Warts as a common occurrence on nevus sebaceous: A case series depicting locus minoris resistentiae
Shuhaab Shah1, Faizan Younus Shah 2, Uzair Khursheed Dar3, Shah Aaqib Aslam3
2, Uzair Khursheed Dar3, Shah Aaqib Aslam3
1Department of Dermatology, Government Medical College, Srinagar, University of Kashmir, Jammu and Kashmir, India, 2Lecturer, Department of Dermatology, SKIMS Medical College, Srinagar, Jammu and Kashmir, India, 3Registrar, Department of Dermatology, SKIMS Medical College, Srinagar, Jammu and Kashmir, India
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Locus minoris resistentiae (LMR) is a special site that offers less resistance to the onset of disease than the rest of the body. Areas of cutaneous mosaicism may act as congenital LMR sites. Viral infections such as verruca are a rare occurrence on these sites. Nevus sebaceous is a benign hamartoma with epidermal, follicular, and apocrine mosaicism in the stem cells that expand in the lines of Blaschko, which may act as a site of LMR. Herein, we present a case series of nevus sebaceous to document the occurrence of verrucae and the possibility of LMR at these sites.
Key words: Wart, Locus minoris resistentiae, Nevus sebaceous
INTRODUCTION
Locus minoris resistentiae (LMR) is a special site that offers less resistance to the onset of disease than the rest of the body. Trauma, irradiation, healed herpes scars, or chronic lymph stasis act as LMR, thus predisposing the site to numerous inflammatory and neoplastic conditions [1]. Areas of cutaneous mosaicism may act as congenital LMR sites. Infectious conditions such as verrucae in such areas are rare [2]. Herein, we report clinico-pathological findings in a series of twelve patients, among whom four cases developed verrucae on nevus sebaceous, pointing toward a possibility of nevus sebaceous as a site of locus minoris resistentiae.
CASE REPORT
Case 1
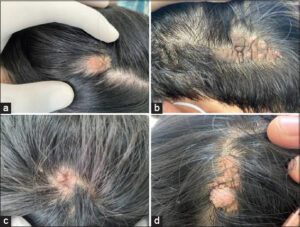
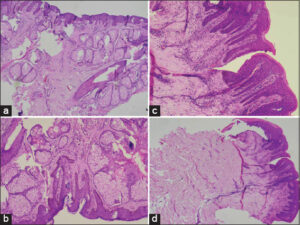
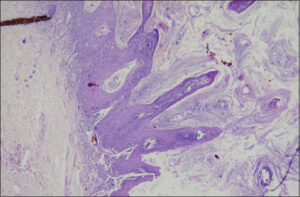
A seventeen-year-old female presented with a solitary asymptomatic orangish-pink raised lesion on the scalp present since birth. She had developed a new lesion with finger-like projections on the old lesion in the previous three months (Fig. 1a). There was no such lesion anywhere else on the body. A biopsy from the orange plaque showed sebaceous gland hypertrophy, abortive hair follicles, acanthosis, and epithelial papillomatosis, suggestive of nevus sebaceous (Fig. 2). A biopsy from the warty lesion revealed hyperkeratosis, parakeratosis, acanthosis, with papillomatosis and koilocytic changes suggestive of warts (Fig. 3). Based on the clinico-histopathological findings, a diagnosis of verruca on nevus sebaceous was established.
Case 2
A ten-year-old male presented with a brownish-yellow lesion on the scalp present since birth. His father noticed a new skin-colored growth near the edge of the previous lesion two months previously. A well-demarcated, hairless, brownish-yellow plaque with filiform growth in the periphery was present on the scalp (Fig. 1b). A clinical diagnosis of nevus sebaceous with filiform wart was confirmed by histopathology.
Case 3
A fifteen-year-old male with an orangish-gray lesion near the vertex present since birth developed a small, rough growth near the edge of the lesion, incidentally noticed by his mother one month previously. A yellowish-brown plaque with irregular edges and an uneven, smooth surface with a filiform growth in the periphery of the lesion was observed on examination (Fig. 1c). The clinico-histopathological findings confirmed the diagnosis of nevus sebaceous with an overlying wart.
Case 4
A twelve-year-old female presented with an orangish-yellow plaque on the scalp apparent since birth and a four-month history of a new large pinkish growth with a rough surface near the anterior aspect of the lesion. A diagnosis of verruca overlying nevus sebaceous was established on clinico-pathological grounds (Fig. 1d). All cases were treated with electrocautery.
The remaining eight cases presented as asymptomatic, yellowish-brown to pinkish plaques of varying sizes and a smooth overlying surface with the absence of hair. The lesions had been present since birth. Based on clinico-pathological grounds, they were diagnosed as cases of nevus sebaceous (Table 1) (Fig. 4). No new growth was noticed at any site.
 |
Figure 4: a-h) Eight cases of nevus sebaceous presenting as solitary, well-defined, hairless, orangish-brown plaques on the scalp. |
Among the twelve cases who presented with nevus sebaceous, four were seen to have secondary growth, which turned out to be verrucae. The prevalence of verruca overlying nevus sebaceous was found to be 33.3%, which was much higher than what was anticipated. This favored the notion of nevus sebaceous as a site of LMR with high chances to develop secondary viral infection, especially due to human papilloma virus.
DISCUSSION
Genetic and acquired factors make some areas of skin more vulnerable to infections than the rest of the body. These areas are known as the immunocompromised district (ICD). Local immune dysregulation makes these sites prone to developing opportunistic infections, tumors, or immune reactions (often of granulomatous nature) confined strictly to the district itself.
Locus minoris resistentiae may be defined as a site that offers lesser resistance to the development of a disorder as compared to rest of the body. LMR may be congenital or acquired. Epidermal nevi, lichen striatus, congenital hemangioma, giant melanocytic nevus, linear porokeratosis, and CHILD syndrome, all being areas of cutaneous mosaicism, act as congenital LMR [2]. The acquired causes of localized immune dysregulation are chronic lymph stasis, herpetic infections, ionizing and UV radiation, burns, trauma (amputation), tattooing, etc. [3,4]. Nevus sebaceous is a benign hamartoma with epidermal, follicular, and apocrine mosaicism in the stem cells that expand in the lines of Blaschko. Various inflammatory dermatoses, adnexal disorders, and neoplasms have been reported to occur on sebaceous nevi [5].
Cribier et al. reported that the most common benign and malignant tumors associated with nevus sebaceous were syringocystadenoma papilliferum and BCC, respectively. They also reported fourteen cases of verrucae on nevus sebaceous [6]. Carlson et al. detected human papilloma virus DNA in 82% of cases of nevus sebaceous, which may be a predisposing factor in the pathogenesis of verrucae on nevus sebaceous [6].
The available literature on such reports from India is sparse. Herein, we have reported this case series in support of the view that nevus sebaceous may act as a site of LMR, and any new growth on nevus sebaceous should be confirmed histopathologically due to the rarity of this association.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent. The patients have given their consent for images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be given to conceal their identity but complete anonymity cannot be guaranteed.
REFERENCES
1. Ruocco V, Ruocco E, Piccolo V, Brunetti G, Guerrera LP, Wolf R. The immunocompromised district in dermatology:A unifying pathogenic view of the regional immune dysregulation. Clin Dermatol. 2014;32:569-76.
2. Al-Rohil RN, Leung D, Carlson JA. Congenital vulnerability of cutaneous segments arising from skin mosaicism:A genetic basis for locus minoris resistentiae. Clin Dermatol. 2014;32:577-91.
3. Ruocco V, Brunetti G, Puca RV, Ruocco E. The immunocompromised district:A unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-73.
4. Baroni A, Piccolo V, Russo T, Ruocco V. Recurrent blistering on fingerprints as a sign of carpal tunnel syndrome:An effect of nerve compression. Arch Dermatol. 2012;148:545-6.
5. Ranugha PS, Betkerur JB, Veeranna S, Basavaraj V. Appearance of verruca over linear verrucous epidermal nevus:An example of locus minoris resistentiae:A report of three cases. Indian Dermatol Online J. 2018;9:334-7.
6. Carlson JA, Cribier B, Nuovo G, Rohwedder A. Epidermodysplasia verruciformis-associated and genital-mucosal high-risk human papillomavirus DNA are prevalent in nevus sebaceous of Jadassohn. J Am Acad Dermatol. 2008;59:279-94.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|





Comments are closed.