Impact of the COVID-19 pandemic on monitoring people living with HIV in Dakar, Senegal
Boubacar Ahy Diatta , Chaymae Yousfi, Pie Nibirantije, Patrice Mendy, Niare Ndour, Ndiague Fall, Khadim Diop, Mamadou Sarr, Coumba Ndiaye, Saer Diadie, Maodo Ndiaye, Assane Diop, Moussa Diallo, Fatimata Ly, Suzanne Oumou Niang
, Chaymae Yousfi, Pie Nibirantije, Patrice Mendy, Niare Ndour, Ndiague Fall, Khadim Diop, Mamadou Sarr, Coumba Ndiaye, Saer Diadie, Maodo Ndiaye, Assane Diop, Moussa Diallo, Fatimata Ly, Suzanne Oumou Niang
Department of Dermatology, Cheikh Anta Diop University of Dakar, Senegal
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The COVID-19 pandemic has had a considerable impact on chronic disease monitoring. Previous work has asserted that people living with HIV (PLHIV) are at risk of developing COVID-19 and have difficulty accessing care and antiretroviral (ARV) treatment. The aim of this study was to determine the prevalence of HIV/COVID-19 co-infection and vaccination and to assess the impact of the pandemic on the follow-up of PLHIV and on their psychosocial and economic lives.
Materials and Methods: This was a cross-sectional, multicenter study conducted from August 16, 2021, to October 10, 2021, at two dermatology departments of Dakar. We included all PLHIV followed at these two services during the study period.
Results: We identified 57 cases of PLHIV. The hospital frequency was 6.44%, the mean age was 46, and the sex ratio was 0.54. The prevalence of COVID-19 infection was 14.1%. All cases had a mild clinical form of COVID-19, outpatient management, complete remission, and no deaths were noted during the follow-up. Viral load was available and undetectable in 25%. All patients co-infected with HIV/COVID-19 were on antiretroviral therapy. The prevalence of PLHIV vaccinated against COVID-19 was 31.6%. During the COVID-19 pandemic, 28.1% of cases missed their appointments. 96.5% of cases accessed to ARV treatment. However, 3.5% of PLHIV stopped their ARV treatment for reasons unrelated to the COVID-19 pandemic. Opportunistic infections were present in 31.6% of cases, with a significant impact on psychological (64.9%), social (45.6%), and economic (71.9%) well-being, as well as on quality of life in 59.6% of cases.
Conclusion: The COVID-19 pandemic and its health measures have had a major impact on the follow-up and quality of life of people living with HIV. The reinforcement of therapeutic education, barrier measures, and COVID-19 vaccination seem to contribute to improving the quality of life of PLHIV.
Key words: HIV, COVID-19, Psychosocial impact
INTRODUCTION
Human immunodeficiency virus (HIV) infection is a major public health problem. In 2020, there was an estimated 37.6 million HIV-positive people in the world, 27.4 million of whom was estimated to have access to antiretroviral (ARV) treatment [1]. In Africa, there was an estimated 25.3 million people living with HIV (PLHIV) in 2020, 18.5 million (73.1%) of whom had access to ARV treatment. In Senegal, an estimated 39,400 people were living with HIV in 2020. The HIV epidemic was widespread, with low prevalence in the general population and high prevalence in certain localities and among the most vulnerable populations [2]. The advent of the COVID-19 pandemic led to considerable disruption of health services in many countries, with people restricted in their movements and care suspended. Elderly people and those with chronic illnesses such as HIV were exposed to severe manifestations of COVID-19 [3]. These resource-limited countries have inadequate healthcare infrastructures, which could increase the risk of COVID-19-related mortality [3,4]. The COVID-19 pandemic and its sanitary measures led to disruptions in health services, particularly in centers for monitoring and caring for people living with HIV. The consequences were a reduction or suspension of care and supply of antiretroviral drugs in some countries [5]. The pandemic also had a psychosocial and economic impact on patients’ quality of life. The most commonly reported consequences were depression, reduced food security, and economic decline [6]. The aims of our study were to determine the prevalence of COVID-19 infection in PLHIV and to assess the psychological, social, and economic impact of COVID-19 on people living with HIV.
MATERIALS AND METHODS
This study was transversal and multicentric and was conducted at the dermatology departments of Aristide Le Dantec Hospital and the Hygiena Sociale Institute for about two months (from August 16, 2021, to October 10, 2021). All PLHIV followed at these two departments during the period were included. HIV infection was confirmed by retroviral serology and COVID-19 infection by polymerase chain reaction. Data was collected using a survey form that recorded socio-professional and medical data concerning the usual follow-up of HIV and COVID-19 infection. Data was processed with Epi-Info 7 and analyzed with SPSS Statistics 26.
RESULTS
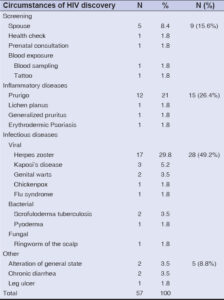
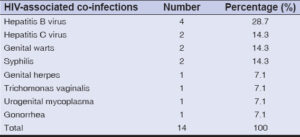
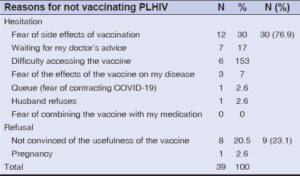
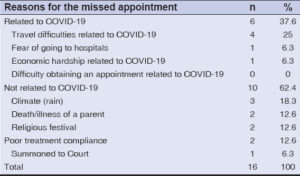
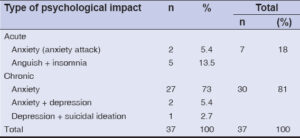
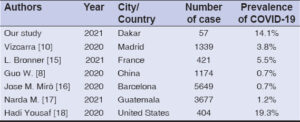
We identified 57 patients living with HIV, representing a hospital frequency of 6.4%. The mean age was 47 years, with extremes of 25 and 69 years. The 40–60 age group was the most represented. The sex ratio was 0.5. The majority of PLHIV were shopkeepers (24.6%) and housewives (37%). Socioeconomic status was low to medium in 87.8% of the cases. The geographical origin (Fig. 1) of the patients was 55 cases from Senegal, one case from Guinea Conakry, and one case from Guinea Bissau. The patients’ serological status was 89.5% in HIV1 and 10.5% in HIV2. Fig. 2 shows the average length of follow-up. The causes of HIV infection were 49.2% from infectious diseases, 26.4% from inflammatory dermatoses, and 15.6% from screening (Table 1). Viral load was undetectable in 24.5%. Other HIV-associated sexually transmitted infections were noted in 14 cases (Table 2). Table 3 illustrates antiretroviral treatment administered to the patients according to national protocols. HIV infection was associated with COVID-19 infection in 14.1% of cases. All PLHIV had a mild form of COVID-19 symptoms with outpatient management and complete remission. The rate of vaccination of PLHIV with COVID-19 was noted to be 31.6% (Table 4). Adverse events were noted in 27.3% of the cases. The reasons for refusing vaccination are shown in Table 5. In terms of regular follow-up, missed appointments were noted in 28.1% of the cases. Duration of follow-up was less than one month in 62.2% of the cases, between 2 and 6 months in 25.2%, and over 10 months in 12.6%. The reasons for missed appointments were related to COVID-19 in 37.6% of the cases (Table 6). Access to ARV treatment was assured in 96.5% of the cases. The occurrence of opportunistic infections was noted in 31.6% of the cases. Psychological impact was noted in 64.9% of the cases, with anxiety and depression associated with suicidal ideation. Table 7 shows the distribution of patients according to psychological impact. Psychological support was provided by experienced psychiatrists in 94.7% of the cases. On the social front, 45.6% of the patients had a worsening perception of loneliness. The reasons were stigmatization, social isolation, financial difficulties linked to COVID-19, and psychosocial stress. On the economic front, financial difficulties were noted in 41 cases. This included loss of employment reduced monthly income and expensive hospitalization costs. Quality of life was impaired in 34 cases (59.6%), with mood disorders and stress. Alcohol and cigarette abuse were noted in two cases.
 |
Figure 1: Distribution of the patients by geographic origin. |
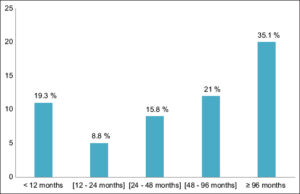 |
Figure 2: Follow-up duration of the PL HIV. |
DISCUSSION
We report the first study to assess the psychosocial and economic impact of COVID-19 on the follow-up of PLHIV at dermatological care centers Senegal. The majority of studies have been conducted in developed countries [7–14]. The limitation of our study was our small sample size, which was linked to the reduced number of consultations during the COVID-19 pandemic. Nevertheless, we noted a 14.1% prevalence of COVID-19 infection among people living with HIV. We noted a higher frequency of COVID-19 in PLHIV compared with previous studies reported in the literature (Table 8). In our series, the clinical form of COVID-19 disease was mild in all patients. No severe forms were noted. The patients were managed on an outpatient basis. Several studies have reported that COVID-19-related mortality in PLHIV does not differ from that in the general population [18–20]. The high mortality rate reported in other studies seems to be linked to the advanced age of PLHIV, the existence of several co-morbidities, a high plasma viral load, and irregular intake of antiretroviral treatment [18–20]. In our study, PLHIV infected with COVID-19 had an average age of 45 years, with no sex predominance. These results were similar to those reported in the literature [13,21,22,26]. Viral load was available and undetectable in 25% of PLHIV with COVID-19 infection. Some authors report that PLHIV who are on antiretroviral treatment and have a satisfactory immuno-virological status do not present a higher risk of severe COVID-19 infection. Their prognosis was identical to that of the general population with the same comorbidities. However, close monitoring of viral load at one month of COVID-19 infection is questionable in these patients [23].
Vaccinated PLHIV represented 31.6%, among which 83.3% had completed their vaccination dose. AstraZeneca, Sinopharm, and Janssen vaccines were used due to their availability in our country. Side effects of vaccination in PLHIV were present in 27.3% of the cases, with most minor. The choice of vaccination was influenced by misinformation spread through social networks, collective denial, and religious beliefs. The low rate of PLHIV vaccinated at the beginning of the COVID-19 vaccination campaign could be explained by the difficulty in access to vaccines [4]. In our series, the rate of PLHIV vaccinated gradually increased thanks to the availability of vaccines and awareness campaigns. Concerning the impact of the COVID-19 pandemic on the follow-up of PLHIV, we noted that 28.1% were absent from appointments. Motivations were unrelated to the COVID-19 pandemic in 62.4% of the cases, and those related to COVID-19 were attributed to health restrictions on inter-city travel, hospital phobia, and financial difficulties linked to COVID-19. Some authors report that the implementation of telemedicine ensured continuity of patient care during a pandemic and reduced the risk of exposure to COVID-19 [24]. The circumstances of transmission of HIV infection were dominated by skin manifestations in 75.6% and screening in 15.6%, which is in line with the literature. Psychologically, there was an impact on the mental health of PLHIV in 64.9% of the cases. These results were also reported in the U.S. and Peru [25–27]. In Senegal, psychological support was provided in 94.7% of cases. Socially, the perception of loneliness increased in 45.6% during the pandemic. In Peru, the prevalence of perceived loneliness, stigmatization, and rejection increased by over 50% [28]. An economic impact was noted in 71.9%. In Indonesia, many patients lost their jobs as a result of COVID-19 [5]. In Peru, 71% of the economically active population was forced to accept informal jobs with no fixed salary [29]. The quality of life of PLHIV was impaired in 59.6%. Isolation, unemployment and financial loss had a negative impact on the quality of life of PLHIV. In our study, 3.5% of patients used tobacco and alcohol to cope with stress. Tobacco and alcohol abuse were also reported by some authors during the COVID-19 pandemic [25,30].
CONCLUSION
The COVID-19 pandemic has had considerable repercussions on the follow-up of patients living with HIV in Senegal. A psychosocial and economic impact was noted in the study. Multidisciplinary management and therapeutic patient education helped to improve the patients’ quality of life and ensure continuity of care. Sentinel epidemiological surveillance in terms of virology proves useful in preventing such endemics.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. ONUSIDA. “Dernières statistiques sur l’état de l’épidémie de sida ”. unaids.org. Estimations épidémiologiques de l’ONUSIDA 2021. https://www.unaids.org/fr/resources/fact-sheet.
2. Conseil National de Lutte contre le Sida. “Rapport annuel 2020 ”. cnls-senegal.org. CNLS, juin 2021. https://www.cnls-senegal.org/bibliotheque/rapports.
3. The Centers for Disease Control. People at increased risk and other people who need to take extra precautions. 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions.
4. COVID-19 Dashboard by the Center for Systems Science and Engineering at. Johns Hopkins University;2020. https://coronavirus.jhu.edu/map.html.
5. Luis H, Fridayantara WD, Mahariski P, Wignall FS, Irwanto I, Gedela K. Evolving ART crisis for people living with HIV in Indonesia. Lancet HIV. 2020;7:384-5.
6. Walker PGT, Whittaker C, Watson OJ, Baguelin M, Winskill P, Hamlett A, et al. The impact of COVID-19 and strategies for Mitigation and suppression in low. and middle. income countries. Science. 2020;369:413-22.
7. Zhu F, Cao Y, Xu S, Zhou M. Co-infection of SARS-CoV-2 and HIV in a patient in Wuhan city, China. J Med Virol. 2020;92:529-30.
8. Guo W, Ming F, Dong Y, Zhang Q, Zhang X, Mo P, et al. A survey for COVID-19 among HIV/AIDS patients in two districts of Wuhan, China. SSRN Electronic J. 2020:19.
9. Blanco JL, Ambrosioni J, Garcia F, Martinez E, Soriano A, Mallolas J et al. COVID-19 in patients with HIV:Clinical case series. Lancet HIV. 2020;7:314-6.
10. Vizcarra P, Perez-Elias MJ, Quereda C, Moreno A, Vivancos MJ, Dronda F, et al. Description of COVID-19 in HIV-infected individuals:A single-center, prospective cohort. Lancet HIV. 2020,7:554-64.
11. Haerter G, Spinner CD, Roider J, Bickel M, Krznaric I, Grunwald S, et al. COVID-19 in people living with human immunodeficiency virus:A case series of 33 patients. Infection. 2020,11:1-6.
12. Gervasoni C, Meraviglia P, Riva A, Giacomelli A, Oreni L, Minisci D, et al. Clinical features and outcomes of HIV patients with coronavirus disease 2019. Clin Infect Dis. 2020.71:2276-8.
13. Ridgway JP, Schmitt J, Friedman E, Taylor M, Devlin S, McNulty M, et al. HIV Care continuum and COVID-19 outcomes among people living with HIV during the COVID-19 pandemic, Chicago, IL. AIDS Behav. 2020;24:2770-2.
14. Ridgway JP, Farley B, Benoit JL, Frohne C, Hazra A, Pettit N, et al. A case series of five people living with HIV hospitalized with COVID-19 in Chicago, Illinois. AIDS Patient Care STDs. 2020;34:331-5.
15. Bronner L, Robineau O, Ajana F, Huleux T, Schmit JL, et al. Évaluation de l’impact de la pandémie de la COVID-19 chez les patients vivants avec le VIH. Infectious Diseases. 2021;51:128-9.
16. MiróJM, Ambrosioni J, Blanco JL. COVID-19 in patients with HIV:Authors’reply. Lancet HIV. 2020;7:383-4.
17. Medina N, Alastruey-Izquierdo A, Bonilla O, Ortíz B, Gamboa O, Salazar L, et al. Impact of the COVID-19 pandemic on HIV care in Guatemala. Int J Infect Diseases. 2021;108:422-7.
18. Hadi YB, Naqvi SF, Kupec JT, Sarwari AR. Characteristics and outcomes of COVID-19 in patients with HIV:A multicenter research network study. Aids. 2020;34:3-8.
19. Costenaro P, Minotti C, Barbieri E, Giaquinto C, DonàD. SARS-CoV-2 infection in people living with HIV:a systematic review. Rev Med Virol. 2021;31:1-12.
20. Sigel K, Swartz T, Golden E, Piranjpe I, Somani S, Richter F, et al. COVID-19 and people with HIV infection:Outcomes for hospitalized patients in New York City. Clin Infect Dis. 2020;71:2933-8.
21. Huang Y, Tu M, Wang S, Chen S, Zhou W, Chen D, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China:A retrospective single center analysis. Travel Med Infect Dis. 2020;36:101-606.
22. Altuntas Aydin O, Kumbasar Karaosmanoglu H, Kart Yasar K. HIV/SARS-CoV-2 co-infected patients in Istanbul, Turkey. J Med Virol. 2020;92:2288-90.
23. Suwanwongse K, Shabarek N. Clinical features and outcome of HIV/SARS-CoV-2 coinfected patients in The Bronx, New York City. J Med Virol. 2020;92:2387-9.
24. Siwicki B. Telemedicine during COVID-19:Benefits, limitations, burdens, adaptation. Health Care News. 2021.
25. Janoczkin A, Kiers S, Edara N, He P, Li Y. Impact of COVID-19 pandemic on emergency psychiatry:Millcreek community hospital, Erie, PA. Compr Psychiatry. 2021;110:152-255.
26. Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events:Lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53:15-23.
27. Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic:A call for action for mental health science. Lancet Psychiatry. 2020;7:547-60.
28. Zafra-Tanaka JH, Ticona-Chavez E. [Stigma related to HIV/AIDS associated with adherence to antiretroviral therapy in patients of a public hospital in Lima, Peru 2014]. Rev Peru Med Exp Salud Publica. 2016;33:625-32.
29. Paredes JL, Navarro R, Cabrera DM, Diaz MM, Mejia F, Caceres CF. [Challenges to the continuity of care of people living with HIV throughout the COVID-19 crisis in Peru]. Rev Peru Med Exp Salud Publica. 2021;38:166-70.
30. Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, Dubey S. COVID-19 and addiction. Diabetes Metab Syndr. 2020;14:817-23.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0001-8923-0790 http://orcid.org/0000-0001-8923-0790 http://orcid.org/0000-0002-1624-0274 http://orcid.org/0000-0002-1624-0274 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0002-0749-0888 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-4550-3704 http://orcid.org/0000-0003-4550-3704 http://orcid.org/0000-0002-9325-4784 http://orcid.org/0000-0002-9325-4784 http://orcid.org/0000-0001-9770-1118 http://orcid.org/0000-0001-9770-1118 http://orcid.org/0000-0001-5812-2770 http://orcid.org/0000-0001-5812-2770 http://orcid.org/0000-0002-2910-8416 http://orcid.org/0000-0002-2910-8416 http://orcid.org/0000-0002-8245-6372 http://orcid.org/0000-0002-8245-6372 http://orcid.org/0000-0003-4132-9315 http://orcid.org/0000-0003-4132-9315 |





Comments are closed.