Evaluation of the therapeutic efficacy of topical 50% hydrogen peroxide vs. 100% trichloroacetic acid vs. 5% 5-fluorouracil in the treatment of warts
Akshay Jain Salecha, Leepika Annamreddy , Kode Sridevi, Damaraju Venkata Satya Bhaskara Ramamurthy, Naga Padma Lakamsani, Teneti Moneka Sai
, Kode Sridevi, Damaraju Venkata Satya Bhaskara Ramamurthy, Naga Padma Lakamsani, Teneti Moneka Sai
Department of Dermatology, Venereology and Leprosy, Katuri Medical College and Hospital, Guntur, India
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Warts (verruca) are caused by human papilloma virus (HPV), which is known to affect the skin and mucosae. Over two hundred strains of HPV have been identified to date, among which few strains cause cutaneous lesions. Various treatment modalities have been elucidated in treating verruca lesions, yet the best therapeutic option is yet to be determined.
Objectives: To evaluate the efficacy and safety of topical 50% hydrogen peroxide (H2O2), 100% trichloroacetic acid (TCA), and 5% 5-fluorouracil (5-FU) as a topical application in the treatment of warts.
Methods: This was a prospective, interventional, clinical trial that included sixty patients with warts randomly allotted into three groups. Group A and group B were treated every week with topical 50% H2O2 and 100% TCA, respectively, and group C with 5% 5-FU under tape occlusion twice a day. The treatment was executed for a maximum period of eight weeks. The patients were evaluated with the Physician Wart Assessment (PWA) every two weeks of treatment and at three months after treatment completion.
Results: At the end of the eight weeks of treatment, 13 patients (65%) in the H2O2 group, 11 patients (55%) in the TCA group, and 8 patients (40%) in the 5% 5-FU group displayed complete clearance of warts (PWA grade 0). In our study, side effects were significantly higher in the TCA group (70%) and in the 5% 5-FU group (60%), notably lower in the H2O2 group (30%) (p = 0.011). The most frequent side effect was irritation (25%), which was reported in all groups. No relapse was encountered at three months of treatment completion.
Conclusion: According to our study, H2O2 and TCA have the advantage of earlier action over 5% 5-FU. However, H2O2 remarkably stands as a safer therapeutic option concerning the clearance of lesions, patient tolerability, and side effects.
Key words: Warts, H2O2, TCA, 5%, 5-FU
INTRODUCTION
Warts (verruca) are caused by human papilloma virus (HPV) [1], which is ubiquitous in nature and is known to affect the skin and mucosae. Over two hundred strains of HPV have been characterized to date [2]. They manifest in the form of common warts, mucosal warts, palmoplantar warts, epidermodysplasia verruciformis, and focal epithelial hyperplasia [3].
Although resistant, verruca has been dealt with a plethora of conventional treatment modalities, such as occlusion, cautery, curettage, cryotherapy, radiofrequency ablation, laser ablation, podophyllin, keratolytics, antiproliferative agents, immunotherapy, and photodynamic therapy [4].
Hydrogen peroxide (H2O2) is a weakly acidic and strong oxidizing agent. It exerts its antiviral effect releasing reactive oxygen species and membrane lipid peroxidation causing apoptosis. It has been used as a peeling agent and as a chemical cautery agent [5]. Trichloroacetic acid (TCA) causes cellular protein hydrolysis causing tissue damage owing to its caustic property [6]. Being an antimetabolite, 5fluorouracil (5-FU) inhibits nucleic acid synthesis, thereby arresting cell proliferation [6]. This mechanism enhances the killing of human papilloma virus (HPV).
Despite the availability of various treatments to deal with warts, the amenable therapeutic option is yet to be determined. This study was undertaken to determine the efficacy of different topical agents in the clearance of warts.
Objectives
The objective was to evaluate the efficacy and safety of topical 50% hydrogen peroxide (H2O2), 100% trichloroacetic acid (TCA), and 5% 5-fluorouracil as a topical application in the treatment of warts.
MATERIALS AND METHODS
This was a prospective, interventional, clinical trial conducted at a tertiary-care hospital for a period of six months after obtaining informed consent from patients and institutional ethical clearance.
All naive patients with warts aged above twelve years and willing to comply with the protocol were included in the study. The exclusion criteria were pregnancy and lactation, immunosuppression, patients with a treatment history of warts prior to enrollment in the study, and patients with unrealistic expectations. On detailed history taking and clinical examination, a total of sixty patients with a clinical diagnosis of warts, randomly divided into three groups, twenty patients in each, were allotted to the study.
At the baseline visit, the lesions were evaluated for type, site, number, and size of warts and photographed in each patient. Group A was treated with topical 50% H2O2 solution, group B with topical 100% TCA, and group C with topical 5% 5-FU. TCA and H2O2 solutions were applied to warts in weekly intervals. The solutions were applied with a wooden toothpick after protecting the surrounding tissue by applying petroleum jelly. The solution was applied, and the formation of white frost was noted on the lesions. Group C patients were advised to apply 5% 5-FU on the lesions with a cotton tip applicator, followed by two-hour occlusion with duct tape twice a day.
The treatment lasted until the total clearance of lesions or a maximum period of eight weeks. Clinical assessments were done at baseline, every two weeks of treatment and after the completion of treatment. Side effects were noted. The patients were also enquired about systemic complaints at each visit. After treatment, follow-up was done three months after treatment completion to check for recurrence.
The following Physician Wart Assessment (PWA) scores were used to assess treatment response:
-
Grade 0: clear.
-
Grade 1: < 3mm (near clear).
-
Grade 2: 3–6 mm.
-
Grade 3: > 6 mm.
Treatment response was noted at each visit and analyzed by a statistician. Data was expressed as mean ± SD quantitative variables and as numbers and percentages as applicable. Chi-squared test and Fisher’s exact tests were used to compare categorical data. An independent sample t-test was used for comparing quantitative data. A p value below 0.05 was considered statistically significant.
RESULTS
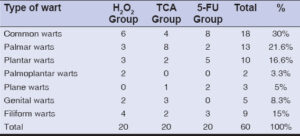
There were 32 (53.3%) males and 28 (46.6%) females out of the total of sixty patients. Age distribution was between 20 and 40 years, with a mean of 31.36 ± 10.28 years. Regarding clinical types, 18 patients had common warts distributed on the trunk and extremities, 13 had palmar warts, 10 had plantar warts, 2 had both palmoplantar warts, 9 had filiform warts distributed on the face and neck, 5 had genital warts, and 3 had plane warts distributed on the face (Table 1). All three groups had comparable demographic data with no significant p value.
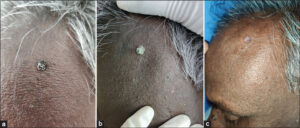
Evaluation was conducted every two weeks (Table 2). By the end of eight weeks, i.e., the completion of all sessions, 13 patients (65%) in the H2O2 group (Figs. 1a and 1b), 11 patients (55%) in the TCA group (Figs. 2a – 2c), and 8 patients (40%) in the 5-FU group (Figs. 3a and 3b) displayed complete clearance of the lesions (PWA grade 0) (Table 3). Treatment responses were compared among the three groups, and no statistically significant difference was noted between the groups.
| Table 2: PWA score at 2, 4, and 6 weeks of treatment. | |
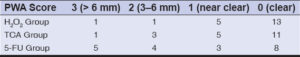 |
Table 3: PWA score at the end of eight weeks of treatment. |
A near-clear response (PWA grade 1) was seen in 5 patients (25%) in the H2O2 group, 5 patients (25%) in the TCA group, and 3 patients (15%) in the 5-FU group. In addition, no response was noted in 3 patients (15%) in the 5-FU group and 1 patient each in the H2O2 and TCA groups.
All three groups exhibited good improvement in terms of reduction in size and number compared to the baseline (Table 4). The H2O2 group had a better reduction with a significant p value of 0.0001, followed by the TCA group with a significant p value of 0.0002 and the 5-FU group with a p value of 0.018.
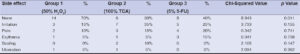
Burning and irritation were the most reported side effects in the H2O2 group and TCA group. Erythema was most reported in the 5-FU group, followed by pain and scaling. Ulceration was noted in one patient in the TCA Group. Overall, side effects were less often reported in the H2O2 group (Table 5). Although irritation and pain were reported more often in groups H2O2 and TCA, symptoms tended to subside post-procedure in the H2O2 group yet lasted longer in the TCA group.
DISCUSSION
Warts are known to be notorious for their unpredictable treatment responses. They occur worldwide and are estimated to involve 30% of children and young adults and 3–5% of adults [7]. They have always been a puzzling entity for clinicians to choose a prudent therapeutic option. The incubation period varies from several weeks to around a year and the number of lesions varies from individual to individual and in the same individual from site to site. Lesions may recur even after obtaining clinical resolution or may regress on their own to recur later. The infection of the host is acquired through direct contact with viral particles or indirect contact via fomites, such as flooring, shoes, clothes, and other equipment [8]. Although not an alarming disease, warts are responsible for psychosocial discomfort [9].
It remains a pressing concern to pick up an efficacious and safe modality of treatment that will cause no recurrences and side effects among currently available treatment options. Sixty patients completed our study, among which 32 (53.3%) were males and 28 (46.6%) were females. Most were in age group 20–40 years. In 2018, Khopkar et al. reported a higher prevalence among males than females, with the highest prevalence in age group 25–29 years [10].
Hydrogen peroxide causes protein denaturation and cell death, which ensures the killing of HPV virus. In our study, after eight weeks of treatment with 50% H2O2, complete wart clearance (PWA grade 0) was noted in 65% of the patients. Similarly, in a trial conducted by Smith et al., patients had a twice-weekly application of 45% H2O2, and statistically significant target wart clearance was achieved in 37.3% out of 76 patients in eight weeks [11]. A study by Kaur et al., in which 40% H2O2 was applied in three sessions at two weeks intervals, revealed a more than 75% reduction in wart size in 30% of twenty patients with genital warts, similarly to our study [5].
TCA has been a time-tested modality for the treatment of warts. In our study, after eight weeks of treatment with 100% TCA, complete wart clearance (PWA grade 0) was noted in 55% of the patients. Similarly, a study by Qayum et al. objectified the efficacy of 100% TCA in anogenital warts. Six sessions of treatment gave an 82% clearance rate in ninety patients [12]. Pouran et al. reported 80% TCA solution being more efficacious than 35% TCA (weekly application in six sessions) yet advised the clinician to be careful in its application [13]. A study conducted by Taner et al. reported the successful treatment of genital warts with 85% TCA (2–4 sittings) in fifty-one female patients, which was in accordance with our study [14].
5-FU blocks DNA synthesis and damages basal layer cells of the epidermis, hindering the proliferation of viral warts. In our study, after eight weeks of treatment with 5% 5-FU, complete wart clearance (PWA grade 0) was obtained in 40% of the patients. Salk et al. studied the efficacy of topical 5% 5-FU in plantar warts under occlusion and observed that 19 out of 20 patients (95%) had complete eradication of all plantar warts within twelve weeks of treatment [15], which would necessitate a longer duration of treatment with 5-FU for better results.
In our study, all three modalities had significant improvement in warts. 50% H2O2 stands ahead of 100% TCA and 5-FU, with a 65% significant improvement vs. 55% (100% TCA) and 40% (5-FU). Meanwhile, the 80% TCA group had a 70% improvement when compared to 40% H2O2 (63% improvement) according to Kaur et al. [5].
50% H2O2 treated patients (group A) had less discomfort and minimal side effects. Few reported irritation and pain, which subsided post-application. 100% of the TCA (group B) patients had more irritation and pain, which lasted longer. Hypopigmentation was noted in two patients (10%). Ulceration was noted in one (5%) patient, also reported in a study by Pouran et al. [13] 5% 5-fluorouracil treated patients (group C) reported irritation, pain, and erythema. Owing to the safety profile, the H2O2 group had minimal side effects and subsided in a short span of time, which was in accordance with a report by Kaur et al. [5].
5-FU treated patients had low response rates in the initial weeks yet had a good response at the end of the eight weeks. At the end of three months of post-treatment follow-up, all three groups had similar results, and no recurrence was encountered.
CONCLUSION
According to our study, H2O2 and TCA have the advantage of earlier action over 5% 5-FU. However, H2O2 stands remarkably as a safer therapeutic option with respect to the clearance of lesions, patient tolerability, and side effects.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Drake LA, Ceilley RI, Cornelison RL, Dobes WL, Dorner W, Goltz RW, et al. Guidelines of care for warts:Human papilloma viruses. J Am Acad Dermatol 1995;32:98-103.
2. Kocjan, BJ, Bzhalava, D, Forslund, O, Dillner, J, Poljak M. Molecular methods for identification and characterization of novel papillomaviruses. Clin Microbiol Infect. 2015:21:808-16.
3. AI Aboud AM, Nigam PK, Wart, SP [internet], Treasure Island (FL):StatPearls publishing;2023 Jan.
4. Scheinfeld N, Lehman DS. An evidence-based review of medical and surgical treatments of genital warts. Dermatol Online J. 200630;12:5.
5. Kaur N, Boparai AS, Kumar S, Brar BK, Bano R, Singh O. Comparative evaluation of therapeutic efficacy and safety of 40% hydrogen peroxide versus 80% of trichloroacetic acid in genital warts. Natl J Physiol Pharm Pharmacol. 2022;12:2081-5.
6. Basavarajappa SJ, Subramaniyan R, Dabas R, Lal SV, Janney MS. A comparative study of topical 5% 5-fluorouracil with needling versus 30% trichloroacetic acid with needling in the treatment of plantar warts. Indian Dermatol Online J. 2021;12:412-6.
7. InformedHealth.org [Internet]. Cologne, Germany:Institute for Quality and Efficiency in Health Care (IQWiG);2006-. Warts:Overview. [Updated 2019 Nov 7].
8. Bruggink SC, Eekhof JA, Egberts PF, van Blijswijk SC, Assendelft WJ, Gussekloo J. Warts transmitted in families and schools:A prospective cohort. Pediatrics. 2013;131:928-34.
9. Bellew SG, Quartarolo N, Janniger CK. Childhood warts:An update. Cutis. 2004;73:379-84.
10. Khopkar US, Rajagopalan M, Chauhan AR, Talwar SK, Singhal PK, Yee K, et al. Prevalence and burden related to genital warts in India. Viral Immunol 2018;31:346-51.
11. Smith SR, Tyring SK, Grande KK, Schlessinger J, Gold MH, Shanier SD. Hydrogen peroxide topical solution, 45% for common warts:Phase 2 efficacy and safety trial results. J Drugs Dermatol. 2020;19:969-76.
12. Qayum A, Majid Paracha M, Sagheer F. Effectiveness of topical 100% trichloroacetic acid in treatment of anogenital warts in male patients. Fortune J Health Sci. 2022;5:37-42.
13. Pouran L, Fakhr-o-Zaman P, Mohammad Taghi, Sareh M. Comparison of the efficacy of 80% trichloroacetic acid with cryotherapy using liquid nitrogen in the treatment of anogenital warts. Iran J Dermatol. 2007;10:174-80.
14. Taner ZM, Taskiran C, Onan AM, Gursoy R, Himmetoglu O. Therapeutic value of trichloroacetic acid in the treatment of isolated genital warts on the external female genitalia. J Reprod Med. 2007;52:521-5.
15. Salk RS, Grogan KA, Chang TJ. Topical 5% 5-fluorouracil cream in the treatment of plantar warts:A prospective, randomized, and controlled clinical study. J Drugs Dermatol. 2006;5:418-24.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0009-8286-5000 http://orcid.org/0009-0009-8286-5000 http://orcid.org/0009-0004-8725-9062 http://orcid.org/0009-0004-8725-9062 http://orcid.org/0009-0001-0491-7284 http://orcid.org/0009-0001-0491-7284 http://orcid.org/0009-0003-6475-5031 http://orcid.org/0009-0003-6475-5031 http://orcid.org/0009-0009-5757-2468 http://orcid.org/0009-0009-5757-2468 http://orcid.org/0000-0002-0460-8465 http://orcid.org/0000-0002-0460-8465 |







Comments are closed.