Actinic keratosis of the eyelid: What management to avoid degeneration?
Jihad Kassel , Zakia Douhi, Chaymae Jroundi, Sara Elloudi, Hanane Baybay, Fatima-Zahra Mernissi
, Zakia Douhi, Chaymae Jroundi, Sara Elloudi, Hanane Baybay, Fatima-Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Actinic keratoses (AKs) appear on sun-exposed skin areas and are considered one of the clinical signs of cutaneous photoaging. They often present as multiple lesions that are rarely unique [1]. They are associated with considerable morbidity which may be decreased if detected and treated early. It has been shown that the risk of developing non-melanoma skin cancer is increased more than sixfold in patients with AK [2]. Dermoscopy is a rapid, non-invasive method that helps in the early diagnosis of AK, which may show erythema forming a reddish-pink vascular pseudo-network surrounding the hair follicles described as the strawberry-like pattern, yellowish-white scales, fine, wavy vessels surrounding the follicles, and follicular openings filled with keratotic plugs [3]. To treat AK and avoid the risk of degeneration, a variety of surgical and non-surgical treatments, such as cryotherapy, topical chemotherapy, chemical peels, laser therapy, and photodynamic therapy may be offered [4]. Some locations represent a therapeutic challenge, particularly in the eyelids. Indeed, on the one hand, surgical treatment, which is recognized for its effectiveness, must be performed with particular care and may be responsible for a functional alteration, ectropion with a constant risk of recurrence [1]. On the other hand, non-surgical treatments, which are often employed by dermatologists, have also shown their efficacy, yet with the possibility of side effects, such as skin erythema, superficial punctate keratitis, and conjunctival hyperemia, often leading patients to stop the treatment [2]. Generally, a large excision with reconstruction remains the method of choice to treat AK of the eyelid and to avoid an evolution toward a squamous cell carcinoma. Non-surgical treatments have also shown satisfactory results. Studies regarding the efficacy and safety of different treatments of AK are needed to determine the optimal treatment of AK in the eyelid and periocular region in order to prevent heavy functional and aesthetic ocular consequences [1]. Herein, we report the case of a patient who presented an AK of the eyelid with a dramatic evolution.
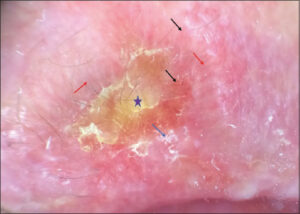
A seventy-year-old female patient, without any pathological history, presented with an erythematous lesion of the upper right eyelid evolving for one year. The patient consulted the dermatologist, who performed a skin biopsy in favor of actinic keratosis. She was treated with cryotherapy with burning and irritation at the palpebral level, which led the patient to stop the sessions. Six months later, she noted an increase in the size of the lesion with redness and tearing of the eye motivating her consultation with the ophthalmologist, who put the patient under several topical treatments without improvement, then the patient was referred to us for further management. An examination revealed an erythematous plaque on the upper right eyelid with a crusty ulceration in the center (Fig. 1). We noted an infiltration associated with erythema at the level of the free edge of the upper eyelid, the lower eyelid, and the internal cantus of the eye. Dermoscopy revealed irregular, linear vascularization with hairpin vessels, scales, and keratin (Fig. 2). The patient reported ocular discomfort with pruritus and lacrimation. The rest of the examination was normal. A biopsy was performed on our patient and found an invasive, poorly differentiated, non-keratinizing squamous cell carcinoma. A locoregional and distant extension assessment was normal and we referred the patient to the ophthalmologist, who performed the exenteration of the eye.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Richard MA, Amici JM, Basset-Seguin N, Claudel JP, Cribier B, et al. Management of actinic keratosis at specific body sites in patients at high risk of carcinoma lesions:Expert consensus from the AKTeam™of expert clinicians. J Eur Acad Dermatol Venereol. 2018;32:339-46.
2. López-Tizón E, Mencía-Gutiérrez E, Garrido-Ruíz M, Gutiérrez-Díaz E, López-Ríos F. Clinicopathological study of 21 cases of eyelid actinic keratosis. Int Ophthalmol. 2009;29:379-84.
3. Reinehr CPH, Bakos RM. Actinic keratoses:Review of clinical, dermoscopic, and therapeutic aspects. An Bras Dermatol. 2019;94:637-57.
4. Lagler CN, Freitag SK. Management of periocular actinic keratosis:A review of practice patterns among ophthalmic plastic surgeons. Ophthalmic Plast Reconstr Surg. 2012;28:277-81.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 |





Comments are closed.