Sulfasalazine-induced lichen planus in a patient with ulcerative colitis
Toshiyuki Yamamoto
Department of Dermatology, Fukushima Medical University, Fukushima, Japan
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
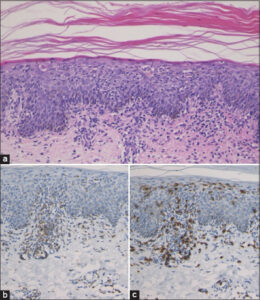
A 76-year-old female with ulcerative colitis was treated with sulfasalazine. Six years after the initiation of sulfasalazine, she developed a pruritic eruption and was referred to our department. A physical examination revealed small, round, brownish, erythematous plaques with scales on the trunk and extremities. Small, scaly erythemas and plaques were distributed on and around old surgical scars due to osteomyelitis (Fig. 1). Neither mucosal nor nail lesions were observed. A laboratory examination revealed normal blood cell counts with a normal eosinophil percentage, as well as normal liver and kidney function. Antinuclear antibody was positive (1:320, homogenous and speckled), yet ani-HCV antibody, anti-thyroglobulin antibody, anti-microsome antibody, anti-SS-A antibody, and anti-SS-B antibody were negative or within normal ranges. The drug transformation test with sulfasalazine was negative. A histopathological examination revealed mild acanthosis of the epidermis, individual cell keratinization of the epidermal cells, vacuolar degeneration in the basement membrane, and infiltration of mononuclear cells in the epidermis and upper dermis (Fig. 2a). Immunohistochemistry revealed that the infiltrating mononuclear cells were positive for both CD4 and CD8 (Figs. 2b and 2c). The cutaneous lesions completely disappeared with the use of topical corticosteroid ointment and the discontinuance of sulfasalazine after two years (Fig. 3).
The patient developed lichenoid eruptions on the trunk and extremities, with a unique distribution of the keratotic erythemas on and around old surgical scars, which was considered a physical trauma of Köbner phenomenon [1]. The discontinuation of sulfasalazine and topical corticosteroid therapy resulted in the complete disappearance of cutaneous eruptions, thus we diagnosed the case as sulfasalazine-induced lichen planus.
Sulfasalazine has immunosuppressive, immunomodulatory, and anti-inflammatory effects and is commonly used in the treatment of rheumatoid arthritis and ulcerative colitis [2]. In the dermatological field, sulfasalazine is occasionally employed off-label for numerous autoimmune and inflammatory disorders [2]. Previous studies have shown the efficacy of sulfasalazine in the treatment of generalized lichen planus in a randomized double-blind clinical trial. A group on oral sulfasalazine (initial dose of 1 g/day, increasing 0.5 g every three days up to 2.5 g/day) showed a greater clinical improvement (80.7%) when compared to a placebo group (7.6%) [3].
After six weeks, the group treated with sulfasalazine showed an improvement at 82.6%, whereas an improvement was observed in 9.6% of the placebo patients. Although not in a placebo-controlled trial, sulfasalazine resulted in a complete resolution (n = 13) or partial response (n = 7) in twenty patients with cutaneous lichen planus. Although the mechanism is unknown, it is speculated to be caused by the inhibition of the expression of several cytokines and adhesion molecules by sulfasalazine [4]. Although sulfasalazine is a possible therapeutic candidate for refractory lichen planus, reports of sulfasalazine-induced lichen planus are rare. In previous reports, lichen planus have been induced during sulfasalazine treatment in patients with rheumatoid arthritis [5,6]. Concurrent lichen planus and ulcerative colitis have rarely been observed [7]. However, to our knowledge, this is the first case of sulfasalazine-induced lichen planus in a patient with ulcerative colitis.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Zhang X, Lei L, Jiang L, et al. Characteristics and pathogenesis of Koebner phenomenon. Exp Dermatol. 2023;32:310-23.
2. Mushtaq S, Sarkar R. Sulfasalazine in dermatology:A lesser explored drug with broad therapeutic potential. Int J Womens Dermatol 2020;6:191-8.
3. Omidian M, Ayoobi A, Mapar MA, et al. Efficacy of sulfasalazine in the treatment of generalized lichen planus:Randomized double-blinded clinical trial on 52 patients. J Eur Acad Dermatol Venereol. 2010;24:1051-4.
4. BauzáA, España A, Gil P, et al. Successful treatment of lichen planus with sulfasalazine in 20 patients. Int J Dermatol. 2005;44:158-62.
5. Kaplan S, McDonald E, Marino C. Lichen planus in patients with rheumatoid arthritis treated with sulfasalazine. J Rheumatol. 1995;22:191-2.
6. Ghosh S, Jain VK, Chaudhuri S, Mathur SK. Sulfasalazine induced lichen planus in a patient of rheumatoid arthritis. Indian J Dermatol Venereol Leprol. 2013;79:541-4.
7. Dhawan SS, Fields K. Lichen planus and ulcerative colitis:Is there a relationship?Int J Dermatol. 1989;28:534.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-8390-2573 http://orcid.org/0000-0002-8390-2573 |






Comments are closed.