of corresponding studies is vindicated to increase the confrere’s knowledge on this intense subject considering its huge impact on dermatologists as responsible citizens.
Study Limitations
Histopathological correlation of the present subjects along with a series of follow-up evaluations could not have been done. Also, the clinical and dermoscopic assessment of the individual potency based topical corticosteroid molecule was deficient in our study.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19:101-2.
2. Coondoo A. Topical corticosteroid misuse:The Indian scenario. Indian J Dermatol. 2014;59:451-5.
3. Lahiri K, Coondoo A. Topical steroid-dependent face (TSDF):An entity of cutaneous pharmacodependence. Indian J Dermatol. 2016;61:265-72.
4. Tatu AL. Topical steroid induced facial rosaceaiform dermatitis. Acta Endocrinol (Buchar) 2016;12:232-3.
5. Lu H, Xiao T, Lu B, et al. Facial corticosteroid addictive dermatitis in Guiyang City, China. Clin Exp Dermatol. 2010;35:618-21.
6. Rapaport MJ, Rapaport V. The red skin syndromes:Corticosteroid addiction and withdrawal. Expert Rev Dermatol 2006;1:547-61.
7. Nyati A, Singhal AK, Yadav D, Sharma MK. Topical steroid abuse on face:A prospective study from a tertiary care centre of north India. Int J Res Dermatol 2017;3:433-8.
8. Manchanda K, Mohanty S, Rohatgi PC. Misuse of topical corticosteroids over face:A clinical study. Indian Dermatol Online J. 2017;8:186-91.
9. Ravindran S, Prabhu SS, Nayak SU. Topical steroid damaged skin:A clinic-epidemiological and dermatological study. J Pak Assoc Dermatol. 2022;31:407-14.
10. Dey VK. Misuse of topical corticosteroids:A clinical study of adverse effects. Indian Dermatol Online J 2014;5:436-40.
11. Ambika H, Vinod CS, Yadalla H, Nithya R, Babu AR. Topical corticosteroid abuse on the face:A prospective study on outpatients of dermatology. Our Dermatol Online. 2014;5:5-8.
12. Mahe A, Ly F, Aymard G, Dangou JM. Skin diseases associated with the cosmetic use of bleaching products in women from Dakar, Senegal. Br J Dermatol. 2003;148:493-500.
13. Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face:A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
14. Pal D, Biswas P, Das S, De A, Sharma N, Ansari A. Topical steroid damaged/dependent face (TSDF):A study from a tertiary care hospital in Eastern India. Indian J Dermatol. 2018;63:375-9.
15. Sethi S, Chauhan P, Jindal R, Bisht YS. Dermoscopy of topical steroid-dependent or damaged face:A cross-sectional study. Indian J Dermatol Venereol Leprol. 2022;88:0-6.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0007-1620-4365 http://orcid.org/0009-0007-1620-4365 http://orcid.org/0009-0004-3409-3206 http://orcid.org/0009-0004-3409-3206 http://orcid.org/0009-0001-3561-6505 http://orcid.org/0009-0001-3561-6505 http://orcid.org/0009-0009-9090-1083 http://orcid.org/0009-0009-9090-1083 |




Comments are closed.