Cutaneous tuberculosis: A series of 10 cases collected at the Dermatology-Venereology Department of the Treichville University Hospital Center
Georgies Steve Tameu Tchomdom 1, Koffi Kouame Pacôme Gbandama1, 2, Ulrich Nguena Feungue1, Kouadio Célestin Ahogo1, 2
1, Koffi Kouame Pacôme Gbandama1, 2, Ulrich Nguena Feungue1, Kouadio Célestin Ahogo1, 2
1Dermatology and Venerology Department, University Teaching Hospital of Treichville, 01 BPV R03 Abidjan 01, Ivory Coast, 2Medical Sciences Training and Research Unit of Abidjan, Félix Houphouët-Boigny University, Ivory Coast
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Cutaneous tuberculosis is a rare and under-diagnosed localization of tuberculosis due to its anatomo-clinical polymorphism and the infrequent isolation of mycobacteria. The general objective of our study was to identify its epidemiological, clinical, paraclinical, and evolutive particularities in our working environment.
Methods: We conducted a prospective study of case series from January 2019 to July 2022. Any patient presenting suggestive clinical signs of cutaneous tuberculosis, as well as a histological and/or biological confirmation, was included.
Results: Out of 26024 patients consulted, 10 cases of cutaneous tuberculosis were identified (0.03%), with a male predominance (M/F ratio of 9). The average age of the patients was 24 years, with an interquartile range of 23 years and extremes of 5 and 57 years. The main clinical forms identified were scrofulodermas (7 cases). We noted three exceptional cases in which several clinical forms were associated: gummas and verrucous tuberculosis, scrofulodermas and gummas, and scrofulodermas, gummas, and verrucous tuberculosis. Histopathology of skin fragments showed tuberculoid granuloma associated with caseous necrosis in 100% of the cases. Auramine staining found AFB in 67% while PCR revealed Mycobacterium tuberculosis in 85.71%. HIV serology was negative in all patients.
Conclusion: Cutaneous tuberculosis in Abidjan is dominated by multibacillary forms, namely gums and scrofuloderma such as other series in the West African subregion. The negativity of HIV serology in all our patients raises the question of the link between cutaneous tuberculosis and HIV as well as the favoring factors of cutaneous tuberculosis in our context.
Key words: Abidjan, Ivory coast, Epidemiology, Cutaneous tuberculosis
INTRODUCTION
Tuberculosis is an infectious, chronic, and contagious disease of primarily human-to-human transmission caused by Mycobacterium tuberculosis or Koch’s bacillus (BK) [1]. It is the second most common infectious disease in the world after HIV infection and the leading cause of death. In 2019, its global incidence was estimated at 10 million people and the number of related deaths was 1.2 million [2]. In Ivory Coast, 36,000 cases of cutaneous tuberculosis (cTB) were reported in 2014, and in a meta-analysis of hospital-based studies, the proportion of extra-pulmonary tuberculosis (EPT) ranged from 16% to 50% with lymph node and pleural forms predominating [3]. However, the cutaneous location of the disease remains rare and difficult to diagnose due to its anatomical-clinical polymorphism, which is the source of a multitude of differential diagnoses and patient wandering [4–7]. Based on this observation, we conducted this study with the aim of studying the epidemiological, clinical, paraclinical, and evolutionary particularities of cutaneous tuberculosis in Abidjan.
METHODOLOGY
This was a prospective case series study of all cases of cTB diagnosed in patients who consulted the Dermatology-Venerology Department of the University Hospital Center of Treichville between January 2019 and July 2022. Our study included patients presenting clinical signs suggestive of cTB associated with a paraclinical confirmation performed on a skin sample. The elements that allowed for this paraclinical confirmation were the presence of Mycobacterium tuberculosis on GEN XPERT® MTB/RIF skin samples (ulceration or pus) and/or the visualization of acid-fast bacilli (AFB) after staining with Auramine and/or the presence of a tuberculoid gigantocellular granuloma on histopathological examination. For each patient, epidemiological (age, sex), clinical (time to disease progression, clinical form), paraclinical (results of tuberculin tests, bacteriological skin samples, skin histology, chest X-ray, abdominal ultrasound), therapeutic (treatment protocol), and evolutionary (cure, failure and loss of sight) variables were specified. Depending on the context, other assessments (bacteriological samples outside the skin and other radiological examinations) were also performed.
RESULTS
Prevalence and Socio-Demographic Characteristics
During the study period, 26.024 patients were consulted and 10 cases of cTB diagnosed, representing a prevalence of 0.03% and a hospital incidence of 2.93 cases per year. The median age was 24 years, with an interquartile range of 23 years and extremes of 5 to 57 years. The 20–30-year age group accounted for 40% of the patients, while the 5–10-year age group accounted for 30%. Forty percent of our patients had a secondary education; all resided in the city of Abidjan or its suburbs with 30% and 20%, respectively, in the communes of Yopougon and Abobo.
Clinical Features
The duration of the disease before the first consultation varied between five months and ten years, with a median of one year. Eight patients had been vaccinated with BCG and only one had previous contact with tuberculosis.
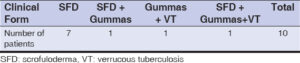
The main dermatological lesions were firm nodules present in 70% of the patients, or fistulized (40%), ulcerations (70%), retractile scars (40%), fluctuating tumors (30%), and verrucous plaques (20%) (Table 1). Ten cases of scrofuloderms or écrouelles were observed (70%), and we noted three cases of the association of several clinical forms. Associated visceral localizations were found in all ten patients: lymph node localization in eight cases and pulmonary in two.
Paraclinical Characteristics
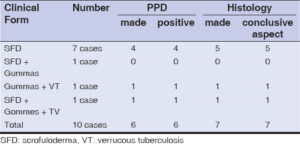
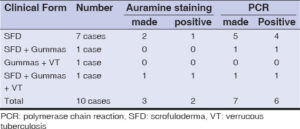
The tuberculin or PPD standard test performed in six patients (Table 2) was positive in all (100%). Histological examination in seven patients (Table 2) showed tuberculoid granuloma with caseous necrosis in all (100%). A search for AFB by auramine staining in three patients was positive in two (66.7%) and the detection of Mycobacterium tuberculosis by gene amplification in purulent secretions was positive in six out of seven cases (85.7%), all of which were sensitive to rifampicin (Table 3). All our patients had negative HIV serology.
Treatment and Progress
The treatment regimen according to the National Tuberculosis Control Programme in Ivory Coast was 2RHZE/4RH in seven patients and 2RHZ/4RH in the three others, depending on their weight. However, in one patient suffering from scrofuloderma, due to the persistence of nodular lesions that remained fistulized despite an improvement in general condition, the protocol was extended to seven months for the maintenance phase to obtain healing.
Healing was achieved in nine of the patients at the cost of numerous retractile scars, and one patient was lost to follow-up.
DISCUSSION
cTB is a rare extrapulmonary localization of BK, even in highly endemic countries such as Ivory Coast [4–9]. In our series, the annual hospital incidence of cTB was 2.93 cases. This was consistent with a series from the Maghreb [10,11], yet it was lower in counterparts in the West African subregion: 3.38 cases/year in Mali [7] and 4.57 cases/year in Senegal [6]. This could be explained by the fact that our study coincided with the onset and peak of the COVID-19 pandemic, which was marked by a decline in hospital attendance. The relatively young age of onset in our study is typical of cTB in sub-Saharan regions [6,7]. We note the ubiquitous nature of the disease marked by a distribution that does not distinguish between the age of the patients, their level of education, or their area of residence.
Clinically, the richness of symptoms observed in our study testifies to the anatomical-clinical polymorphism of TB and constitutes a diagnostic difficulty for practitioners. Only lesions of true cutaneous tuberculosis were collected in our series, as in other studies conducted in West Africa [6–8] with a scrofuloderma and gumma predominance. This predominance was observed in all regions of the world (Europe [12], South America [13], Maghreb [9,11,14], and sub-Saharan Africa [6,7]) with the exception of Asia, where there was a clear predominance of lupus tuberculosis [15,16].
No patient was HIV positive in our series. The same observation was also made in France and Morocco [9,12]. However, Ossalé Abacka et al., in a retrospective study comparing EPT and pulmonary tuberculosis (PT), found an HIV positivity rate of 37.34% for EPT and concluded that the latter was the prerogative of subjects with weak immune defense [17]. However, the latter did not record any cases of cTB. This concrete difference between the cTB and the other EPT on HIV co-infection raises the question of whether HIV, or even immunodepression in general, has a real, direct or indirect link in the development of cutaneous tuberculosis.
The PPD performed on six patients had a 100% positivity rate. These patients all had scrofuloderma and/or gumma, two clinical forms known as multibacillary. Knowing that the pauci/multibacillary classification in cTB is based on the same principle as that of Ridley and Jopling in leprosy, one would expect a negative PPD, which is not the case and once again calls into question the impact of immunodepression in this disease. PCR had a positivity rate of 85.7% with a sensitivity to rifampicin in all cases and the efficacy of the first-line antituberculosis treatment was noted. This efficacy was found in almost all studies, although there were variations in the duration of treatment [6,7,9,10,14].
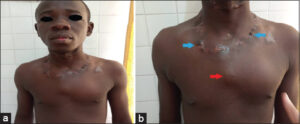
The particularity of our study was that 3 out of our 10 patients had several clinical forms of cTB simultaneously, namely, gummas and verrucous tuberculosis (patient 1, Figs. 1 – 2), scrofuloderma and gummas (patient 2, Figs. 3 – 4), and especially scrofuloderma, gummas and verrucous tuberculosis (patient 3, Figs. 5 – 6). Combinations of two clinical forms have been frequently observed in the last decade [9,11,18,19], yet a combination of three clinical forms remained rare, even exceptional. As with other authors, we were unable to establish a link between all these patients that could explain this phenomenon, and no immunodepression factor was found. However, the frequent coexistence of several clinical forms of cTB in the same patient would indicate a preferential attack of cTB in specific areas that remain to be identified.
CONCLUSION
Our series illustrates the anatomical-clinical polymorphism of cTB marked by the predominance of the so-called multibacillary forms with scrofuloderms and gummies. The first-line anti-tuberculosis treatment remains effective. We did not find any association with immunodepression in general, or HIV in particular, and it would be advisable in our context to look for favoring factors of the occurrence of cTB.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Mjid M, Cherif J, Ben Salah N, Toujani S, Ouahchi Y, Zakhama H, et al. Épidémiologie de la tuberculose. Rev Pneumol Clin. 2015;71:67 72.
2. Organisation mondiale de la Santé. Rapport sur la tuberculose dans le monde 2021. Genève:Organisation mondiale de la Santé;2022. Disponible sur:https://apps.who.int/iris/handle/10665/353790
3. Man-Koumba S, Abdoulaye O, Youssouf T, Boris T-KG, Issifou Y, Daouda S, et al. [Epidemiology of tuberculosis in Côte d’Ivoire:A systematic review]. Rev Int Sci Médicales. 2018;20:140 7.
4. Kivanc-Altunay I, Baysal Z, Ekmekci T, Koslu A. Incidence of cutaneous tuberculosis in patients with organ tuberculosis. Int J Dermatol. 2003;42:197 200.
5. Farina M, Cegundez M, Pique E. Cutaneous tuberculosis:A clinical, histopathologic and bacteriologic study. J Am Acad Dermatol. 1995;33:433 40.
6. Assane K, Cisse M, Diallo M, Dieng Mame T, Ndiaye B, Niang SO, et al. [Cutaneous tuberculosis in Dakar:151 cases report]. Mali Med. 2010;25:14 7.
7. Dicko A, Faye O, Fofana Y, Soumoutera M, BerthéS, TouréS, et al. [Cutaneous tuberculosis in Bamako, Mali]. Pan Afr Med J. 2017;27:102.
8. Andonaba JB, Barro-TraoréF, Yaméogo T, Diallo B, Korsaga-SoméN, TraoréA. [Cutaneous tuberculosis:Observation of six confirmed cases at CHU Souro Sanou (CHUSS) Bobo-Dioulasso (Burkina Faso)]. Pan Afr Med J. 2013;16:50.
9. Gallouj s, Harmoucch T, Karkos F, Baybay H, Meziane M, Sekal M, et al. [Cutaneous tuberculosis:A 36-case series from Morocco]. Med Trop. 2011;71:58 60.
10. Ben Jmaa M, Ben Ayed H, Koubaa M, Ben Hmida M, Trigui M, Hammami F, et al. La tuberculose cutanée entre 1995 et 2016 :particularités épidémio-cliniques et évolutives. Méd Mal Infect. 2020;50:S150.
11. Farah A, Souissi A, Ines Z, Ben Lagha I, Chelly I, Slim H, et al. La tuberculose cutanée :étude anatomoclinique. Rev Méd Interne. 2019;40:A109.
12. Maalouf D, Halabi-Tawil M, Bourrat E, Bouaziz J-D, Bagot M, Flageul B, et al. Facteurs de risque et caractéristiques cliniques et microbiologiques de la tuberculose cutanées :étude rétrospective de 29 cas confirmés en culture. Ann Dermatol Vénéréol. 2015;142:S436.
13. Mann D, Sant’Anna FM, Schmaltz CAS, Rolla V, Freitas DFS, Lyra MR, et al. Cutaneous tuberculosis in Rio de Janeiro, Brazil:Description of a series of 75 cases. Int J Dermatol. 2019;58:1451 9.
14. Sajiai H, Fikal S, Serhane H, Aitbatahar S, Rachid H, Moumen N, et al. Tuberculose cutanée. Rev Mal Respir. 2016;33:A166.
15. Zhang J, Fan Y k., Wang P, Chen Q q., Wang G, Xu A, et al. Cutaneous tuberculosis in China:A multicentre retrospective study of cases diagnosed between 1957 and 2013. J Eur Acad Dermatol Venereol. 2018;32:632 8.
16. Sharma S, Sehgal VN, Bhattacharya SN, Mahajan G, Gupta R. Clinicopathologic spectrum of cutaneous tuberculosis:A retrospective analysis of 165 Indians. Am J Dermatopathol. 2015;37:444 50.
17. OssaléAbacka KB, KonéA, Akoli Ekoya O, Bopaka RG, LankoandéSiri H, Horo K. Tuberculose extra-pulmonaire versus tuberculose pulmonaire :aspects épidémiologiques, diagnostiques et évolutifs. Rev Pneumol Clin. 2018;74:452 7.
18. Elkhachine Y, Sakkah A, Hallab L, Jakar A, Elhaouri M, Elbenaye J. Tuberculose verruqueuse compliquant un scrofuloderme chez un enfant immunocompétent. Ann Dermatol Vénéréologie. 2019;146(12, Supplément):A196.
19. Nguena Feungue U, Abdoul W, Kouotou EA. Disseminated tuberculosis in HIV-negative patient:A special case combining tuberculous gumma, scrofulodermas and pulmonary tuberculosis. Our Dermatol Online. 2021;12(Supp 2):21 5.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0006-5975-0449 http://orcid.org/0009-0006-5975-0449 http://orcid.org/0000-0001-8529-3962 http://orcid.org/0000-0001-8529-3962 http://orcid.org/0000-0003-0630-2678 http://orcid.org/0000-0003-0630-2678 http://orcid.org/0000-0002-1094-6188 http://orcid.org/0000-0002-1094-6188 |










Comments are closed.