Vulvar dermatofibrosarcoma of Darier and Ferrand in a young woman: About a new observation
Niare Ndour 1, Abdou Niass2, Mor Ndack Mbengue3, Saër Diadie4, Amadou Badji5, Mamadou Ba1, Ahma Gaye1, Fatimata Ly6
1, Abdou Niass2, Mor Ndack Mbengue3, Saër Diadie4, Amadou Badji5, Mamadou Ba1, Ahma Gaye1, Fatimata Ly6
1Department of Internal Medicine and Dermatology, Cheikh Ahmadoul Khadim Hospital, Touba, Senegal, 2Surgery Department, Cheikh Ahmadoul Khadim Hospital, Touba, Senegal, 3Anatomopathology Laboratory, Cheikh Anta Dop University, Dakar, Senegal, 4Dermatology Department, Aristide Le Dantec Hospital, Dakar, Senegal, 5Gynecology Department, Cheikh Ahmadoul Khadim Hospital, Touba, Senegal, 6Department of Dermatology, Hospital Institut d’Hygiène Social, Dakar, Senegal
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Darier and Ferrand Dermatofibrosarcoma is a rare mesenchymal tumor in young adults, often located in the trunk. We report an observation of a vulvar localization of dermatofibrosarcoma Darier and Ferrand. It was a young patient, aged 25, who presented a tumor of the vulvar region. This tumor has been evolving for about 10 years in two phases, the first of which is longer, with very slow development, and a second phase characterized by rapid growth of the tumor coinciding with the start of pregnancy. The examination noted a tumor developed at the expense of the vulvar region. The diagnosis of dermatofibrosarcoma was retained in view of a characteristic histopathological appearance. The treatment consisted of resection surgery with margins of about 5 cm followed by reconstruction by direct suture. The evolution, in the immediate aftermath, was good. Vulvar localization of dermatofibrosarcoma is possible.
Key words: Darier and Ferrand dermatofibrosarcoma, Vulva, Young woman
INTRODUCTION
Dermatofibrosarcoma of Darier and Ferrand is a rare fibroblastic mesenchymal tumor characterized by slow progression, high potential for local recurrence, and rare metastasis [1]. It usually appears in young adults and is located with predilection in the trunk and proximal extremities. Vulvar localization is a rare entity, described in only about fifty cases in the literature [2]. We report a new observation of a vulvar localization of a Dermatofibrosarcoma of Darier and Ferrand in a young woman.
CASE REPORT
This was a 25-year-old woman, married and mother of 3 children, the last of whom was 2 months old, with a history of spontaneous abortion during her first pregnancy, who was seen in consultation for a vulvar tumor.
The history of the disease would go back to about 10 years with the occurrence of a small lesion that appeared after a fall from a height of about 1 m with impact of the genitals on an object. The lesion would evolve very slowly during the first years until the beginning of the pregnancies. Then it starts to increase in volume as the pregnancies follow one another. There were no symptoms, in particular, there was neither pain nor pruritus, but there was a hindrance to sexual activity with a fairly significant psychological impact. The evolution would have accelerated during the last pregnancy with an increase in the volume of the tumor which had become very important at the end of the pregnancy. The patient, after vaginal delivery in an obstetrical environment, was referred to our department for better care.
On admission, the patient was conscious and in good general condition with a Glasgow score of 15/15. The dermatological examination revealed a genital tumor measuring approximately 10 cm, painless to palpation, of firm consistency, located at the level of the left lip, with superior development towards the pubis, erasing the vulvar relief and hindering the opening of the vaginal orifice. There was no discharge or genital ulceration (Fig. 1). Examination of the spleno-ganglionic system did not show any adenopathy at the inguinal level or at other sites. The rest of the clinical examination was normal.
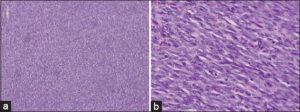
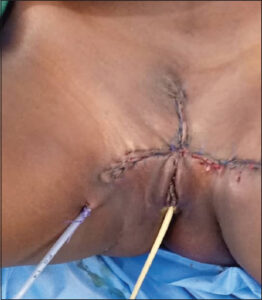
A biopsy was performed and showed a sarcomatous proliferation with spindle-shaped cells containing elongated and moderately dyskaryotic nuclei with elongated cytoplasm. Examination noted a storiform arrangement of tumor cells with a fishbone appearance. Mitoses were few, less than 10 mitoses per 10 fields at high magnification. The stroma was fibrillar and the surface epithelium was regular (Figgs. 2a and 2b). The diagnosis of dermatofibrosarcoma of Darier and Ferrand was thus retained. An extension workup was performed and included a thoraco-abdomino-pelvic CT scan which showed a suspicious vulvar mass, lateralized to the left, measuring 45×39 mm, strongly enhanced by contrast medium, without infiltration of the perineal region, nor extension to the vaginal level. In addition, there was no suspicious lesion of secondary appearance in the thoraco-abdomino-pelvic region. In a multidisciplinary consultation meeting (RCP), the decision was made to perform excision surgery followed by neoadjuvant radiotherapy. The patient underwent a monobloc excision with wide margins of 5 cm except for the clitoris and the urethra where the margins were reduced to 2 cm. Then, a reconstruction by simple suture was performed (Fig. 3). Anatomopathological examination of the excision specimen confirmed the diagnosis of Darier and Ferrand dermatofibrosarcoma and showed healthy resection margins. The postoperative course was good with complete healing and a reduction of the vaginal perimeter but without functional damage to the organs of the region such as the clitoris and the urethra. Neoadjuvant radiotherapy was not performed. Surveillance was instituted including, at least, a clinical examination every 3 to 6 months for at least 3 years.
DISCUSSION
Dermatofibrosarcoma was first described by Taylor in 1890 and individualized as a true anatomoclinical entity in 1924 by Jean Darier and Marcel Ferrand [3]. It is a tumor with a dermal origin, of intermediate malignancy between fibroma and true sarcoma. It represents less than 2% of all soft tissue sarcomas [4]. The young age of our patient, who was 25 years old at the time of diagnosis, corroborates the data in the literature, which report the occurrence of this tumor in young adults aged, on average, between 28 and 47 years [5,6]. However, the tumor has been reported to evolve since adolescence, i.e., around the age of 15 years, which corresponds to a younger age of onset. Cases of dermatofibrosarcoma with pediatric onset have been reported [7]. This late diagnosis would be due to the very slow rate of development of dermatofibrosarcoma, which remained asymptomatic for a long time. The evolution would have been accelerated by the pregnancies with a growth which would be more rapid during the last pregnancy. A probable accelerating role of pregnancy on Darier and Ferrand dermatofibrosarcoma is suggested by some authors [8]. Moreover, the notion of previous trauma, as noted in our observation, is reported in the literature, without a precise explanation being given as to the role of trauma in the occurrence of Darier and Ferrand dermatofibrosarcoma [5,9]. However, an accelerating role of trauma on the growth of dermatofibrosarcoma is well established [10]. This seems to be confirmed in our case, where a more rapid growth was noted during the pregnancies and which, on the one hand, could be linked to the trauma generated by the various successive vaginal deliveries.
This condition may be located on any organ, but it affects the trunk with predilection [11], then the limbs, head and neck [5]. Vulvar localization is rare, described mostly in isolated cases in the literature [2].
Clinically, there is great variability in its presentation. Initially, the appearance is that of a small nodule or a single firm plaque. This initial lesion slowly grows over several months or years to a painless tumor formation. At a more advanced stage, the plaque spreads, the surface becomes irregular, bumpy, realizing after some time a multinodular, polychromatic mass of variable size or sometimes uninodular. We presented a case of uninodular, protuberant dermatofibrosarcoma of Darier and Ferrand with taut, shiny and erythematous skin giving the impression of imminent fistulization. However, despite this rather characteristic clinical presentation, the diagnosis of certainty is based on anatomopathological examination, which classically shows a proliferation of dense, spindle-shaped cells of regular size, most often organized in tangled bundles in all directions, adopting a swirling or storiform structure. These cells have an oval nucleus, with dense granular chromatin, without major atypia and with rare mitoses. The proliferation is monomorphic and intradermal invading all the dermis, then it infiltrates deeply and invades the hypodermis. The tumor is poorly limited and lacks its own capsule and the central area is more cellular than the periphery. The epidermis is usually thinned [12]. However, despite this very suggestive description, histopathologic distinction between Darier and Ferrand dermatofibrosarcoma and other spindle cell tumors such as histiocytofibroma, fibrosarcoma, and nodular fasciitis is sometimes difficult. In these cases, the use of immunohistochemistry techniques is necessary to make the diagnosis. Indeed, dermatofibrosarcoma tumor cells consistently express CD34, but not PS100 or factor XIIIa [13]. However, this marker is not specific to dermatofibrosarcoma and can be expressed by other tumors such as fibromas, fibromyxomas and Kaposi’s disease [14].
The reference treatment today remains excisional surgery, which should be performed in monobloc with resection margins of at least 4 cm, down to the fascial plane in depth [15]. An alternative to this wide surgery is the Mohs micrographic technique, which involves an extemporaneous examination and 3 cm margins [16]. It offers the main advantage of removing the entire tumor with the smallest possible margin of safety, but its disadvantage is its high cost and the longer duration of the procedure. Our patient was operated on using an excisional technique with wide margins, 5 cm except for the clitoris and the urethra to preserve the function of these two organs. The anatomopathological examination of the surgical specimen showed healthy resection margins.
The other challenge in the therapeutic management of these tumors remains reconstruction after removal. This is an essential aspect given the importance of the loss of substance caused by the surgery of these tumors, in a sensitive anatomical region because it includes essential organs whose destruction leaves important unaesthetic and functional sequelae. Several reconstruction techniques are available, including direct suture, thin skin grafting, and flap grafting [17]. The latter is more suitable for covering large losses of substance [18]. In our case, the reconstruction was done by direct suture leaving part of the vaginal orifice free.
Recurrence is one of the essential characteristics of Darier and Ferrand’s dermatofibrosarcoma and it is essential to take it into account in the therapeutic decision. It may occur several years after excision and is more frequent when the margins are reduced [17]. This is why, to reduce this risk, complementary treatments are sometimes proposed. For example, some authors have used radiotherapy for recurrent tumors [19]. Oral imatinib mesylate is a tumor cell-targeted therapy that has also been used in recurrent, metastatic or unresectable tumors with encouraging results [20]. In our case, neoadjuvant radiotherapy was proposed in a multidisciplinary consultation meeting but not performed because of technical failure.
The absence of lesions suspected of metastasis in our observation is in agreement with the data of the literature which report the rarity of metastasis in Darier and Ferrand dermatofibrosarcoma. However, the follow-up was not sufficient to appreciate their existence because metastases are described as occurring on average 6 years after the first tumor removal [17]. The evolution of the postoperative course was good in our case, at the cost of an amputation of part of the affected vulva. On the other hand, considering the high potential of recurrence of Dermatofibrosarcoma, a surveillance was instituted including a clinical examination every 3 months, then every 6 months during the first 3 years [1].
CONCLUSION
Dermatofibrosarcoma of Darier-Ferrand is a rare tumor of intermediate and local malignancy, exposing to the risk of recurrence. Our observation confirms the possibility of a vulvar localization of this pathology that should be evoked in front of any vulvar tumor in a young woman. Surgery is the cornerstone of treatment but it must face the challenge of safeguarding the function of the organs in the region.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Monnier D, Algros MP, Vidal MC, Danzon A, Pelletier F, Puzenat E, et al. Dermatofibrosarcoma protuberans (Darier et Ferrand tumor):A retrospective descriptive epidemiological study in Franche-Comtéover a 20-year period (1982-2002). In:Annales de Dermatologie et de Vénéréologie. Elsevier Masson;2005. 607.
2. Nguyen AH, Detty SQ, Gonzaga MI, Huerter C. Clinical features and treatment of dermatofibrosarcoma protuberans affecting the vulva:a literature review. Dermatol Surg. 2017;43:771-4.
3. Taylor RW. Sarcomatous tumors resembling in some respects keloids. Arch Dermatol. 1890;8:3847.
4. Malhotra B, Schuetze SM. Dermatofibrosarcoma protruberans treatment with platelet-derived growth factor receptor inhibitor:a review of clinical trial results. Current opinion in oncology. 2012;24:419-24.
5. HB T, EB H. Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer. 1962;15:717-25.
6. Kasse A, Dieng M, Deme A, Fall MC, Drabo B, Timbely G, et al. Dermatofibrosarcomas of darier and ferrand, about 22 cases and review of the literature. Médecine d’Afrique Noire. 1999;46:222-7.
7. Chicaud M, Frassati-Biaggi A, Kaltenbach S, Karanian M, Orbach D, Fraitag S. Dermatofibrosarcoma protuberans, fibrosarcomatous variant:A rare tumor in children. Pediatr Dermatol. 2021;38:217-22.11.
8. Parlette LE, Smith CKJ, Germain LM, Rolfe CA, Skelton H. Accelerated growth of dermatofibrosarcoma protuberans during pregnancy. J Am Acad Dermatol. 1999;41:778-83.
9. Bashara ME, Jules KT, Potter GK. Dermatofibrosarcome protuberans:4 years after a local trauma. J Foot Surg. 1992;31:160-5.
10. Preaux J, Texier M. How serious is Darier et Ferrand’s dermatofibrosarcoma?What about its malignancy. Ann Dermatol Syphilol. 1970;97:49.
11. Bendix-Hansen K, Myhre-Jensen O, Kaae S. Dermatofibrosarcome protuberans:a clinico-pathological study of nineteen cases and review of world literature. Scan J Plast Reconstr Surg. 1983;17:247-52.
12. Hao X, Billings SD, Wu F, Stultz TW, Procop GW, Mirkin G, et al. Dermatofibrosarcome protuberans:update on the diagnosis and treatment. JCM. 2020;9:1752.
13. Mentzel T, Beham A, Katenkamp D, Dei Tos AP, Fletcher CD. Fibrosarcomatous (“high-grade ”) dermatofibrosarcoma protuberans:clinicopathological and immunohistochemical study of a series of 41 cases. With emphasis on the prognostic significance. The American journal of surgical pathology. 1998;22:576-87.
14. Haycox CL, Odland PB, Olbricht SM, Piepkorn M. Immunohistochemical characterization of dermatofibrosarcoma protuberans with practical applications for diagnosis and treatment. Journal of the American Academy of Dermatology. 1997;37:438-44.
15. Arnaud EJ, Perrault M, Revol M, Servant JM, Banzet P. Traitement chirurgical du dermatofibrosarcome protuberans. Plastic and reconstructive Surgery. 1997;100:884-95.
16. Chaput B, Filleron T, Le Guellec S, Meresse T, Courtade-Saïdi M, Grolleau JL, et al. Dermatofibrosarcome protuberans:margins reduction using slow-Mohs micrographic surgery. Expérience avec 35 patients. In:Annales de Chirurgie Plastique Esthétique. Elsevier;2014. 219-25.
17. Gattoni M, Tiberio R, Angeli L, Bornacina G, Boggio P, Annali G, et al. Dermatofibrosarcoma of Darier-Ferrand:treatment by the Tübingen surgical technique (31 cases). Annals of Dermatology and Venereology. 2007;134:31-4.
18. Brabant B, Revol M, Vergote T, Servant JM, Banzet P. Dermatofibrosarcoma protuberans of the thorax and shoulder:Wide and deep excisions with immediate reconstruction. Plastic and Reconstructive Surgery. 1993;92:459-62.
19. Snow SN, Gordon EM, Larson PO, Bagheri MM, Bentz ML, Sable DB. Dermatofibrosarcome protuberans:A report on 29 patients treated by Mohs micrographic surgery with long-term follow-up and review of the literature. Cancer. 2004;101:28-38.
20. McArthur GA, Demetri GD, van Oosterom A, Heinrich MC, Debiec-Rychter M, Corless CL, et al. Molecular and Clinical Analysis of Locally Advanced Dermatofibrosarcoma Protuberans Treated With Imatinib:Imatinib Target Exploration Consortium Study B2225. JCO. 2005;23:866-73.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0001-9687-3970 http://orcid.org/0000-0001-9687-3970 http://orcid.org/0009-0002-9902-117X http://orcid.org/0009-0002-9902-117X http://orcid.org/0000-0001-9770-1118 http://orcid.org/0000-0001-9770-1118 http://orcid.org/0009-0002-2949-0245 http://orcid.org/0009-0002-2949-0245 http://orcid.org/0000-0003-4132-9315 http://orcid.org/0000-0003-4132-9315 |





Comments are closed.