Comedonal variant of chronic cutaneous lupus erythematosus on the nose
Chaimae Ait Khabba 1, Basma Karrakchou1, Marwa Asermouh1, Laila Berbich1, Kaoutar Znati2, Karima Senouci1
1, Basma Karrakchou1, Marwa Asermouh1, Laila Berbich1, Kaoutar Znati2, Karima Senouci1
1Department of Dermatology and Venereology, Ibn Sina Hospital, Mohammed V University, Rabat, Morocco, 2 Department of Anatomo-Pathology, Ibn Sina Hospital, Mohammed V University, Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
A thirty-year-old patient presented with an erythematous papule on the left nostril evolving for ten months. A clinical examination revealed an infiltrated, erythematous, well-limited plaque with a raised border, covered with multiple open and closed comedones. On dermoscopy, there was an erythematous background with some fine telangiectasias and horny plugs at the follicular orifices. A skin biopsy was performed, revealing orthokeratotic hyperkeratosis sinking into the follicular orifices dilated by sebum clumps with basal vacuolation associated with a subepidermal and periadnexal/perivascular lymphocyte band infiltrate. Direct immunofluorescence staining for immunoglobulin M was positive. The diagnosis of lupus comedones was retained, and the patient was put on topical tacrolimus 0.1% twice a day. A systemic damage assessment was negative. Our case highlighted, the importance of recognizing this rare variant of cutaneous lupus, confused with acne vulgaris, hence the delayed diagnosis, which may also be an early sign of a concomitant systemic involvement.
Key words: Acne; Chronic Cutaneous Lupus Erythematosus; Comedonal Variant; Discoid Lupus Erythematosus
INTRODUCTION
Chronic cutaneous lupus erythematosus most commonly presents as a discoid form consisting of scaly, erythematous plaques covered with fine telangiectasias surrounding central atrophy. Comedonal lupus is an extremely rare variant of chronic cutaneous lupus with a misleading acneiform appearance. Herein, we report a rare case of comedonal lupus on the left nostril and present its characteristics.
CASE REPORT
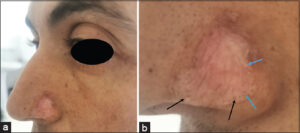
A thirty-year-old patient with no medical history presented with a firm, erythematous papule on the left nostril evolving for ten months, progressively increasing in size.
A clinical examination revealed an infiltrated erythematous plaque, 1 cm in diameter, well-limited with a raised border, and covered with multiple open and closed comedones, especially on the periphery (Figs. 1a and 1b). On dermoscopy, there was an erythematous background with some fine telangiectasias and horny plugs at the follicular orifices.
A skin biopsy with an anatomo-pathological examination was performed, finding orthokeratotic hyperkeratosis sinking into the follicular orifices dilated by sebum clumps. There was also vacuolation of the basement membrane with significant lymphocyte infiltrate in subepidermal and periadnexal/perivascular bands (Fig. 2). The dermis was the seat of discrete deposits of mucin of Alcian blue color. Direct immunofluorescence staining for immunoglobulin M was positive.
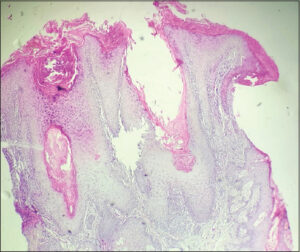 |
Figure 2: Large follicular openings dilated by clumps of sebum, interface dermatitis, and dermal mucinosis (H&E). |
The diagnosis of lupus comedonal was retained, and the patient was put on topical tacrolimus 0.1% twice a day combined with rigorous photoprotection. A systemic damage assessment was negative.
DISCUSSION
Comedonal lupus is a rare and, probably, an underestimated variant of chronic cutaneous lupus erythematosus. Clinically, it appears in the form of comedones on an erythematous plaque, mainly in seborrheic areas [1]. Its etiology remains unknown. Actinic lesions allow modifications of the collagen of normal skin, which modifies its structure and, thus, promotes the retention of sebum. This leads to the training of actors, as in Favre–Racouchot disease. The other postulated theory is that follicular plugging promotes comedogenesis [2].
Dermoscopy may be of great help in revealing black openings in pseudo-comedones and images of pseudo-grains of milium testifying to the folliculotropic character.
The differential diagnosis is inflammatory acne, milium spots, Favre–Racouchot disease, and comedonal hamartoma [3]. If there are no comedones, there is an acneiform scar pattern. In this entity, the lesions are characterized by the presence of ice-pick scars secondary to the destruction of the hair follicle and the sebaceous glands by the inflammatory infiltrate [4].
A histopathological study confirms the diagnosis and finds predominant interface dermatitis with the degeneration of the basal layer and thickening of the basal membrane, associated with follicular plugs and comedones, as described in our patient. Direct immunofluorescence may aid in the diagnosis if the histological results are inconclusive, in which a deposition of IgM, IgG, and C3 is observed at the dermal–epidermal junction [2,5].
The therapeutic options vary, although the treatment of choice is hydroxychloroquine (200 mg twice a day). In our case, it was not administered in front of a single small lesion. As an alternative, a topical corticosteroid or topical tacrolimus is offered [6].
The prognosis of comedonal lupus is uncertain and, although few cases have been described in the literature, a risk of progression to SLE was observed in four of them [7]. Early diagnosis and long-term follow-up are of great importance because of the risk of progression to systemic involvement.
CONCLUSION
This clinical case illustrates the need to broaden the differential diagnosis of atypical acneiform and comedonal lesions. Lupus comedones should be considered especially in an itchy, localized lesion that does not improve with conventional treatment for acne vulgaris and should be investigated for systemic involvement.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Hammami F, Bahloul E, Masmoudi A, Boudaya S, Mseddi M, Amouri, et al. Le lupus comédonien:Particularités cliniques et dermoscopiques. Ann Dermatol et Venerol. 2019;146:12-217.
2. Droesch C, Magro C. A comedonal variant of chronic cutaneous lupus erythematosus:Case report and literature review. JAAD Case Rep. 2019;29:801-5.
3. El Sayed F, Dhaybi R, Ammoury A, Bazex J. [Lupus comedonicus]. Ann Dermatol Venereol. 2007;134:897-8.
4. Chang YH, Wang SH, Chi CC. Discoid lupus erythematosus presenting as acneiform pitting scars. Int J Dermatol. 2006;45:944-5.
5. El Gaitibi FA, Belcadi J, Ali SO, Znati K, Senouci K, Ismaili N. Comedonal plaque on the scalp. JAAD Case Rep. 2021;11:90-2.
6. Frioui R, Mokni S, Jouini W, Tabka M, Fajji Y, Sriha B, et al. Comedonal lupus on the scalp:a case report. Scand J Rheumatol. 2022;51:333-5.
7. Cozzani E, Herzum A, Burlando M, Parodi A. Comedonal variant of chronic cutaneous lupus erythematosus causing mutilation of the earlobe. JAAD Case Rep. 2020;6:843-4.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0001-1343-4188 http://orcid.org/0009-0001-1343-4188 http://orcid.org/0000-0002-5204-0528 http://orcid.org/0000-0002-5204-0528 |




Comments are closed.