Bullous pemphigoid secondary to an orf nodule: A still unrecognized complication
Zineb Zeggwagh , Sara Kerroum, Nadia Ismaili, Laila Benzekri, Mariame Meziane, Karima Senouci
, Sara Kerroum, Nadia Ismaili, Laila Benzekri, Mariame Meziane, Karima Senouci
Department of Dermatology and venerology, University Hospital Center Ibn Sina, University Mohamed V, Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Orf is a rare viral zoonosis due to Parapoxvirus infection. Transmission to humans occurs through contact with infected goats and sheep. It may be complicated by fever, lymphangitis, lymphadenopathy, bacterial infection, and erythema multiforme. Only several cases of autoimmune bullous dermatoses have been described. Bullous pemphigoid secondary to an orf was found in ten patients. Herein, we report one case of a human orf complicated by bullous pemphigoid. This is an occasional complication following an orf. Knowledge of co-occurrence allows for the better management of the affected patient. This case is reported for its rare association.
Key words: Bullous Pemphigoid; Orf; Orf-Induced Immunobullous Disease
INTRODUCTION
An orf nodule is a rare viral zoonosis caused by Parapoxvirus infection. Human transmission may occur by contact with sheep or goats themselves suffering from contagious ecthyma. Diagnosis is often clinical and manifests as a single or multiple lesions on a finger or hand.
Several complications may occur following an orf: fever, lymphangitis, lymphadenopathy, and bacterial infection [1]. Post-orf autoimmune bullous dermatoses are much rarer, with only eleven cases reported in the literature: ten cases of bullous pemphigoid and one case of pemphigoid with mucosal involvement and the presence of anti-laminin-332 antibodies [2]. We describe the eleventh case of bullous pemphigoid secondary to an orf, which is considered a highly rare complication.
CASE REPORT
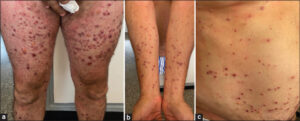
A 56-year-old Moroccan male with a history of type 2 diabetes, on metformin for two years, presented eight days after Eid al-Adha (a Muslim religious sacrifice) with a nodule on the right middle finger gradually increasing in size. In view of the lesion and the context of occurrence (handling of sheep during Eid al-Adha), the diagnosis was in favor of an orf. The patient received a topical antibiotic with a complete regression of the lesion in five weeks. Three weeks after the appearance of the orf nodule, he consulted for a diffuse, pruriginous, bullous eruption, initially located on the right arm, then generalizing to the trunk, abdomen, and all four limbs. A dermatological examination revealed an erythematous, ulcerated nodule, well-limited, firm, deeply infiltrated, measuring 2 cm in size, and located on the right middle finger (Fig. 1). Multiple tense blisters with a clear content on non-inflamed skin affecting the four limbs, abdomen, and back (Fig. 2a). Multiple erythematous papules were on the four limbs and abdomen (Fig. 2b). Some erosions were on the limbs and abdomen (Fig. 2c). The Nikolsky sign was negative.
He did not present any lesions on the mucous membranes or scalp. The rest of the examination was normal.
Dermoscopy of the nodule on the hand revealed an erythematous lesion with yellowish scales, especially on the periphery, red areas without a structure, glomerular vascularization on the periphery, and whitish structures (Fig. 3).
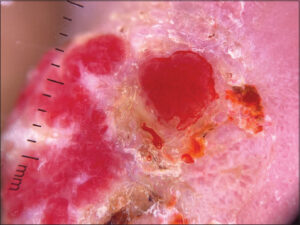 |
Figure 3: Dermoscopy of the orf nodule: an erythematous lesion with yellowish scales, red areas without a structure, and glomerular vascularization on the periphery. |
A skin biopsy revealed a subepidermal bulla with a mixed inflammatory infiltrate in the dermis. Direct immunofluorescence revealed a deposition of C3 linearly along the basal membrane. Indirect immunofluorescence revealed the presence of anti-basal membrane antibodies positive at 40. The rest of the biological assessment was unremarkable.
The diagnosis of pemphigoid complicating an orf nodule was retained. The patient received topical steroids (clobetasol propionate) for several weeks with a complete regression of the lesions three weeks later. He did not present any bullous eruptions after one year of follow-up.
DISCUSSION
Orf, or ecthyma contagiosum, is a zoonosis caused by a DNA virus from the Parapoxvirus family. It is a rare and often misunderstood pathology that affects sheep and goats. The population at risk includes shepherds, butchers, farmers, wool shearers, and veterinarians.
It is transmitted to humans through direct contact with infected animals, or indirectly through contaminated offal or knives, which was the mode of transmission in our patient. No human-to-human transmission of Parapoxvirus infection has been reported [3]. The most frequently observed complications are fever, lymphangitis, lymphadenopathy, and bacterial infection. Cases of erythema multiforme complicating an orf nodule have also been described in the literature, despite it being a highly rare complication [4,5].
Alian et al. reported a case of erythema multiforme associated with a pemphigoid-like eruption [6]. Post-orf autoimmune bullous dermatoses are much rarer, with only eleven cases reported in the literature [2]. The first cases of bullous pemphigoid secondary to an orf nodule were described in 1995 by Murphy et al., who reported five cases occurring after two-to-three weeks [7]. In our case, the bullous lesions appeared around three weeks after the appearance of the orf nodule, which was consistent with the literature (2–4 weeks) [2,7].
Avci et al. also reported the relationship between orf infection and bullous pemphigoid [8].
The clinical, histopathological, immunofluorescence results, as well as the improvement under topical steroids and the absence of a relapse, confirmed the diagnosis of orf-induced bullous pemphigoid.
The relationship between orf and bullous pemphigoid has not yet been fully elucidated [9].
The pathophysiological mechanism of autoimmune diseases secondary to an orf may include viral mimicry of host proteins or the destruction of basement membrane proteins by the virus.
The physiopathological mechanism of autoimmunity induced by orf virus is poorly understood, hence the interest in reporting other cases of this complication.
Further case reports regarding this clinical condition are needed.
The patient was treated with a topical steroid giving a complete improvement.
In cases described in the literature, their patients were also treated by topical steroids, yet some patients received prednisone, azathioprine, dapsone, colchicine, or cyclosporine.
CONCLUSION
Herein, we have reported a case of bullous pemphigoid secondary to an orf nodule, which is a highly rare complication. The relationship between the two diseases has not been elucidated completely. Further case reports regarding this clinical condition are needed.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Johannessen JV, Krogh HK, Solberg I et al. Human orf. J Cutan Pathol. 1975;2:265-83.
2. Zuelgaray E, Salle de Chou C, Gottlieb J, Battistella M, Vignon-Pennamen MD, Bagot M, et al. Human orf complicated by epidermolysis bullosa acquisita. Br J Dermatol. 2018;178:547-50.
3. Slattery WR, Juckett M, Agger WA, Radi CA, Mitchell T, Striker R. Milkers’nodules complicated by erythema multiforme and graft-versus-host disease after allogeneic hematopoietic stem cell transplantation for multiple myeloma. Clin Inf Dis. 2005;40:63-6.
4. Ozturk P, Sayar H, Karakas T, Akman Y. Erythema multiforme as a result of Orf disease. Acta Dermatovenerol Alp Pannonica Adriat. 2012;21:45-6.
5. Shahmoradi Z, Abtahi-Naeini B, Pourazizi M, Meidani M. Orf disease following 'eid ul-adha’:A rare cause of erythema multiforme. Int J Prev Med. 2014;5:912-4.
6. Alian S, Ahangarkani F, Arabsheybani S. A Case of orf disease complicated with erythema multiforme and bullous pemphigoid-like eruptions. Case Rep Infect Dis. 2015;2015:105484.
7. Murphy JK, Ralfs IG. Bullous pemphigoid complicating human orf. Br J Dermatol. 1996;134:929-30.
8. Avci A, Avci D, Turasan A, Çınar SL. [A case of bullous pemphigoid as a complication of human orf]. Turk J Dermatol. 2013;7:91-2.
9. Ogretmen Z, Gül C, Ekinci A, Akalın T. Bullous pemphigoid complicating human orf disease. J Pak Assoc Dermatol. 2018;28:375-7.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0009-0006-6042-0236 http://orcid.org/0009-0006-6042-0236 http://orcid.org/0009-0005-7920-3082 http://orcid.org/0009-0005-7920-3082 http://orcid.org/0000-0002-2927-4983 http://orcid.org/0000-0002-2927-4983 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0003-1885-6563 http://orcid.org/0000-0003-0231-1665 http://orcid.org/0000-0003-0231-1665 http://orcid.org/0000-0002-5204-0528 http://orcid.org/0000-0002-5204-0528 |





Comments are closed.