Merkel cell carcinoma: A rare sarcoma
Jorge González-Torres 1, Georgína Gutierrez-Rodriguez1, Judith Corona-Herrea1, Linda García-Hidalgo1, Judith Domínguez-Cherit1, Daniel Montante-Montes2, Edgar Salas-Ochoa3
1, Georgína Gutierrez-Rodriguez1, Judith Corona-Herrea1, Linda García-Hidalgo1, Judith Domínguez-Cherit1, Daniel Montante-Montes2, Edgar Salas-Ochoa3
1Dermatology Department, National Institute of Medical Sciences and Nutrition “Salvador Zubirán”, Mexico City, Mexico, 2Pathology Department, National Institute of Medical Sciences and Nutrition “Salvador Zubirán” Mexico City, Mexico, 3Plastic Surgery, Mexican Institute of Social Security, Specialty Hospital “La Raza”. México City, Mexico.
Citation tools:
Copyright information
© Our Dermatology Online 2024. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Merkel cell carcinoma (MCC) is a rare cutaneous neoplasm that accounts for less than 1% of all primary cutaneous neoplasms. The majority of MCC cases (80%) are caused by Merkel cell polyomavirus (MCPyV) clonal integration into the host genome. In the remaining 20% of cases, UV mutations are responsible, and prolonged UV exposure is a factor. Herein, we present two cases of this rare tumor: a 48-year-old female with a diagnosis of hairy cell leukemia and an elderly male previously healthy.
Key words: Merkel cell carcinoma, Cutaneous neoplasm, Hospital dermatology
INTRODUCTION
Merkel cell carcinoma (MCC) is a rare cutaneous neoplasm that accounts for less than 1% of all primary cutaneous neoplasms [1]. A trabecular carcinoma was first described by Toker in 1972. It was named Merkel cell because it expresses Merkel cell markers, which are still being discussed. Regional incidences range from 0.1 to 0.88/100,000 person-years, yet they are higher in countries such as New Zealand and Australia [2]. A majority of MCC cases (80%) are caused by Merkel cell polyomavirus (MCPyV) clonal integration into the host genome. In the remaining 20% of cases, UV mutations are responsible, and prolonged UV exposure is a factor [3,4]. MCPyV early regions contain large and small T antigens, which have been shown to drive tumorigenesis. These proteins may play a role in MCC as well. Cells express a truncated form of LT protein that cannot replicate the virus yet retain the domain that inhibits retinoblastoma (Rb), the tumor suppressor. MCC without MCPyV exhibit cellular genomic mutations in tumor suppressor genes, especially TP53 and RB1. Other tumor suppressors, including NOTCH genes and KMT2D, are inactivated less frequently [5]. Based on a systematic review conducted in Japan, the following clinical characteristics were found: male-to-female ratio of 1:1.6, mean age of 77.5 years; 63.0% of the tumors found in the head and neck, 5.2% in the trunk, 12.6% in the upper limbs, 15.1% in the lower limbs, 3.5% in the buttocks, and 0.6% in the genitals; mean tumor size of 2.79 cm, MCPyV detected in 68.9%, and immunosuppression noted in 6.8%[6]. Herein, we present two cases of this rare tumor that are larger than usually reported in the literature and have rare topography: one was immunosuppressed, and the other was sun-exposed.
CASE REPORTS
Case 1
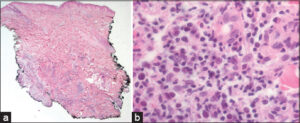
A 48-year-old female and a stay-at-home mom was diagnosed with low-risk hairy cell leukemia in 2019 and was given cladribine to treat it. In 2020, she was seen by the dermatology team and diagnosed with dermatosis with a neoformation. It was in her right gluteus and looked cupuliform with a diameter of 4 cm. The surface was smooth and shiny, with purple coloration, and the edges were regular and smooth, with a solid consistency (Fig. 1a). When it was looked at through a microscope, there were unstructured, white and pink areas (Fig. 1b). She had three months of growth and was growing rapidly, yet she was not feeling well. A spindle biopsy was performed, and the pathology report was invasive MCC with deep dermis invasion (Figs. 2a and 2b). CK-7, CK20 + (Fig. 3a), Chromogranin + (Fig. 3b), Synaptophysin -, Ki67 80%, CD56 +, Pax 5+ (Fig. 3c) CD117 + (Fig. 3d). Subsequently, the oncology service classified the patient as an IV EC patient, and she was subsequently treated with surgery and etoposide and cisplatin chemotherapy.
Case 2
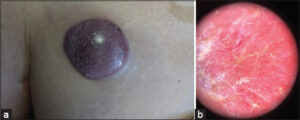
In 2021, an elderly male, a flea market vendor, and a type 2 diabetic, had a dermatosis with exophytic necrolysis, which was located on the right upper limb, affecting the anterior side of the arm, distal third, and elbow. The necrolysis had a diameter of 8 by 12 cm, was multilobulated in appearance, and had a reddish-purple coloration. The surface of the necrolysis was ulcerated and friable, and it was mobile to the touch (Fig. 4a). Dermoscopy revealed an unstructured area of white and pink color (Fig. 4b). The patient had a history of more than one year of painful, intermittent bleeding, limited limb mobility, and continued growth without medical attention. The patient underwent a spindle biopsy, which resulted in a diagnosis of soft tissue carcinoma. The pathology report revealed that the cancer was Merkel cell carcinoma CK20+ with a paranuclear pattern and synaptophysin + and chromogranin +, and it was free of TTF1. Subsequently, the oncology service classified the patient as an IV EC patient, and he was subsequently treated with nivolumab.
DISCUSSION
The clinical presentation of the two cases highlights the wide variation in topographic and morphological presentation, making it a diagnostic challenge, and as with all neoplasms, the diagnosis is histological. They are predominantly located in the head and neck, and were found in the upper extremities and buttocks, the latter being the second most common cases reported in the literature [6,7]. The morphology of the lesion is consistent with that found in other publications. The subcutaneous necro-formations are red to vultureous, well-circled, and may include ulceration and pedunculation. [8,7] The dermoscopic features of the lesion were linear irregular, polymorphous, poorly focused, milky-pink, white, and structureless. Architectural disorder was present, yet pigmented structures were not present in all lesions [7]. In the two cases, the lesion had structureless white or pinkish-red areas. Among the histological differential diagnoses are osteosarcoma, rhabdomyosarcoma, desmoplastic small cell tumor, small cell or amelanotic melanoma, mesenchymal chondrosarcoma, Ewing sarcoma, lymphomas, and neuroblastoma. The metastatic small cell lung cancer is frequently the most challenging distinction [10,11]. A majority of MCC express cytokeratins, CK20 in 95% of cases, neuroendocrine markers (synaptophysin, chromogranin, and CD56), and neurofilament (NF). Thyroid transcription factor-1 (TTF-1) and CDX-2 are negative. CK7 is generally negative, yet occasional reported cases are positive [12]. In the present case, a combination of neural filaments, chronic lymphocytic cells (CK-20), chronic lymphoblastic cells (CK7), and thyroid transcriptase factor-1 (THF-1) stains had a high degree of sensitivity and specificity to differentiate MCC from histopathological mimics [9]. For treatment of localized disease, resection of the tumor with wide margins is recommended, with secondary closure plus radiotherapy. If the lymph nodes are involved, resection plus radiotherapy is recommended. In metastatic disease or recurrence, the treatment of choice includes immunotherapy with anti-PD1 and anti-PDL-1. Avelumab became the first FDA-approved checkpoint inhibitor for MCC, as a first-line treatment, had an ORR of 62.1% in patients with stage IV disease, Nivolumab (anti-PD-1) administered 240 mg every two weeks as a first-line or second-line treatment exhibited tumor regression response in patients with metastatic MCC in phase I/II clinical trial, ORR was 68% with 82% progression-free survival and 92% overall survival at three months. [12,13,14] Only one case was indicated for anti-PD-1 treatment due to the high cost of treatment, making it only available to a limited number of patients. About the forecast MCC primary tumor size cutoff of 2 cm is still considered a significant breakpoint in prognosis [9]. In both cases, the dimensions were larger, which is a negative prognostic factor. The relative 5-year survival in distant cases is 19%. Related factors are nodal involvement, the presence of metastases, and a size greater than 5 cm [15].
CONCLUSION
Clinical diagnosis of Merkel cell carcinoma is a challenging and uncommon neoplasm requiring a high level of suspicion. In this case report, two patients were diagnosed with this neoplasm. These cases illustrated the entire spectrum of the disease. The two neoformations were associated with UV radiation exposure and immunosuppression, respectively. However, the presentation size of these neoformations exceeded the reported literature size, indicating a poor prognosis. This was likely due to the delays in medical care caused by the ongoing COVID-19 pandemic. New treatments are available for the advanced stages of the disease; however, the cost of these treatments makes them out of reach in our country.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Schadendorf D, LebbéC, Zur Hausen A, Avril MF, Hariharan S, Bharmal M, Becker JC. Merkel cell carcinoma:Epidemiology, prognosis, therapy and unmet medical needs. Eur J Cancer. 2017;71:53-69.
2. Amaral T, Leiter U, Garbe C. Merkel cell carcinoma:Epidemiology, pathogenesis, diagnosis and therapy. Rev Endocr Metab Disord. 2017;18:517-32.
3. Tabachnick-Cherny S, Pulliam T, Church C, Koelle DM, Nghiem P. Polyomavirus-driven Merkel cell carcinoma:Prospects for therapeutic vaccine development. Mol Carcinog. 2020;59:807-21.
4. Samimi M, TouzéA. Merkel cell carcinoma:The first human cancer shown to be associated with a polyomavirus. Presse Med. 2014;43:e405-11.
5. Arora R, Choi JE, Harms PW, Chandrani P. Merkel cell polyomavirus in Merkel cell carcinoma:Integration sites and involvement of the KMT2D tumor suppressor gene. Viruses. 2020;12:966.
6. Shinogi T, Nagase K, Inoue T, Sato K, Onita A, Takamori A, Narisawa Y. Merkel cell carcinoma:A systematic review of the demographic and clinical characteristics of 847 cases in Japan. J Dermatol. 2021;48:1027-34.
7. Jalilian C, Chamberlain AJ, Haskett M, Rosendahl C, Goh M, Beck H, et al. Clinical and dermoscopic characteristics of Merkel cell carcinoma. Br J Dermatol. 2013;169:294-7.
8. Ramahi E, Choi J, Fuller CD, Eng TY. Merkel cell carcinoma. Am J Clin Oncol. 2013;36:299-309.
9. Coggshall K, Tello TL, North JP, Yu SS. Merkel cell carcinoma:An update and review:Pathogenesis, diagnosis, and staging. J Am Acad Dermatol. 2018;78:433-42.
10. Merkel cell carcinoma, National Comprehensive Cancer Network, https://www.nccn.org/guidelines/february 2023.
11. Pulitzer M. Merkel Cell Carcinoma. Surg Pathol Clin. 2017;10:399-408.
12. Kok DL, Wang A, Xu W, Chua MST, Guminski A, Veness M, et al. The changing paradigm of managing Merkel cell carcinoma in Australia:An expert commentary. Asia Pac J Clin Oncol. 2020;16:312-9.
13. Babadzhanov M, Doudican N, Wilken R, Stevenson M, Pavlick A, Carucci J. Current concepts and approaches to Merkel cell carcinoma. Arch Dermatol Res. 2021;313:129-38.
14. Wollina U, Koch A, Cardoso JC. Advanced Merkel cell carcinoma:A focus on medical drug therapy. Dermatol Ther. 2020;33:e13675.
15. Survival rates for Merkel Cell Carcinoma https://www.cancer.org/cancer/merkel-cell-skin-cancer/detection-diagnosis-staging/survival-rates.html, ACS.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-1392-1602 http://orcid.org/0000-0003-1392-1602 http://orcid.org/0000-0002-6193-0450 http://orcid.org/0000-0002-6193-0450 http://orcid.org/0000-0002-9151-9726 http://orcid.org/0000-0002-9151-9726 http://orcid.org/0000-0002-0955-4099 http://orcid.org/0000-0002-0955-4099 http://orcid.org/0000-0003-3542-4615 http://orcid.org/0000-0003-3542-4615 http://orcid.org/0000-0002-3654-331X http://orcid.org/0000-0002-3654-331X http://orcid.org/0009-0005-3158-5915 http://orcid.org/0009-0005-3158-5915 |






Comments are closed.