Fibrosing frontal alopecia: An original pediatric case
Najoua Ammar , Jihane Belcadi, Sara Oulad Ali, Mariam Meziane, Laila Benzekri, Karima Senouci
, Jihane Belcadi, Sara Oulad Ali, Mariam Meziane, Laila Benzekri, Karima Senouci
Department of Dermatology and Venereology, CHU Ibn Sina, Université Mohammed V Rabat
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Frontal fibrosing alopecia (FFA) is an anatomoclinical form of lichen planus pilaris, which is defined by a recession of the frontotemporal and sometimes even occipital line of implantation of the scalp, realizing a banded or crown-shaped, scarring alopecia. Described for the first time by Kossard in 1994 in six postmenopausal women and, since this first description, several cases have been documented, thus coining the term postmenopausal describing this type of scarring alopecia [1]. Herein, we report an original pediatric case of FFA, confirmed clinically, dermoscopically, and histologically.
A twelve-year-old female with no particular pathological history presented with a progressive and symmetrical receding frontotemporal hairline of the scalp evolving since the age of six years. On clinical examination, there was frontotemporal alopecia in bands with the disappearance of downy hair, follicular hyperkeratosis, and the “solitary hair” sign (Figs. 1a and 1b). The rest of the physical examination was normal. Dermoscopy revealed erythema and perifollicular hyperkeratosis, and the histological examination was in favor of lichen planus pilaris. We, therefore, retained the diagnosis of AFF and the child received oral corticosteroid in mini-pulses of 20 mg/day twice a week.
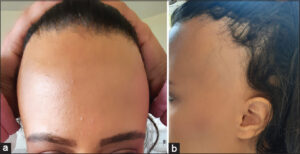 |
Figure 1: (a-b) Symmetrical recession of the frontotemporal implantation line with the disappearance of the downy hair. |
AFF is a rare condition with an increasing incidence. It is characterized by the progressive recession of the fronto-temporo-parietal, sometimes even occipital, line of implantation of the scalp, realizing a scarring alopecia known as the “band” or “crown” [2]. The downy hair disappears completely, giving a particular aspect to the line of implantation. A few isolated terminal hairs often remain in front of the receding area, giving the sign of the solitary hair [3], which is useful for distinguishing AFF clinically from other alopecias that may affect the frontotemporal region, such as traction alopecia, androgenic alopecia, and alopecia pelada. In its typical form, the diagnosis may be exclusively clinical. Dermoscopy facilitates the diagnosis of AFF by showing sensitive and specific signs [4]. In case of doubt, histology is necessary. AFF is not always postmenopausal, nor exclusively female [5]. Some cases have been reported in non-menopausal women, followed by rare pediatric cases. Male cases have also been described, as well as familial cases [6,7]. The etiology of AFF has not been clearly elucidated. Its occurrence after menopause argues for a hormonal factor. The efficacy of anti-androgens, reported by some authors, is also in this direction. However, observations in non-menopausal women, in men, and now in children do not support this hypothesis. A genetic component remains to be confirmed after the recent identification of familial cases. Regarding treatment, there is no consensus on a therapeutic strategy. Intralesional corticosteroid therapy allows to obtain an improvement in almost 60% of cases.
The description of cases of FFA in children intrinsically implies a paradigm shift in the conception of the disease.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Kossard S. Postmenopausal frontal fibrosing alopecia. Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-4.
2. Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia:A multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670-8.
3. Tosti A, Miteva M, Torres F. Lonely hair:A clue to the diagnosis of frontal fibrosing alopecia. Arch Dermatol. 2011;147:1240.
4. Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5:82-8.
5. Jumez N, Bessis D, Guillot B. [Frontal fibrosing alopecia is not always post-menopausal]. Ann Dermatol Venereol. 2005 Mar;132:263.
6. Salido-Vallejo R, Garnacho-Saucedo G, Moreno-Gimenez JC, Camacho-Martinez FM. Beard involvement in a man with frontal fibrosing alopecia. Indian J Dermatol Venereol Leprol. 2014;80:542-4.
7. Chan DV, Kartono F, Ziegler R, Abdulwahab N, DiPaola N, Flynn J, et al. Absence of HLA-DR1 positivity in 2 familial cases of frontal fibrosing alopecia. J Am Acad Dermatol. 2014;71:e208-10.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-6348-4450 http://orcid.org/0000-0001-6348-4450 |




Comments are closed.