Dermoscopic pattern of the topical steroid damaged face: A cross-sectional, observational study at a tertiary referral center in south India
Pappala Mamatha , Sruthi Kareddy, Haarika Sadhu
, Sruthi Kareddy, Haarika Sadhu
Department of Dermatology, Venereology and Leprosy, Vydehi Institute of Medical Sciences & Research Centre, #82, Nallurahalli, Near BMTC 18th Depot, Whitefield, Bangalore – 560 066, Karnataka, India
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Unsupervised overuse of topical corticosteroids (TCs) is highly common in dermatological practice, leading to steroid abuse known as topical steroid damaged/dependent face (TSDF). Dermoscopy aids in the early detection of TSDF.
Aims: The aim of this study was to evaluate the clinical and dermoscopic findings in patients with TSDF.
Materials and Methods: The study was conducted on eighty patients presenting with clinical features suggestive of TSDF. Detailed history taking, clinical examination, and dermoscopic evaluation with a DermLite dermoscope were performed.
Results: Out of the eighty patients included in the study, 64 (80%) were females and 16 (20%) were males. The most common age group affected was 18–30 years (52; 65%). Sixty-six were literate. Melasma was a common underlying condition for which a steroid was used by the patients (44; 55%). Betamethasone (34; 47.5%) was the most commonly used, followed by clobetasol (18; 22.5%). Relatives and friends were the common sources of recommendation (46; 57.5%). Most of the patients applied these for one year. Redness was the predominant presenting complaint, seen in sixty patients (75%). The common clinical findings were erythema (75%), hyperpigmentation (44; 55%), and hypertrichosis (50; 62.5%). The common findings observed on dermoscopy were telangiectasia (90%), red, diffuse areas (75%), brown globules (55%), and hypertrichosis (62.5%). In telangiectasia, the linear (60%), polygonal (30%), Y-shaped (25%), and serpentine (15%) types were seen. The other findings observed were white, structureless areas (37.5%), Demodex tails (25%), scaling (15%), pustules (10%), comedones (20%), and the breaking of the pseudo-reticular network (22.5%).
Limitations: The limitation of this study was the lack of histopathological correlation.
Conclusion: Dermoscopy aids in the early diagnosis of TSDF.
Key words: Dermoscope; Corticosteroid; Face; Telangiectasia; Hyperpigmentation
INTRODUCTION
The first topical corticosteroid (TC) was introduced by Sulzberger and Witten in the year 1952 as “Compound F” (hydrocortisone) [1]. Since then, a number of steroid molecules with varying potencies have been available on the market.
TCs have anti-inflammatory, antiproliferative, immunosuppressive, antipruritic, atrophogenic, melanopenic, and sex hormone-like effects on the skin, so they are useful for hyperproliferative, inflammatory, and immunologic disorders [2].
Due to their wide action and easy availability, TCs have been misused by pharmacists, general doctors, and patients. Yet, the other side of steroids remains largely unknown. They are rosacea acneiform eruption, hypertrichosis, demodicosis [3], red face syndrome [4], and addiction [5]. These effects occur due to the combined effects of the inhibition of action of nitric oxide and local immunosuppression leading to the overgrowth of microbes.
Topical steroid-damaged face is a relatively new entity, described in 2008. It is defined as “semi-permanent or permanent damage to face precipitated by indiscriminate, unsupervised, irrational or prolonged use of TCs resulting in a plethora of cutaneous signs and symptoms and psychological dependence on the drug” [6].
The face is commonly affected in TSDF as it is the most accessible site, and the facial epidermis (0.12 mm) is comparatively thinner than the rest of the body (0.60 mm), which results in increased percutaneous absorption of drugs [7].
Dermoscopy may help in the early detection of subclinical changes caused by topical steroid use and, thereby, tailor the treatment specific to every patient. The dermoscopic features searched for in TSDF are telangiectasia, white areas (atrophy), erythema, scales, and hypertrichosis [8].
The aim of this study was to evaluate the pattern of topical steroid abuse among patients attending the dermatology OPD, to characterize the clinical and dermoscopic findings in patients with TSDF and, to correlate them with the duration of steroid use.
There are very few studies conducted in relation to the dermoscopic features of TSDF, thus we decided to undertake this study.
MATERIALS AND METHODS
This was a cross-sectional, observational study conducted on patients above 18 years of age with clinical features suggestive of TSDF and H/O use of topical steroids for more than thirty days in the past three months. The study ran for a period of six months from March 2021 to August 2021.
The exclusion criteria were patients with pre-existing comorbidities (Cushing syndrome, PCOS, and thyroid disease), pregnant patients, patients under treatment with oral steroids, and patients unwilling to give consent.
Informed consent was taken from all patients. The sample size was 80. After detailed history taking regarding the nature of the steroid used, source, duration, and indication, clinical examination and dermoscopic evaluation were performed for all patients. Clinical and dermoscopic pictures were captured with an iPhone. Dermoscopy was performed by DermLite DL4. Statistical analysis was done with SPSS, version 22. Categorical variables were presented as frequencies and percentages. Quantitative variables were presented as means and SDs. Qualitative variables were compared with the chi-squared test. Ethical committee clearance was obtained.
RESULTS
A total of 80 patients were included in the study, among which 64 (80%) were females and 16 (20%) were males. The most common age group affected was 18–30 years (52; 65%). Sixty-six patients (82.5%) were literate and received basic education, while fourteen (17%) were illiterate. Melasma (44; 55%) was the common underlying condition for which steroids were applied (Table 1). Betamethasone (34; 47.5%) was the most commonly used by the patients, followed by clobetasol (22.5%). They were mostly used in combination with other creams, such as antifungal, antibacterial, and depigmenting creams. The cream formulation was used by most patients (90%) compared to ointments and lotions. The most common source of recommendation for the use of a topical steroid was relatives and friends (46; 57.5%) (Table 1). Most of the patients applied TCs for one year. The duration ranged from two months to twelve years. Eighty percent of the patients employed topical steroids continuously, whereas only a small number of the patients (10%) employed them intermittently over a period of twelve years.
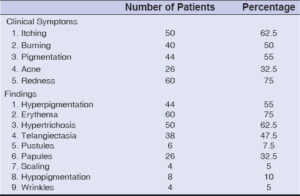
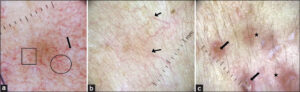
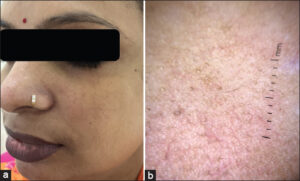
Redness was the predominant presenting complaint (60; 75%), followed by itching (50; 62.5%). Most patients had more than one clinical finding or side effect induced by steroids. The common clinical findings observed were erythema (75%), hyperpigmentation (44; 55%), hypertrichosis (50; 62.5%), acneiform eruption (26; 32.5%), telangiectasia (47.7%), and atrophy (4,5%) (Table 2) (Figs. 1a and 1b).
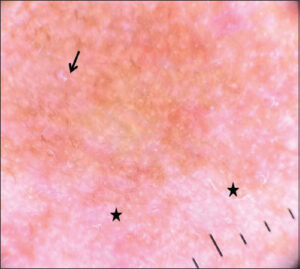
On dermoscopy, the most common findings observed were telangiectasia or vessels (90%), red, diffuse areas (75%), brown globules (55%), and hypertrichosis (62.5%). Telangiectasia and vessels were observed in the following patterns: linear vessels without branches (60%), polygonal vessels with multiple branches (30%), Y-shaped vessels with bifurcations (25%), and serpentine vessels (15%) (Figs. 2 and 3). The other features noted were white, structureless areas (37.5%), Demodex tails (25%) (Fig. 4), scaling (15%), pustules (10%), comedones (20%), and the breaking of the pseudo-reticular network (22.5%) (Table 3). Erythema, polygonal vessels, and white, structureless areas were seen more frequently in patients with long-standing use of topical steroids (Fig. 5). Brown globules were mostly observed in patients with a background of hyperpigmentation, such as melasma.
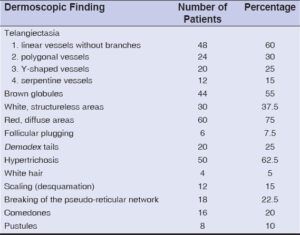 |
Table 3: Dermoscopic findings. |
DISCUSSION
TSDF is caused by patients and laymen applying TCs of the wrong potency to the face for a wrong indication and at the wrong age [2].
Topical steroid abuse is of great concern not only in India yet also in countries such as Africa, Iraq, and China [9–11].
The most common age group in our study was 18–30 years, which was in concordance with other studies [2,12,13]. At this age, social interactions and peer influence are more important. Yet, an Iraqi study found an age group of 15–19 years, which was a significantly younger population [9].
Abuse of steroids was more frequent in females in our study, similarly to other studies [11,12,14,15]. The reason could be cultural, ethnic, and social factors. In our study, 82.5% of the patients were literate, disproving the fact that steroid abuse is common among illiterates. This was also observed in other Indian studies [15].
Most of the patients employed TCs for more than one year, mostly due to feel-good effects and steroid addiction. The most common sources of recommendation were relatives and friends, followed by pharmacies, similarly to other studies [10,15]. This showed the unregulated OTC prescriptions common in India.
Betamethasone was commonly employed in our study and mostly in combination, as the Indian market is flooded with several combinations of steroids with antibacterial and antifungal agents. They are also cheaper. This finding was also observed in a multicentric study by Saraswat et al. and other studies [2,16].
TCs are mostly marketed as fairness creams, anti-acne medications, and general-purpose creams. In our study, most patients used TCs for melasma and fairness.
According to the literature, the common clinical findings observed in patients with TSDF are erythema, dyspigmentation, and papulopustular lesions [11,12,14]. Hypertrichosis and atrophy were also observed in addition to the above findings. Most of the patients presenting with erythema may have been due to rebound vasodilation.
Some studies have documented the dermoscopic findings of TSDF. According to Sethi et al., the most common dermoscopy findings were brown globules (96.2%), red, diffuse areas (92.4%), vessels (87.1%), white, structureless areas (86.4%), hypertrichosis (80.3%), and white hairs (62.1%) [15]. Meanwhile, in a study on forty patients by Tatu, the dermoscopy findings observed were polygonal vessels (100%), red, diffuse areas (100%), Demodex tails (80%), and pustules (80%) [8]. In our study, we observed vessels and telangiectasia (90%), red, diffuse areas (75%), brown globules (55%), and hypertrichosis (62.5%). Sethi et al. observed brown globules predominantly in their study along with red, diffuse areas [15], while brown globules were not predominant in our study. Vessels were common in our study, similarly to a study by Tatu et al., in which 100% of the cases had polygonal vessels [8].
Sonthalia et al., in a case report on TSDF, observed brown dots on a reddish-brown background, globules, clods, and ivory white to pinkish patches, multiple serpentine and branching linear vessels without branches with hypertrichosis [17]. In another case report, Jakhar and Kaur observed irregular, dilated, branched, serpentine vessels almost interconnecting, creating a polygonal pattern along with white, structureless areas and hypertrichosis [18]. In our study, we also observed various types of vasculature, linear, polygonal, Y-shaped, and serpentine vessels. Linear vessels without branches were the most common in our study. Polygonal vessels were seen in patients with long-standing use of steroids. Sethi et al. also observed Y-shaped vessels in patients using TCs for more than three months and polygonal vessels in patients using TCs for more than six months [15].
We observed Demodex tails in some cases, as Demodex infestation is common following the use of topical steroids.
In our study, predominant brown globules were seen more frequently in patients using TCs for melasma. As per the literature, dermoscopy of melasma shows a diffuse, light to dark brown background, brown granules, and globules with arcuate and annular structures.
Dermoscope is a valuable tool in the early diagnosis of damage caused by the use of topical steroids. When shown dermoscopic pictures, patients become more aware and vigilant on topical steroid use and adhere to future treatment.
If the patient is not giving a history suggestive of topical steroid use, a dermoscope may detect the changes and we may prompt the patient accordingly.
This study highlights the importance of awareness of the adverse effects of topical steroids and their addiction among doctors and patients. As these side effects are quite serious, early detection is essential. OTC sales of TCs should be banned in India, and the public should be highly educated about the topic.
Study Limitations
The limitation of this study was the lack of histopathological correlation.
CONCLUSION
Dermoscope is highly recommended as a non-invasive tool for the diagnosis of TSDF.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19:101-2.
2. Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face:A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
3. Basta-JuzbasićA, SubićJS, LjubojevićS. Demodex folliculorum in development of dermatitis rosaceiformis steroidica and rosacea-related diseases. Clin Dermatol. 2002;20:135-40.
4. Rapaport MJ, Rapaport V. Eyelid dermatitis to red face syndrome to cure:Clinical experience in 100 cases. J Am Acad Dermatol. 1999;41:435-42.
5. Kligman AM, Frosch PJ. Steroid addiction. Int J Dermatol. 1979;18:23-31.
6. Lahiri K, Coondoo A. Topical steroid damaged/dependent face (TSDF):An entity of cutaneous pharmacodependence. Indian J Dermatol. 2016;61:265-72.
7. Souza, Aieska De, and Bruce E. Strober. “Chapter 214, Pg No.2643-68. Principles of Topical Therapy.“Fitzpatrick›s Dermatology in General Medicine, 8eEds. Lowell A. Goldsmith, et al. McGraw Hill,2012.
8. Tatu AL. Topical steroid-induced facial rosaceiform dermatitis. Acta Endocrinol (Buchar). 2016;12:232-3.
9. Al-Dhalimi MA, Aljawahiry N. Misuse of topical corticosteroids:A clinical study in an Iraqi hospital. East Mediterr Health J. 2006;12:847-82.
10. Lu H, Xiao T, Lu B, Dong D, Yu D, Wei H, et al. Facial corticosteroid addictive dermatitis in Guiyang City, China. Clin Exp Dermatol. 2010;35:618-21.
11. Nagesh TS, Akhilesh A. Topical steroid awareness and abuse:A prospective study among dermatology outpatients. Indian J Dermatol. 2016;61:618-21.
12. Hameed AF. Steroid dermatitis resembling rosacea:A clinical evaluation of 75 patients. ISRN Dermatol. 2013;2013:491376.
13. Inakanti Y, Thimmasarthi VN, Anupama, Kumar S, Nagaraj A, Peddireddy S, et al. Topical corticosteroids:Abuse and misuse. Our Dermatol Online. 2015;6:130-4.
14. Jain S, Mohapatra L, Mohanty P, Jena S, Behera B. Study of clinical profile of patients presenting with topical steroid induced facial dermatosis to a tertiary care hospital. Indian Dermatol Online J. 2020;11:208-11.
15. Sethi S, Chauhan P, Jindal R, Bisht YS. Dermoscopy of topical steroid dependent or damaged face:A cross-sectional study. Indian J Dermatol Venereal Leprosy 2022;88;40-6.
16. Ravindran S, Prabhu S, Nayak SUK. Topical steroid damaged skin:A clinico-epidemiological and dermatological study. J Pak Assoc Dermatol. 2021;31:407-14.
17. Sonthalia S, Jha AK, Sharma R. The role of dermoscopy in a topical steroid-damaged face. Dermatol Pract Concept. 2018;8:166-7.
18. Jakhar D, Kaur I. Dermoscopy of topical steroid damaged/dependent face.Indian Dermatol Online J. 2018;9:286-7.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-5686-0902 http://orcid.org/0000-0002-5686-0902 http://orcid.org/0000-0000-9590-2100 http://orcid.org/0000-0000-9590-2100 http://orcid.org/0000-0009-4904-9476 http://orcid.org/0000-0009-4904-9476 |







Comments are closed.