Epidemiological, clinical, and therapeutic aspects of dermatitis herpetiformis at Yalgado Ouédraogo University Hospital Centre, Burkina Faso
Muriel Sidnoma Ouédraogo 1,2, Djimtibaye Djounitanan1, Nomtondo Amina Ouédraogo1,2, Gilbert Patrice Marie Louis Tapsoba1,2, Angèle Ouangré/Ouédraogo1, Nina Korsaga/Somé2,3, Jean-Baptiste Andonaba4, Fatou Barro/Traoré2,5, Pascal Niamba1,2, Adama Traoré1,2
1,2, Djimtibaye Djounitanan1, Nomtondo Amina Ouédraogo1,2, Gilbert Patrice Marie Louis Tapsoba1,2, Angèle Ouangré/Ouédraogo1, Nina Korsaga/Somé2,3, Jean-Baptiste Andonaba4, Fatou Barro/Traoré2,5, Pascal Niamba1,2, Adama Traoré1,2
1Department of Dermatology-Venereology Yalgado Ouédraogo University Hospital (YO UH), Ouagadougou, Burkina Faso, 2Health Science Training and Research Unit, Joseph Ki-Zerbo University, Ouagadougou, Burkina Faso, 3Department of Dermatology Venerology, Boulmiougou District Hospital, Ouagadougou, Burkina Faso, 4Department of Dermatology Venerology Souro Sanon University Hospital, Ouagadougou, Burkina Faso, 5Department of Dermatology Venerology, Tengandogo University Hospital, Ouagadougou, Burkina Faso
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Dermatitis herpetiformis is a rare autoimmune bullous dermatosis that predominantly affects Caucasians, adults or children, with a sex ratio of 1.8.
Materials and Methods: The aim of this study was to document the clinical and epidemiological profiles of dermatitis herpetiformis and to detail its treatment in a hospital setting in order to increase our knowledge about this disease in our context and so to improve its management. We conducted a retrospective, cross-sectional study of the records of all patients seen in consultation or hospitalized at the dermatology department of Yalgado Ouédraogo University Hospital Centre, Ouagadougou, a public hospital in Burkina Faso, from January 2016 to December 2020.
Results: We collected 14 cases (0.12%) of dermatitis herpetiformis among 11,456 patients seen. The mean age was 8 years (ranging from 4 to 27 years). The sex ratio was 1.33. The majority of the patients were schoolchildren living in rural areas (8 cases). The duration of the disease ranged from five days to one year (mean duration: 59.35 days). Eight patients had a history of digestive problems such as abdominal pain and diarrhea. Pruritis was the principal functional sign. In all patients, the lesions were polymorphous: disseminated vesicular bullae, papules, erosive, and excoriated lesions, sometimes forming clusters. Mucosal involvement was rare (3 cases). A gluten-free diet and dapsone 2 mg/kg/day were proposed to all patients and resulted in the improvement of the lesions.
Conclusion: Our study confirmed that dermatitis herpetiformis is rare in our context. It is more frequent in young children and predominantly affects boys. It is intensely pruritic, and generalized polymorphous lesions were present in all our patients. Treatment is essentially based on a gluten-free diet and dapsone, which is a therapeutic test in the absence of supplementary investigations to establish a definitive diagnosis.
Key words: Dermatitis Herpetiformis; Clinical Medicine; Dapsone; Gluten Intolerance
INTRODUCTION
Dermatitis herpetiformis (DH) is a rare, recurrent auto-immune bullous dermatosis classically associated with gluten enteropathy. It predominantly affects Caucasians, with a sex ratio of 1.8 [1]. The prevalence is higher in northern Europe, ranging from 11 to 66 cases per 100,000 inhabitants [2,3]. In Black Africa, studies of this bullous dermatosis are highly sparse. Two hospital studies conducted in the Ivory Coast and in Sudan found a prevalence of 20.9 for 100,000 patients [4] and 5 cases in 16 years [5], respectively. In view of the rarity of African data and the difficulties of diagnosis in our context, we undertook the present study to document the sociodemographic, clinical, and therapeutic aspects of DH in a hospital setting.
MATERIALS AND METHODS
This was a descriptive, cross-sectional study in which we retrospectively examined the records of patients with a clinical or histological diagnosis of DH during the five-year period from January 1, 2016, to December 31, 2020, at the dermatology and venereology department of Yalgado Ouédraogo University Hospital Centre, the national reference hospital in Ouagadougou, Burkina Faso. The variables collected were sociodemographic (age, sex, place of residence), clinical (history, gastrointestinal problems, pruritis, type of primary lesions (location), therapeutic (dapsone), and on the course of the disease (healed, stationary, death of patient, lost to follow-up).
RESULTS
Epidemiological Data
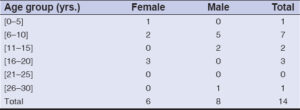
We collected 14 cases of DH among 11,456 patients who had been seen in consultation or admitted to the hospital. The prevalence of DH at the dermatology department was 0.12%. The mean age of the patients was 8 years (range: 4 to 27 years). Eight patients were male and six were female (sex ratio: 1.33). Most patients were in the 6–10 year age group (7 cases) (Table 1) and were schoolchildren (8 cases) living in a rural environment.
Clinical Data
The duration of the disease ranged from five days to one year, with a mean duration of 59.35 days. A history of gastrointestinal disturbances, such as abdominal pain and diarrhea, was observed in eight patients. Pruritis was the main functional sign observed and was present in twelve patients. The general condition remained good in ten patients. All patients presented with generalized polymorphous lesions consisting of vesicular bullae, papules, and erosive and blackish excoriated lesions in clusters in some areas (Fig. 1). Mucosal involvement was present as vesicular stomatitis (2 cases) and conjunctivitis (1 case).
Paraclinical Data
A biopsy of the bullous lesion was performed in six patients and the findings were consistent with DH in 5 cases. Four patients had anemia, as shown by a full blood count. G6PD was measured in two patients yet showed no deficiency.
Treatment
A gluten-free diet (GFD) and dapsone (2 mg/kg/day) were proposed in all patients. Systemic corticotherapy was administered in association with dapsone in one patient who did not respond to dapsone alone after one month.
Course of the Disease
After one month of treatment, six patients were clinically healed and the episode of vesicular-bullous lesions had cleared. The episode persisted in seven patients and one patient was lost to follow-up. After three months of follow-up, five patients had no recurrence of bullous lesions. A new outbreak occurred in two cases, and six patients who lived in rural areas were lost to follow-up.
DISCUSSION
Epidemiology
We recorded 14 cases (0.12%) of DH at the dermatology department of our institution during the five-year period. Kaloga et al. in the Ivory Coast and Akakpo et al. in Togo found a lower prevalence at their departments, with 7 patients in 5 years and 11 patients in 8 years, respectively [6,7]. Zaraa et al. in Tunisia observed 9 cases in 11 years [8]. Our findings confirmed the rarity of DH.
The disease predominantly affected males. Ouattara and Sidigg et al. also found a male predominance, with sex ratios of 1.56 and 1.03, respectively [4,5]. On the other hand, Akakpo et al. and Zaara et al. found a female predominance, with sex ratios of 0.8 [7] and 0.5 [8], respectively. A female predominance was also reported by Smith et al. in the U.S. [9].
The age of our patients ranged from 4 to 27 years, with a mean of 8 years. The disease was most frequent in the 6–10 year age group. This was similar to reports in the literature indicating that DH most often develops between the second and seventh year of life, as found by Ermacora et al. [10]. Other studies, however, have shown a predominance of DH in adults aged between 25.6 and 66 years [2,5,6,11].
Clinical Aspects
The duration of the disease before the specialist consultation ranged from five days to one year, with a mean of 59.35 days. This delay was long and is explained in our context by initial neglect by the patients of their skin problems, the use of phytotherapy before seeking medical advice, and the lack of access to dermatologists. This long time to diagnosis has also been reported in some developed countries, sometimes being as long as two years [12].
Pruritis was the principal functional sign, reported by the majority of the patients. In the literature, DH is classically accompanied by intense pruritis [1,4,7,13,14].
Eight patients presented with gastrointestinal signs. However, confirmatory gastrointestinal endoscopy was not performed. Akakpo et al. observed no signs of gluten enteropathy, nor did they conduct supplementary investigations to detect one [7]. Ouattara reported a case of associated coeliac disease [4]. Zaraa et al. reported two cases of coeliac disease among four patients who had undergone supplementary tests [8]. Dermatitis herpetiformis is considered as the cutaneous manifestation of gluten intolerance, invariably accompanied by coeliac disease [10,14].
Generalized polymorphous lesions were present in all our patients. The same observation was made by Akakpo et al. [7] and by Ouattara, who reported polymorphous and symmetrical lesions in 73.9% of cases [4].
Three patients (21.4%) had oral and ocular mucosal involvement. Akakpo et al. also reported such involvement in 36.4% of cases [7] and Ouattara in 17.4% [4]. Zaara et al. found no mucosal involvement [8]. It is rare in DH [1].
Paraclinical Aspects
A biopsy of the lesions was performed in six patients, and the histology was compatible with GH in five cases. Ouattara confirmed this observation in 52.2% of biopsies [4]. Histology makes little contribution to the diagnosis. The reference diagnostic test for DH is direct immunofluorescence (DIF) [1,14], which is unavailable in our context.
Treatment
A gluten-free diet was initiated in all patients. It is indispensable for the management of DH [1,14], yet is difficult to follow. Treatment with dapsone (2 mg/kg/day) was offered to the fourteen patients. This molecule is the mainstay of DH treatment [1,14,15] and was effective in obtaining rapid regression of the cutaneous signs, generally within several days.
Evolution
After three months of follow-up, seven patients who came from a rural environment were lost to follow-up. This could be explained by financial difficulties and the use of phytotherapy. Better therapeutic education could considerably reduce the number of patients lost to follow-up.
CONCLUSION
This study shows that DH is a rare disease that, in our setting, mainly affects children of school age. It usually manifests as generalized polymorphous lesions. Diagnosis is essentially clinical and management is based on dapsone, which is a diagnostic test.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Ingen-Housz-Oro S. [Dermatitis herpetiformis:A review]. Ann Dermatol Venereol. 2011;138:221-7.
2. Reunala T. Dermatitis herpetiformis. Clin Dermatol. 2001;19:728-36.
3. Gawkrodger DJ, Blackwell JN, Gilmour HM, Rifkind EA, Heading RC, Barnetson RS. Dermatitis herpetiformis:Diagnosis, diet and demography. Gut. 1984;25:151-7.
4. Ouattara GF. Aspects épidémiologiques, cliniques et paraclinique de la dermatite herpétiforme en Côte d’Ivoire. Universitéde Cocody, Côte d’Ivoire. Medical thesis n°4002;2005:112 p.
5. Siddig O, Mustafa MB, Kordofani Y, Gibson J, Suleiman AM. The epidemiology of autoimmune bullous diseases in Sudan between 2000 and 2016. PLoS One. 2021;16:e0254634.
6. Kaloga M, Ecra E, Kourouma S, Allou S, Kouassi YI, Gbery IP, et al. Panorama des dermatoses bulleuses auto-immunes (DBAI) sur peaux foncées. Revue Internationale des Sciences Médicales d’Abidjan. 2016;18:275-9.
7. Akakpo AS, Abilogun-Chokki A, Téclessou JN, Kassang P, Moise YE, Djalogue L, et al. Auto-immune bullous dermatosis in hospital in Togo:A retrospective study from 2010 to 2018. Our Dermatol Online. 2021;12(Supp. 2):1-5.
8. Zaraa I, Kerkeni N, Ishak F, Zribi H, El Euch D, Mokni M, et al. Spectrum of autoimmune blistering dermatoses in Tunisia:An 11-year study and a review of the literature. Int J Dermatol. 2011;50:939-44.
9. Smith JB, Tulloch JE, Meyer LJ, Zone JJ. The incidence and prevalence of dermatitis herpetiformis in Utah. Arch Dermatol. 1992;128:1608-10.
10. Ermacora E, Prampolini L, Tribbia G, Pezzoli G, Elmetti C, Cucchi G, et al. Long-term follow-up of dermatitis herpetiformis in children. J Am Acad Dermatol. 1986;15:24-30.
11. Salmi TT, Hervonen K, Kautiainen H, Collin P, Reunala T. Prevalence and incidence of dermatitis herpetiformis:A 40-year prospective study from Finland. Br J Dermatol. 2011;165:354-9.
12. Mansikka E, Salmi TT, Kaukinen K, Collin P, Huhtala H, Reunala T, et al. Diagnostic delay in dermatitis herpetiformis in a high-prevalence area. Acta Derm Venereol 2018;98:195-9.
13. Rabinowitz LG, Esterly NB. Inflammatory bullous diseases in children. Dermatol Clin. 1993;1:565-81.
14. Nguyen CN, Kim SJ. Dermatitis herpetiformis:An update on diagnosis, disease monitoring, and management. Medicina (Kaunas). 2021;57:843.
15. Collin P, Reunala T. Recognition and management of the cutaneous manifestations of celiac disease:A guide for dermatologists. Am J Clin Dermatol. 2003;4:13-20.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-7938-8639 http://orcid.org/0000-0002-7938-8639 http://orcid.org/0000-0002-0734-0759 http://orcid.org/0000-0002-0734-0759 http://orcid.org/0000-0002-1042-9770 http://orcid.org/0000-0002-1042-9770 |





Comments are closed.