Multiple non-familial trichoepitheliomas: A rare case and a review of the literature
Fatima Amaaoune 1, Wassima Zidane2, Mohamed Aksim3, Maryem Aboudourib1, Ouafa Hocar1, Said Amal1
1, Wassima Zidane2, Mohamed Aksim3, Maryem Aboudourib1, Ouafa Hocar1, Said Amal1
1Department of Dermatology-Venerology, CHU Med VI, Marrakech – Laboratory of Bioscience and Health-FMPM-University Quadi Ayyad, Marrakech, Morocco, 2Department of Dermatology, Hassan II Regional Hospital Center, Agadir, Morocco, 3Anatomopathology Laboratory, Hassan II Regional Hospital Center, Agadir, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Trichoepitheliomas are benign tumors of follicular origin often appearing in childhood or early adolescence. They present as small, firm papulonodular lesions of normal skin color or translucent. The lesions gradually increase in size and then stabilize. They sit electively on the face, mainly on the nasolabial folds, forehead, chin, and cheeks, and sometimes on the scalp and neck. Trichoepitheliomas may be divided into three subgroups: multiple familial trichoepitheliomas, solitary non-hereditary trichoepitheliomas, and desmoplastic trichoepitheliomas. Non-familial multiple trichoepitheliomas are rarely described. Herein, we report the case of a twelve-year-old child whose clinical history and clinicopathologic correlation allowed us to retain the diagnosis of multiple non-familial trichoepitheliomas.
Key words: Trichoepitheliomas; Sporadic; Genodermatosis; Cyld Gene; Anatomopathology
INTRODUCTION
Trichoepitheliomas (TE) are benign tumors of follicular origin. They were first described by Brooke in England in 1892 as “cystic adenoid epithelioma” and, in the U.S., by Fordyce as “multiple benign cystic epithelioma” [1,2]. These are papules, measuring several millimeters, mainly located on the face, scalp, and neck, appearing in childhood and increasing in number with age. They may be isolated or multiple and occur sporadically or in families [3]. Although rare, the malignant transformation of TE into trichoblastic carcinoma or basal cell carcinoma has been described [4]. Herein, we report a case of multiple non-familial TE in a twelve-year-old child.
CASE REPORT
This was a twelve-year-old male child, with no particular pathological history and no notion of consanguinity, who presented with asymptomatic skin lesions on the face evolving for the previous one year, gradually increasing in size and number, without any similar case in the family or other associated cutaneous and extra-cutaneous signs.
A general examination found a patient who was hemodynamically and respiratory stable. A dermatological examination revealed translucent, flattened, and globular papules, 2 to 4 mm in size, pink, fleshy, and painless, sitting on healthy skin, electively on the face (nose, nasolabial folds, eyelids, cheeks, forehead, and chin) (Figs 1a and 1b). The rest of the dermatological and somatic examinations was unremarkable.
 |
Figure 1: (a-b) Translucent, flattened, globular papules, 2 to 4 mm, pink and fleshy, located on the healthy skin of the face. |
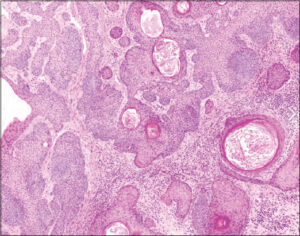
A histopathological study of the papules confirmed the diagnosis of TE by showing a well-limited, benign tumoral proliferation localized in the reticular dermis, comprising lobules and islands of basaloid cells arranged in anastomosed spans and developing around horny cysts (Fig. 2). The diagnosis of multiple non-familial TE was retained, given the absence of similar cases in the family and the clinical and histological aspects. We offered CO2 laser with regular clinical monitoring, having informed the parents about the risk of malignant transformation of the disease.
DISCUSSION
Trichoepitheliomas are benign hamartomas of pilosebaceous follicles often appearing in childhood or early adolescence [5]. The various synonyms of TE are trichoepithelioma papulosum multiplex, cystic adenoid epithelioma, cystic adenoid acanthoma, multiple benign cystic epithelioma, Brooke’s tumor, and Brooke Fordyce’s trichoepithelioma [6]. Clinically, TE presents as small, firm, papulonodular lesions of normal or translucent color, sometimes covered with telangiectasias. The lesions gradually increase in size and then stabilize. They sit electively on the face, mainly on the nasolabial folds, forehead, chin, and cheeks, and sometimes on the scalp and neck [7]. Their prevalence is unknown. However, a dermatopathology laboratory in the U.S. found 2.14 to 2.75 cases of TE out of 9,000 biopsies per year [8].
TE may be divided into three subgroups: multiple familial TE, solitary non-hereditary TE, and desmoplastic TE. Non-familial multiple TE is rarely described, Sehrawat et al. published the first case in 2016 [9]. Our case had multiple TEs with no similar family history.
Multiple familial trichoepitheliomas (MFT) is an autosomal dominant hereditary genodermatosis associated with mutations in chromosome 9p21 or the cylindromatosis (CYLD) tumor suppressor gene, located on chromosome 16q12-113 [10,11]. The CYLD gene encodes a protein of 956 amino acids with a molecular weight of 120 kDa belonging to the family of deubiquitinases. In the normal state, the CYLD protein acts primarily as an inhibitor of nuclear factor B in the TNF signaling pathway. In the majority of cases, the mutations lead to the formation of an abnormal truncated protein, leading to an increase in NF-kB activity induced by TNF and a defect in apoptosis at the origin of tumor proliferation [12,13]. MFT may be seen in Brooke–Spiegler syndrome, in which inherited adnexal tumors are combined, including multiple trichoepitheliomas, cylindromas, and spiradenomas [5]. Moreover, it may also be seen in other syndromes, such as Rombo syndrome (vermicular atrophoderma, milia, trichoepithelioma, hypotrichosis, basal cell carcinomas, and hypohidrosis) and Bazex syndrome (follicular atrophoderma, trichoepithelioma, hypotrichosis, basal cell carcinomas, and hypohidrosis) [14]. MFT has also been found to be associated with multiple renal and pulmonary cysts, basal cell adenoma of the parotid gland, ovarian cancer, breast cancer, steatocystomas, alopecia, and myasthenia gravis [15].
The differential diagnosis of TE includes the juvenile colloid milium, cylindroma, syringoma, milium, eccrine poroma, eccrine nevus, nevus comedonicus, multiple trichoblastoma, sebaceous adenoma, trichofolliculoma, basal cell carcinoma, and molluscum contagiosum [14]. A histological examination of TE confirms the diagnosis. It shows a well-defined lesion comprising epithelial bands and small cords of basophilic cells, often centered or terminated by horny cysts forming the characteristic “tadpole tail” appearance. The basaloid cells may assume a palisade arrangement around the periphery of the lobules and islets. The perilesional stroma is dense and fibrous [16].
Multiple non-familial TE is rare and the diagnosis is usually reached by clinicopathologic correlation in the absence of a family history of similar cases and, if necessary, a genetic study. Our original case was the fourth case of multiple non-familial TE reported in the literature. For the three other cases, one presented multiple, non-segmental, unilateral, grouped papules on the trunk [8], one had extensive and disfiguring TE on the face [9], and one had multiple segmental TE along Blaschko lines on the right shoulder [17].
The evolution of non-familial multiple TE is marked by the multiplication of lesions. The damage is essentially aesthetic, as was the case of our patient. However, rare cases of associated malignant tumors have been described (basal cell carcinoma, trichoblastic carcinoma), justifying regular monitoring [18,19].
Therapeutic methods are based on surgical excision or destructive methods (cryotherapy, electrocoagulation, CO2 laser, or Er: YAG laser), yet the latter does not prevent the occurrence of new lesions [20,21].
Topical sirolimus at 1%, imiquimod at 5%, and tretinoin at 1% are also used. In an eleven-year-old girl with multiple TEs, the application of imiquimod initially alone, then in combination with tretinoin, resulted in an 80% improvement in the lesions after three years [22,23].
A better knowledge of the pathophysiological mechanisms of the CYLD protein, in particular, concerning its inhibitory activity on nuclear factor B induced by TNF may lead to the consideration of other therapeutic alternatives, such as NF-B antagonists (aspirin or non-steroidal anti-inflammatory drugs) and anti-TNF (adalimumab). Yet, as the lesions are asymptomatic and have an extremely low malignant potential, treatment is usually not necessary unless there is disfigurement [7,24].
CONCLUSION
Herein, we have reported a rare case of sporadic multiple TE with no family history. To our knowledge, our case represented the fourth case described to date in the literature.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Brooke HG. Epithelioma adenoidscysticum. Br J Dermatol. 1892;4:269-87.
2. Fordyce JA. Multiple benign cystic epitheliomas of the skin. J Cutan Dis. 1892;10:459-73.
3. Miotto IZ, Romiti R. Nonfamilial multiple trichoepithelioma. JAMA Dermatol. 2019;155:1070.
4. Lee KH, Kim JE, Cho BK, Kim YC, Parq CJ. Malignant transformation of multiple familial trichoepithelioma:Case report and literature review. Acta Derm Venerol. 2008;88;43-6.
5. Karimzadeh I, Namazi MR, Karimzadeh A. Trichoepithelioma:Une revue complète. Acta Dermatovenerol Croat. 2018;26:162-5.
6. Kataria U, Agarwal D, Chhillar D. Familial facial disfigurement in multiple familial trichoepithelioma. J Clin Diagn Res. 2013;7:3008-9.
7. Duparc A, Lasek-Duriez A, Wiart T, Duban-Bedu B, Gosset P, Modiano P. [Multiple familial trichoepithelioma:A new CYLD gene mutation]. Ann Dermatol Venereol. 2013;140:274-7.
8. Vy M, Mehrzad M. An unusual case of multiple grouped non-familial trichoepitheliomas, Dermatol Online J. 2021;27:8.
9. Sehrawat M, Jairath V, Jain VK. Nonfamilial multiple trichoepithelioma:Few and far between. Indian J Dermatol. 2016;61:78-80.
10. Bignell GR, Warren W, Seal S, Takahashi M, Rapley E, Barfoot R. Identification of the familial cylindromatosis tumoursuppressor gene. Nat Genet. 2000;2:160-5.
11. Zhang XJ, Liang YH, He PP, Yang S, Wang HY, Chen JJ. Identification of the cylindromatosis tumor-suppressor gene responsible for multiple familial trichoepitheliomas. J Invest Dermatol. 2004;122:658-64.
12. Brummelkamp TR, Nijman SM, Dirac AM, Bernards R. Loss of the cylindromatosis tumor suppressor inhibits apoptosis by activating NF-kappaB. Nature. 2013;424:797-801.
13. Bonnet M, Courtois G. CYLD deubiquitinase as a recurrent target in oncogenic processes. Med Sci (Paris). 2011;27:626-31.
14. Gupta M, Sharma RK, Rao M. Multiple non-familial trichoepitheliomas in a naine wear old Child. Nepal J Dermatol. 2019;17:76-8.
15. Centurion SA, Schwartz RA, Lambert WC. Trichoepithelioma papulosum multiplex. J Dermatol. 2000;27:137-43.
16. Clarke J, Ioffreda M, Helm KF. Multiple familial trichoepitheliomas. Am J Dermatopathol. 2002;24:402-5.
17. Parren LJ, Munte K, Winnepenninckx V. Les trichoépithéliomes unilatéraux groupés indiquent une manifestation segmentaire de type 1 du trichoépithéliome familial multiple. Clin Exp Dermatol. 2016;41:682-4.
18. Tsalamlal A, Bourillon C, Kannengiesser A, Riffault C, Moreno F, Aubin. Étude clinique et moléculaire de patients atteints de cylindromatose. Ann Dermatol Venereol. 2011;138:A78.
19. Pincus LB, McCalmont TH, Neuhaus IM, Kasper R, Oh DH. Basal cell carcinomas arising within multiple trichoepitheliomas. J Cutan Pathol. 2008;35:59-64.
20. Rallan D, Harland CC. Brooke–Spiegler syndrome:Treatment with laser ablation. Clin Exp Dermatol. 2005;30:355-7.
21. LoPiccolo MC, Sage RJ, Kouba DJ. Comparing ablative fractionated resurfacing, photodynamic therapy, and topical imiquimod in the treatment of trichoblastomas of Brooke–Spiegler Syndrome:A case study. Dermatol Surg. 2011;37:1047-50.
22. Urquhart JL, Weston WL. Treatment of multiple trichoepitheliomas with topical imiquimod and tretinoin. Pediatr Dermatol. 2005;22:67-70.
23. Alessi SS, Sanches JA, Oliveira WR, Messina MC, Pimentel ER, Festa Neto C. Treatment of cutaneous tumors with topical 5% imiquimod cream. Clinics (Sao Paulo). 2009;64:961-6.
24. Malakar S, Mukherjee SS. Dermoscopic description of trichoepithelioma in the skin of color. Our Dermatol Online. 2018;9:335-6.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-0670-2540 http://orcid.org/0000-0003-0670-2540 |




Comments are closed.