Cutaneous localization of Waldenström’s macroglobulinemia
Jihad Kassel , Hanane Baybay, Chaymae Jroundi, Sara Elloudi, Zakia Douhi, Fatima-Zahra Mernissi
, Hanane Baybay, Chaymae Jroundi, Sara Elloudi, Zakia Douhi, Fatima-Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Waldenström’s macroglobulinemia (WM) is a rare B-type lymphoproliferative disease of unknown etiology characterized by lymphoplasmacytic proliferation in the bone marrow and a peak of monoclonal IgM in peripheral blood [1]. Cutaneous manifestations remain rare, being manifested in only 5% of the patients. It is divided into two subtypes: neoplastic and non-neoplastic. Non-neoplastic lesions or secondary to paraproteinemia are more frequently non-specific, such as purpura, ulcers, and urticarial lesions. These lesions are caused by hyperviscosity of the blood, immune complex-mediated vascular damage, paraprotein deposition, and amyloid deposition. A cutaneous neoplastic attack or a result of direct cutaneous infiltration of lymphoplasmacytic cells are rarer [2]. Clinically, the cutaneous localization of WM of the neoplastic type presents as firm, erythematopurple papulo-nodules embedded in the dermis and hypodermis, rarely ulcerated, or as a cutaneous infiltration in reddish-brown plaques. More rarely, they are non-infiltrated lesions, such as brownish macules, rounded or oval, and of variable size [2]. Its lesions are located more frequently on the face and ears in a symmetrical manner. Localizations at the level of the thorax, the flanks, and the back are also described [3]. Skin biopsies show a normal epidermis, a dermal infiltrate composed of small lymphocytes and plasma cells or lymphoplasmo-cytoid cells with a nodular, diffuse, or interstitial pattern, sometimes perivascular or periadnexal; the cutaneous lymphoplasmacytic infiltrate is positive for CD19, CD20, and CD22 and negative for CD38 and CD138 (plasma cell markers)s [2]. The treatment of cutaneous localizations of WM is, therefore, justified in the absence of a general indication only in the cases of aesthetic or functional damage, especially since these cutaneous localizations have no prognostic value and do not change the course of the disease [1]. Herein, we report the case of a patient followed for WM with a cutaneous localization presented afterward.
A 75-year-old patient without a pathological history followed for WM for three years consulted for asymptomatic, cutaneous nodules, which appeared two months earlier. On examination, we found cutaneous and subcutaneous nodules at the level of the trunk with an erythematous plate in regards to the sternum (Figs. 1a and 1b). In this context, we suggested a cutaneous localization of WM, cutaneous metastases of solid tumors, and amyloidosis. A skin biopsy was performed revealing a dermal and hypodermic infiltrate consisting of plasma cells and lymphocytes. Immunohistochemistry revealed CD20 to be intensely positive, in favor of a subcutaneous localization of lymphocytic lymphoma. We did not indicate a specific treatment for the cutaneous involvement.
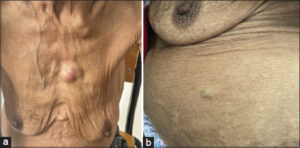 |
Figure 1: (a) An erythematous plate in regards to the sternum. (b) Cutaneous and subcutaneous nodules at the level of the trunk. |
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Stien S, Durot E, Durlach A, Beylot-Barry M, Adamski H, Beltraminelli H, et al. Cutaneous involvement in Waldenström’s macroglobulinaemia. Acta Derm Venereol. 2020;100:adv00225.
2. D’Acunto C, Purpura V, Scarpellini F, Liardo EV, Melandri D. Painful, plantar nodules in cutaneous macroglobulinosis:Successful treatment with rituximab and bendamustine. JAAD Case Rep. 2020;6:981-3.
3. Oscoz-Jaime S, Agulló-Pérez AD, Llanos-Chavarri C, Yanguas-Bayona JI. Cutaneous infiltration due to Waldenström macroglobulinemia. Actas Dermosifiliogr (Engl Ed). 2018;109:75-8.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |




Comments are closed.