Skin cancers of cephalic extremity epidemiology and their anatomical, clinical, therapeutic, and evolutive aspects: A series of 260 cases
Siham Boularbah , Sara Elloudi, Sabrina Oujdi, Ghita Gmira, Zakia Douhi, Meryem Soughi, Hanane Bay Bay, Fatima Zahra Mernissi
, Sara Elloudi, Sabrina Oujdi, Ghita Gmira, Zakia Douhi, Meryem Soughi, Hanane Bay Bay, Fatima Zahra Mernissi
Department of Dermatology, CHU Hassan II, Fez, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The most malignant skin tumors of the head are dominated by epithelial cancers, particularly basal cell carcinomas, followed by squamous cell carcinomas and melanomas. Herein, we present a case series of malignant skin cancers in the cephalic region. We address their epidemiological, clinical, histological, and therapeutic profiles in our context.
Materials and Methods: This was a prospective study conducted for descriptive purposes on cases of skin cancer, including melanoma, squamous cell carcinoma, and basal cell carcinoma, followed at the dermatology department of CHU Hassan II Fez between June 2017 and December 2021.
Results: We collected a total of 260 patients with different types of skin cancer. 147 cases (57%) were in the cephalic location: 56% presented squamous cell carcinoma, followed by melanoma (22%) and basal cell carcinoma (21%).
Conclusion: The early detection of skin cancer is essential to reduce the functional morbidity and mortality associated with these tumors, especially in these cephalic locations.
Key words: Cutaneous tumors, Cephalic region, Early diagnosis
INTRODUCTION
The head may be affected by all types of skin cancer, the most common being basal cell carcinoma, followed by squamous cell carcinoma and melanoma [1]. Surgery remains the reference treatment yet is still subject to the constraints of mutilation in advanced cases despite the comfort reported by reconstructive surgery. Nevertheless, in the face of clinical scalability, decisions may only be collegial, and respect to the patient and their choices remains essential. The adequate management of these tumors is based on a good knowledge of their epidemiological profiles and diagnostic methods and the different therapeutic methods. Our objective was to determine the epidemiological, anatomical, clinical, therapeutic, and evolutionary profiles of malignant tumors in the cephalic region.
MATERIALS AND METHODS
We conducted a descriptive, retro-prospective study including melanomas, squamous cell carcinomas, and basal cell carcinomas of the cephalic region followed at the dermatology department of CHU Hassan II Fez between June 2017 and December 2021. Epidemiological, clinical, histological, therapeutic, and evolutive data was collected in a pre-established exploitation sheet.
RESULTS
We collected a total of 260 patients with different types of skin cancer (BCC, melanoma, SCC) in different locations (Figs. 1a, 1b, and 2). Among these patients, 147 cases (57%) had a cephalic localization, with an average age of 61.9 years and extremes ranging from twenty years to one hundred years, and a sex ratio of 1.24 (144 males and 116 females). The average diagnosis time, hospitalization waiting time, hospital time were 40.20 and 33 days, respectively.
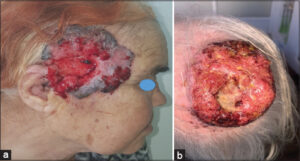 |
Figure 1: (a) Histologically confirmed temporal basal cell carcinoma. (b) Histologically confirmed squamous cell carcinoma of the scalp. |
 |
Figure 2: Histologically confirmed facial melanoma. |
The average time between the symptomatology and initial consultation, the average time of diagnosis in our patients, was 43 months, 40 days. Eighty-seven percent of the patients came from rural areas. Phototypes III and IV were predominant. All patients were exposed to the sun during their childhood and adolescence, without noticeable protection. The patients were mainly farmers, masons, itinerant day laborers, or without professions. Self-medication was noted in 20% of the cases. Sixty percent of the patients consulted with the general practitioner and 20% with the dermatologist, among whom 80% received symptomatic treatment and only 20% had a skin biopsy taken. All patients had benefited from anatomopathological confirmation prior to oncological excision. The diagnostic biopsy revealed 56% squamous cell carcinomas, 22% melanomas, and 21% basal cell carcinomas.
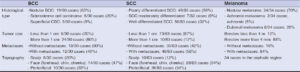
Table 1 shows the distribution of BCC, SCC, and melanoma (Table 1).
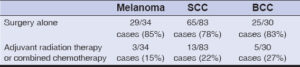
Table 2 shows the received therapeutic management (Table 2).
The cephalic tip may be affected by all types of skin cancers, among which the most common are BCC, followed by SCC and melanoma [1]. In our study, it was noted that SCC was the most frequent followed by melanoma and BCC, which may be explained by the selection of generally aggressive cancers requiring hospitalization at our department. Although the risk of developing carcinoma depends on genetic, phenotypic, and environmental factors, it is well established that UV radiation is the main risk factor for developing skin cancer [2,3]. In our series, most patients were male, of phototypes III and IV, and of rural origin. This may be explained by the fact that males are more exposed to the sun given the nature of their work, and that the majority of them do not use means of protection unlike females. In our series, as in most Maghreb and African publications, the diagnostic time was long [4]. The reasons for late diagnosis were dominated by financial problems and diagnostic errors. The cephalic region may be affected by any type of skin cancer, among which the most common are BCC followed by SCC and melanoma [1]. Basal cell carcinoma is characterized by a local invasive potential, yet it may cause significant tissue destruction to the cephalic region [5,6]. Current guidelines subdivide BCC into low-risk (nodular and superficial) and high-risk (micronodular, infiltrating and morphoeic, squamous differentiation subtypes) [3,4]. Nodular and sclerodermiform BCC is most often located on the head and neck and near the orifices of the face, while the superficial form is mainly located on the trunk and limbs [7]. Our study corroborated the data from the literature in that we observed that the nodular form presented 63% of the cases, followed by sclerodermiform carcinoma (21%). For squamous cell carcinoma, Girish et al. noted that nasal involvement was the most common (25.5%), followed by cheek (16%), periorbital (14%), forehead (7.5%), lip (6%), and chin (2%) involvement [8]. In our work, 54% of SCC were located in the nose, orbit, ear, and mouth, 34% in the cheeks and forehead, and 12% in the scalp. The cervicofacial locations of melanomas accounted for 10% to 30% of cutaneous melanomas. It has been described that the mortality rate is more than two times higher than that of melanomas localized elsewhere [9]. Regarding the risk of invasion, these melanomas are often associated with a high Breslow index and have more high-risk histological features, including neurotropism, lymphovascular invasion, and satellite metastases [9,10]. Our study revealed the predominance of nodular forms (76%), and less common Dubreuil’s melanoma (23%). Almost all of these melanomas were diagnosed late, with a Breslow index greater than 4 mm. This may be explained by the capillary cover [11] in this region and a higher blood and lymphatic flow responsible for a high proportion of rapidly growing, vertically growing melanomas, such as nodular and desmoplastic melanomas [12].
Surgery remains the treatment of choice for skin tumors of the cephalic region. The use of non-surgical treatments that are exclusive or complementary to surgery may be indicated [13]. External beam radiation therapy is most often complementary after surgery for some aggressive tumors [14,15]. In our study, most patients (89%) had received surgical treatment and around 11% had received treatment with either chemotherapy or adjuvant radiotherapy. The evolution was favorable in 66–80% of the patients. However, there was an increase in 14% and death in 6%.
CONCLUSION
Skin cancers of the cephalic region are the most frequent integumentary pathology in the daily practice of the dermatologist and maxilloplastic surgeon in our country. The advanced form of these cancers is a provider of functional morbidity and aesthetic sequelae, and in some situations, is life-threatening, which defines their severity and the difficulties of management both for carcinological excision and reconstruction. The early detection of skin cancer is, therefore, crucial to reduce the functional morbidity and mortality associated with these tumors. As a result, the establishment of continuing medical education programs on the subject as well as the organization of public awareness campaigns are necessary.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
REFERENCES
1. Föhler C, Vogt T, Müller CSL. Malignant head and neck melanoma:Part 1:Diagnosis and histological particularities. HNO. 2015;63:523-34.
2. Michael GB, Corey CM. Nonmelanoma skin cancer. Facial Plast Surg Clin North Am. 2019;27:1-13.
3. Gupta M. Assessment of knowledge, attitudes and practices about sun exposure and sunscreen usage in outpatients attending a Dermatology Clinic in North India. Our Dermatol Online. 2018;10:34-7.
4. DiabatéA, Kourouma HS, Vagamon B, GuéI, Kaloga M, Aka BR. Skin pathology of the elderly patients:Case of black African. Our Dermatol Online. 2018;9:19-21.
5. Daisley Jr H, Rampersad A, Acco O, Ramirez E, Sirjuesingh D. Squamous cell carcinoma developing in an epidermal inclusion cyst. Our Dermatol Online. 2019;10:166-9.
6. Nicoletta B, Nevena S, Sara Z, Ersilia T, Veronica Ba, Alessandra M, et al. Face and scalp basal cell carcinoma treatment:A review of the literature. Acta Dermatovenerol Croat. 2019;27:22-7.
7. Jonathon MF. Basal cell and cutaneous squamous cell carcinomas:Diagnosis and treatment. Am Fam Physician.2020;102:339-46.
8. Girish BK, Boyd V, Hollier L. Basal cell and squamous cell carcinoma. Integument. 2000.
9. Ana CP, Tatiana PB, Ivan SF, Vinícius FC, João PDN, Juliana CTB. Primary cutaneous melanoma of the scalp:Patterns of clinical, histological and epidemiological characteristics in Brazil. PLoS One. 2020;15:e0240864.
10. C Pföhler 1, T Vogt, C S L Müller. Malignant head and neck melanoma:Part 1:Diagnosis and histological particularities. HNO. 2015;63:523-34.
11. Pasquali S, Montesco MC, Ginanneschi C, Baroni G, Miracco C, Urso C, et al. Lymphatic and blood vasculature in primary cutaneous melanomas of the scalp and neck. Head Neck. 2015;37:1596–602.
12. Xie C, Pan Y, McLean C, Mar V, Wolfe R, Kelly JW. Scalp melanoma:Distinctive high risk clinical and histological features. Australas J Dermatol. 2017;58:181-8.
13. Pföhler C, Vogt T, Müller C S L. Malignant head and neck melanoma:Part 2:Therapy. HNO. 2015;63:593-602.
14. Andrew MF,Shayan MS, Pierce C H, Caitlin FG, James FT. Treatment of non-melanoma skin cancers in the absence of Mohs micrographic surgery. Plast Reconstr Surg Glob Open. 2020,8:e3300.
15. Henning A. Skin cancer and “Dr. YouTube”:Using PEMAT scoring to determine understandability and actionability of audiovisual patient education material. Our Dermatol Online. 2020;11:309-11.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3975-8316 http://orcid.org/0000-0002-3975-8316 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X http://orcid.org/0009-0002-5084-9152 http://orcid.org/0009-0002-5084-9152 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 |




Comments are closed.