Syringocystadenoma papilliferum associated with apocrine gland hyperplasia arising from nevus sebaceous
Eleni Klimi 1, Katerina Kourantzi2, Panagiotis Mpethanis2, Dimitrios Panourgias2
1, Katerina Kourantzi2, Panagiotis Mpethanis2, Dimitrios Panourgias2
1Department of Dermatology, Thriassio General Hospital Magula Athens, Greece, 2Department of Pastic Surgery, Thriassio General Hospital Magula Athens, Greece
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
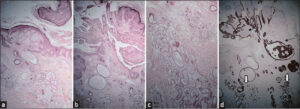
A 22-year-old male with essential endocranial hypertension and hyperaldosteronism consulted for a lesion on the scalp that appeared four years prior to consultation. The patient reported a hairless, yellowish plaque present since childhood at the place of the actual lesion. A clinical examination revealed a soft, erythematous mass, 4 x 4 cm in size, with hyperkeratotic, exophytic horns (Fig. 1). From the medical history, suspicion of a tumor that developed from nevus sebaceous was raised. The patient was referred to the Plastic Surgery Department where the lesion was excised. A histological examination confirmed the clinical suspicion of nevus sebaceous (Fig. 2a). In addition, under areas of epidermal papillomatosis, cystic invaginations were found extending down the dermis. In the lower portion of the cystic invaginations, numerous papillary projections extended into the lumina of the invaginations. The inner row of the papillary projections consisted of columnar cells, while the outer row consisted of small cuboidal cells. This was compatible with the diagnosis of syringocystadenoma papilliferum (Fig. 2b). Another interesting histological finding was apocrine gland hyperplasia (Fig. 2c). Syringocystadenoma papilliferum, likewise apocrine gland hyperplasia, stains positive for cytokeratin CK7, an immunomarker for epithelial cells (Fig. 2d). Nevus sebaceous of Jadassohn manifests in childhood as a hairless, yellowish plaque usually solitary, yet its linear variety may be a component of Schimmelpenning–Feuerstein–Mims syndrome associated with multisystemic complications. Histologically, no or little hair is associated with sebaceous glands that mature with age. Nevus sebaceous is derived from primary epithelial germ cells, which under the influence of external factors, leading to the mutation of different genes (HRAS, KRAS, etc.), may give rise to a variety of neoplasms, both benign and malignant [1]. Syringocystadenoma papilliferum, sebaceoma, trichoblastoma, and trichilemmoma may develop from nevus sebaceous [2]. Basal cell carcinomas, squamous cell carcinomas, and microcystic adnexal carcinomas have also been reported. Rarely, multiple tumors may develop from a single lesion [3]. Ectopic apocrine glands, which are abundant at the breasts, anogenital area, and axilla, may be found in nevus sebaceous, yet the presence of apocrine gland hyperplasia has been considered as a precursor of cancer by some authors [4]. This case is being reported because it is the first case associating syringocystadenoma papilliferum with apocrine gland hyperplasia originating in nevus sebaceous.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Neto MPDS, Assis BR, Andrade GR. Sebaceous nevus of Jadassohn:Review and clinical-surgical approach. An Bras Dermatol. 2022;97:628-36.
2. Wang F, Wu Y, Zheng Z, Bai Y. Syringocystadenoma papilliferum and trichoblastoma arising in the nevus sebaceous. Indian J Pathol Microbiol. 2018;61:106-8.
3. Kuo YW, Lin JC, Tsai WH. Development of seven secondary neoplasms in a nevus sebaceous:A case report and literature review. Arch Craniofac Surg. 2022;23:83-8.
4. Sciarra A, Lopez G, Corti C, Runza L, Ercoli G, Bonometti A, et al. Columnar cell lesion and apocrine hyperplasia of the breast:Is there a common origin?The role of prolactin-induced protein. Appl Immunohistochem Mol Morphol. 2019;27:508-14.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-5113-5640 http://orcid.org/0000-0001-5113-5640 |





Comments are closed.