Transformed mycosis fungoides in an atypical location
Zineb Zeggwagh ¹, Kaoutar Znati², Nadia Ismaili¹, Mariame Meziane¹, Laila Benzekri¹, Karima Senouci¹
¹, Kaoutar Znati², Nadia Ismaili¹, Mariame Meziane¹, Laila Benzekri¹, Karima Senouci¹
¹Department of Dermatology and venerology, University Hospital Center Ibn Sina, University Mohamed V, Rabat, Morocco, ²Department of Anatomopathology, University Hospital Center Ibn Sina, University Mohamed V, Rabat, Morocco.
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Mycosis fungoides is the most common variant of primary cutaneous T-cell lymphoma. Large cell transformation in mycosis fungoides is the histopathological transformation of neoplastic small lymphocytes to a clonally identical large cell phenotype. It is associated with a poor prognosis, although some patients have indolent disease. Clinically, it is manifested by ulcerated, tumoral lesions that may affect the entire body. The location in the external auditory canal has never been described before. Herein, we report the first case of transformed mycosis fungoides located in the external auditory canal.
Key words: External auditory canal; Large cell transformation; Mycosis fungoides
INTRODUCTION
Mycosis fungoides (MF), the most common form of cutaneous T-cell lymphoma, is mainly seen in older patients [1]. It generally follows an indolent course. However, a transformation of MF into large cell lymphoma occurs in 10% of cases in adults and is associated with an aggressive course and shortened overall survival. Herein, we report an original case of transformed MF located in the external auditory canal (EAC) never described before.
CASE REPORT
A 52-year-old Moroccan patient, with no pathological history, presented to the dermatology department for the appearance of multiple, ulcerative tumors as well as a papulous nodule on the trunk, back, all four limbs, and face with the involvement of the genitals mucosa. All had been evolving for one year. He also reported purulent otorrhea and hypoacusis of the left ear present for one month.
A clinical examination revealed three ulcerative tumors, one next to the right nipple, and the other two on the hypogastrium. He also presented multiple, erythematous papules and nodules on the face, trunk, back, and all four limbs and a multiple, ulcerative lesion on the scrotum (Figs. 1a – 1c). An auricular examination revealed an ulcerative tumor on the posterior wall of the EAC and erythematous papules on the helix (Fig. 1d).
An examination of the lymph node areas found mobile, painless inguinal adenopathy, firm on palpation. The rest of the clinical examination was normal. A skin biopsy and a biopsy of the auricular process with an immunohistochemistry study were in favor of transformed MF (Fig. 2a).
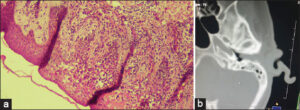 |
Figure 2: (a) Histology with epidermotropism and atypical lymphocyte.(b) CT of the petrous bone revealing a heterogeneous filling of the EAC and the left eardrum. |
CT of the petrous bone revealed a heterogeneous filling of the EAC and the left eardrum, which was in favor of a tumoral process (Fig. 2b). An extended examination through imaging and a biological test was normal and showed no metastasis.
A diagnosis of MF with large cell transformation located in the EAC was established. It was classified as T3N1M0B0 IIB. He was transferred to the hematology department to receive polychemotherapy and, then, he was lost to sight.
DISCUSSION
The incidence of malignant EAC tumors is low. The most common tumors are adenocarcinoma and squamous cell carcinoma. Seventeen cases of MF involving the external ear and EAC have been described so far [2]. Ours was the first case of MF with large cell transformation located in the external auditory canal.
The clinical presentation of MF at the CAE level is not specific. It may be manifested by otalgia, hypoacusis, or otorrhea [3]. The involvement of the EAC by MF portends a poor prognosis [2].
The main complications are essentially infection (otitis) and perforation of the eardrum [4].
Diagnosis is based on histology with an immunohistochemistry study. The biopsy should be deep, or even a complete excision of the process should be performed so as not to miss the diagnosis.
The diagnosis is histological and finds discreet epidermotropism, an atypical lymphocyte population (at least 25%), and significant mitotic activity. The phenotype of these cells may be CD30+ or CD30-.
Diffusion of the lesions to cutaneous, ganglionic, then all organs (spleen, liver, kidneys, lung, GI tract, oropharynx, MO, CNS, etc.) may occur.
The evolution is quick toward the aggressive form and the prognosis is poor. The MF is a great imitator of psoriasis, tinea, and syphilis especially if the lesions are annular [5]. This is why it is always necessary to consider the diagnosis of MF in front of any chronic dermatosis and not to hesitate to multiply the biopsies [6].
Dermoscopy may sometimes help to guide the diagnosis of MF if there is a lesion on the body. The main finding is short linear vessels, dotted vessels, and orangish-yellow, patchy areas [7].
The treatment is poorly codified and depends on the extent of the lesions: localized radiotherapy, monochemotherapy, or polychemotherapy.
In our patient, polychemotherapy treatment with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) was prescribed.
CONCLUSION
The auricular location of the MF is exceptional. It will be necessary to perform a systematic ENT examination in front of any MF even if the clinical manifestations are not specific.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Borowska K, Wasyłyszyn T. Mycosis fungoides as casus pro diagnosi. Our Dermatol Online. 2017;8:229-30.
2. Wilkinson, AJ, Nader ME, Roberts D, Duvic M, Gunther JR, Dabaja BS, et al. Survival outcomes of patients with mycosis fungoides involving the external ear and ear canal. Laryngoscope. 2022 Aug 31. doi:10.1002/lary.30377.
3. Bauman TM, Wichterman CM, Musiek AC, Nemer KM. Hoarseness as a presentation of mycosis fungoides infiltrating the larynx. BMJ Case Reports. 2017;2017:bcr2017221531.
4. Delgado AC, Marco FA, Martínez NS, GassóCS. T Cell Non-Hodgkin’s lymphoma of the external auditory canal. Acta Otorrinolaringologica. 2008;59:200-01.
5. Sajjan V, Chandela M, Pandit AM, Manjunathswamy B. Mycosis fungoides:The great imitator. Our Dermatol Online. 2015;6:76-9.
6. El Amraoui M, Hjira N, Ismaili N, Boui M, Senouci K. Neglected mycosis fungoides transformed into cutaneous CD30?T-cell lymphoma. Our Dermatol Online. 2021;12:88-9.
7. Elloudi S, Mrabat S, Baybay H, Douhi Z, El Fakir S, Mernissi FZ. Dermoscopy of mycosis fungoides:A study on 31 patients. Our Dermatol Online. 2021;12:257-61.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0006-6042-0236 http://orcid.org/0009-0006-6042-0236 http://orcid.org/0000-0001-8688-190X http://orcid.org/0000-0001-8688-190X http://orcid.org/0000-0002-2927-4983 http://orcid.org/0000-0002-2927-4983 http://orcid.org/0000-0003-0231-1665 http://orcid.org/0000-0003-0231-1665 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0002-5204-0528 http://orcid.org/0000-0002-5204-0528 |





Comments are closed.