Hypertrophic lichen planus of the soles: A rare variant in a rare location
Chaymae Jroundi 1, Sara Elloudi1, Jihad Kassel1, Zakia Douhi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1, Sara Elloudi1, Jihad Kassel1, Zakia Douhi1, Hanane Baybay1, Fatima Zahra Mernissi1, Mouna Rimani2
1Department of Dermatology, University Hospital Hassan II, Fes, Morocco, 2Hassan Center of Pathology, Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Lichen planus (LP) is a chronic inflammatory and immune-mediated condition of unknown etiology that affects the skin, hair, and nails. It usually occurs in females and is most often characterized by pruritic, purple, plane papules located on the flexural extremities [1]. Numerous variants of LP have been described, including actinic, annular, atrophic, eruptive, follicular, hypertrophic, inverse, linear, palmoplantar, pemphigoids, pigmentosus, ulcerative, vesiculobullous, and vulvovaginal [1,2]. Palmoplantar LP is a rare variant presumed to be more common in males and is usually associated with oral Wickham striae and skin lesions in regions other than the palms and soles. The clinical presentation in this particular location may vary from hypertrophic plaques to erosive, erythematous patches and may be considered a diagnostic challenge [1]. Hypertrophic lichen planus (HLP) is characterized by hyperkeratotic, itchy papules and plaques, involving commonly the extremities, especially the anterior legs, and also the upper extremities and trunk [3]. Dermoscopy may be a useful, non-invasive tool that aids in the diagnosis of LP. Dermoscopic features of classic LP have been widely described. Recently, more reports of LP variants have found some dermoscopic structures to be more specific of hypertrophic LP than others, such as comedo-like openings, also known as corn pearls, peripheral striations, bluish-gray/brown globules, and a globular pattern of Wickham striae [4,5]. On dermoscopy, corn pearls may increase in number and size and conglomerate forming a “bouquet of white roses,” which reflects the degree of hyperkeratosis [6]. Diagnosis is usually clinical, with the typical presentation of classic LP. However, a skin biopsy might be required to confirm the diagnosis in atypical presentations [4]. The histopathological features of palmoplantar LP are similar to those of classical LP, including hyperkeratosis with parakeratosis, a focal increase in the granular cell layer, vacuolar degeneration of the basal cell layer, and a band-like lymphocytic infiltrate at the dermal–epidermal junction [2]. Due to the varied presentation and a large number of similar appearing conditions, recognition is often delayed, which makes it essential to keep this entity in mind [4,7]. Herein, we report three cases of hypertrophic lichen planus of the soles with no other skin involvement in two females and one male.
CASE 1
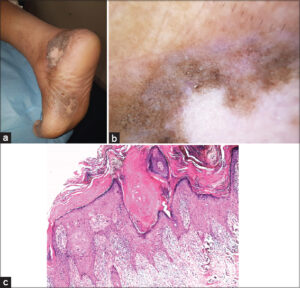
A sixty-year-old female patient, with a history of diabetes, presented with pruritic lesions on the soles of both feet evolving for four years, for which she had applied topical antifungals without improvement. A clinical examination found three hyperkeratotic, pigmented plaques with achromic centers, well-limited and oval in shape, located on the internal plantar arch of both feet and on the ankle, without any other skin lesions (Fig. 1a). Dermoscopy revealed comedo-like openings, Wickham striae with a globular pattern, a reticulated and globular pigmented pattern, whitish areas without structures, and pointed vessels (Fig. 1b). Anatomopathological analysis of a skin biopsy showed hyperacanthosis, marked hyperkeratosis, and a thickened granular layer with hypertrophic epidermal ridges in a sawtooth pattern, sometimes in the form of clubs, associated with a lichenoid interface dermatitis, concluding to a hypertrophic lichen (Fig. 1c). The patient was treated with high-potency topical steroids.
CASE 2
In a 54-year-old female patient, with a history of lichen planus confirmed on a skin biopsy five years prior, the lesions were initially located on the thighs and arms with no palmoplantar involvement and were treated with topical steroids with complete regression of all lesions. The patient presented three years later with slightly pruritic lesions on the soles evolving for over two years. On examination, hyperkeratotic pigmented plaques with fissurations were found on the inner arches of the soles of both feet extending to the back of the foot (Fig.2a). Dermoscopy showed comedo-like openings, whitish scales, pointed vessels, fissuring, homogeneous pigmentation, in favor of a plantar hypertrophic lichen (Fig. 2b). The rest of the skin examination was normal. This patient was also treated with high-potency topical steroids with good improvement.
CASE 3
A 54-year-old male patient, without a previous history, had pruritic lesions on the palmoplantar area for four years as well as pigmented lesions on the face and trunk. A dermatological examination revealed an erosive palmoplantar keratoderma with fissurations (Fig. 3) and well-limited, macular, pigmented patches on the face and trunk. The patient underwent two skin biopsies in favor of a lichen pigmentosus of the face and a lichen planus of the feet. A treatment based on topical steroids initially, then oral corticosteroids at a dose of 0.5 mg/kg/day was administered along with localized UVB therapy with partial improvement.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Riahi RR, Cohen PR. Hypertrophic lichen planus mimicking verrucous lupus erythematosus. Cureus. 2018;10:e3555.
2. Koh YP, Su P. An unusual case of pigmented plaques on the sole. Dermatol Online J. 2020;26:13030/qt5q9169rw.
3. Korbi M, Rouatbi J, Njima M, Belhadjali H, Youssef M, Zili J. Hypertrophic lichen planus on the face. Our Dermatol Online. 2020;11:e112.1-2.
4. Mirchandani S, Ballal DS, Rodrigues G, Pai K. Generalized hypertrophic lichen planus:An atypical presentation of a characteristic disease. Med Pharm Rep. 2020;93:210-12.
5. Hanumaiah B, Joseph JM. Role of dermoscopy in the diagnosis of hypertrophic lichen planus and prurigo nodularis. Indian J Dermatol. 2019;64:341-5.
6. Malakar S, Mehta P, Save S, Malakar SS. “Bouquet of white roses“:A dermoscopic marker for hypertrophic lichen planus. Our Dermatol Online. 2021;12:96-8.
7. Abreu Velez AM, Howard MS, Pereyo N. Palmar and plantar lichen planus:A case report and review of the literature. An Bras Dermatol. 2015;90(3 Suppl 1):175-7.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 |






Comments are closed.