Benign vulvar tumors: A series of 60 cases
Noura Kalmi , Hanane Baybay, Choukri Souad, Zakia Douhi, Sara Elloudi, Soughi Meryem, Fatima Zahra Mernissi
, Hanane Baybay, Choukri Souad, Zakia Douhi, Sara Elloudi, Soughi Meryem, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Vulvar dermatology represents a challenge for many providers. Patients with vulvar lesions may present for primary care, gynecology, or dermatology. Although most tumors do not require treatment, it is necessary to consider a differential diagnosis, including pre- and malignant tumors and infectious pathologies. The aim of our study was to report the various benign tumors in a vulvar pathology series. The observational study included 64 cases over five years. Clinical examination was supplemented by dermoscopy, and a biopsy was taken in suspected cases or cases with a doubtful diagnosis. Condyloma acuminatas were excluded from our study.
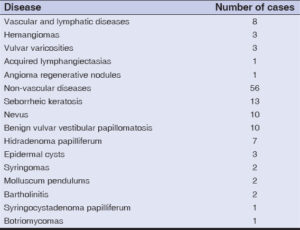
Among 200 patients, 49 had 64 benign tumors, among which only eight were of a vascular or lymphatic nature (Figs. 1a – 1d), while 56 were not (Figs. 2a – 2j). Twenty patients had multiple lesions. Table 1 summarizes the number of cases by type of pathology. Lesions were mainly located on the labia majora (83%), vestibule (15%), and other sites (2%). They were asymptomatic (80%), pruritic (15%), bleeding on contact (6%), painful (4%), and oozing in the patient with acquired lymphangiectasias. Excision confirmed the diagnoses of hidradenoma papilliferum, syringomas, molluscum pendulum, botriomycomas, and syringosystadenomas papilliferum. For seborrheic keratosis, nevus, and epidermoid cysts, excision was performed for patients who requested it. Other treatments were instituted: laser in the patient with acquired lymphangiectasias; antibiotic therapy with drainage in the two cases of bartholinitis; venotonics for varicosities; and propanolol for infantile hemangiomas. Therapeutic abstention was recommended for benign vulvar vestibular papillomatosis.
As a gynecological and dermatological organ, the vulva falls well within the dermatologist’s practice [1,2]. To date, no staging of benign vulvar tumors has been established [1].
Most benign vulvar tumors are diagnosed clinically, sometimes requiring appraisal through the dermoscope, and do not require any treatment; however, surgical excision may be indicated for various reasons, such as aesthetic appearance, friction, recurrent infection, or if malignancy is suspected [3–5]. Some of these tumors have shown an association between their increase in size and hormonal factors (pregnancy, menstruation) as well as endocrinopathies [6]. The dermatologist has a key role to play in recognizing benign lesions of the vulva, diagnosing malignant lesions at an early stage, alleviating patient anxiety, and reducing the need for unnecessary examinations [1].
Our study presents a panorama of benign vulvar tumors, with the presence of fairly rare tumors. Despite the frequency of bartholinitis, its small number in our series may be explained by its easy recognition by general practitioners and its direct referral to gynecology. However, their occurrence in postmenopausal women should exclude any malignancy [7].
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Corrado G, Garganese G. Leading new frontiers in vulva cancer to build personalized therapy. Cancers (Basel). 2022;1424:6027.
2. Puri N, Puri A. A study on non venereal genital dermatoses in north India. Our Dermatol Online. 2013;4:304-7.
3. Mohamed M, Korbi M, Hadhri R, Akkari H, Hajjaji A, Youssef M,et al. A huge fibro epithelial polyp of the vulva with myxoid stroma in Tunisian nulliparous woman. Our Dermatol Online. 2014;5:409-11.
4. El Faqyr I, Dref M, Zahid S, Oualla J, Mansouri N, Rais H, et al. Syringocystadenoma papilliferum presented as an ulcerated nodule of the vulva in a patient with Neurofibromatosis type 1. Our Dermatol Online. 2020;11:174-6.
5. Mansouri S, Mai S, Ismaili N, Benzekri L, Hassam B. Acquired vulvar lymphangioma circumscriptum:A report of 3 cases. Our Dermatol Online. 2019;10:156-8.
6. Mansur AT, Ramadan S. Syringoma, hormone receptors and associated endocrinopathies:Are they clinically relevant?Our Dermatol Online. 2020;11:168-70.
7. Chang Y, Wu W, Chen H. Adenoid cystic carcinoma of the Bartholin’s gland:A case report and literature review. J Int Med Res. 2020;482:300060519↻40.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |






Comments are closed.