Comorbidities as prognostic factors in the healing of venous ulcers
Mirela Vasileva , Vesna Brishkoska Boshkovski, Elena Drakalska Sersemova
, Vesna Brishkoska Boshkovski, Elena Drakalska Sersemova
Dermatovenerology Department, University “Goce Delcev” Shtip, Faculty of Medical Science, Shtip, North Macedonia
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: The problem of venous ulcers and chronic venous insufficiency is quite common in dermatological clinics. Every day, we face challenges regarding treatment and prognosis. As the patients are more often over fifty years of age, with more comorbidities, and at the very beginning of treatment, we already have an idea of how the entire process of epithelization of the ulcers may take place.
Materials and Methods: A total of 105 patients with chronic venous insufficiency and venous ulcers were included in the study. Each was followed for more than twelve weeks. Patients with hypertension, diabetes mellitus, and thrombophlebitis were analyzed separately.
Results: Patients with an ulcer closure time of twelve weeks and longer had a high blood pressure more often. Diabetics with venous ulcers on the lower extremities more often had delayed ulcer healing. A statistically significant difference was confirmed in the distribution of the patients with and without thrombophlebitis.
Conclusion: The existence of comorbidities, such as hypertension, diabetes mellitus, and thrombosis, may affect the healing process of venous ulcers, yet thrombosis proved to be the most important factor.
Key words: Venous Ulcers; Diabetes Mellitus; Thrombosis; Hypertension
INTRODUCTION
The problem of venous ulcers and chronic venous insufficiency is quite common in dermatological clinics. Every day, we face challenges regarding treatment and prognosis. To improve the therapeutic possibilities, we must always begin from the base, that is, the etiology and pathophysiology of the disease.
As the patients are more often over fifty years of age, with more comorbidities, and at the very beginning of treatment, we already have an idea of how the entire process of epithelization of the ulcers may take place. Most systemic diseases impact the process of vascularization, granulation, and finally epithelization of the ulcer tissue.
Peripheral arterial disease has already been proven to be an important factor in the delayed healing of ulcers, thus, in this research, we address diabetes mellitus, hypertension, and recurrent thrombosis as factors that may affect the healing of venous ulcers.
Patients with diabetes mellitus develop severe atherosclerosis of the small blood vessels in the legs and feet, leading to compromised vascular function. Because blood is unable to reach the wound, healing is delayed, eventually leading to necrosis and gangrene [1].
The pathophysiology of hypertension as a factor in the occurrence of delayed ulcer healing may be described as a narrowing of small blood vessels in the skin, which increases resistance to blood flow. The pathogenesis is associated with local factors triggering dermal arteriosclerosis and subsequent hyperplasia of the media layer and elastic lamina, a process known as hyalinosis [2,3]. Thrombosis is most often present in the past diseases of patients with venous ulcers. More than half of patients suffer from recurrent thrombosis of the great saphenous vein or its varicosities, while those with deep vein thrombosis occur somewhat less frequently.
The thrombotic process causes inflammation, scarring, and adhesion of the valves and luminal narrowing [4,5]. This leads to valvular incompetence and reflux, which further increase venous pressure and worsen chronic venous insufficiency [5,6].
MATERIALS AND METHODS
A total of 105 patients with chronic venous insufficiency and venous ulcers were included in the study. Each was followed for more than twelve weeks. The treatment was the same with the use of compression therapy, Diosmin, and debridement of the ulcer. The patients were divided into two groups: with normal ulcer closure up to twelve weeks and delayed ulcer closure longer than twelve weeks in terms of the comorbidities that they had. Patients with hypertension, diabetes mellitus, and thrombophlebitis were analyzed separately.
Performance methodology was with a clinical examination of the patient, taking a detailed history, and Doppler of the lower extremities.
The statistical significance of intergroup differences was tested with the chi-squared test.
RESULTS
Patients with an ulcer closure time of twelve weeks and longer had a high blood pressure (HTA) more often when compared to patients with a ulcer closure time below twelve weeks, yet without a statistical significance: 44 (73.3%) vs. 27 (60%), p = 0.15 (Table 1).
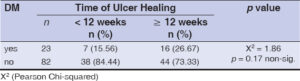
Diabetics with venous ulcers on the lower extremities more often had delayed ulcer healing, yet a statistical significance in the distribution of patients with and without diabetes, between groups with a ulcer closure time up to twelve weeks and twelve weeks or longer was not confirmed (p = 0.17); 16 (26.7%) patients with delayed ulcer healing and 7 (15.6%) with normal healing had diabetes mellitus (DM) (Table 2).
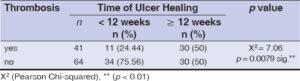
A statistically significant difference was confirmed in the distribution of patients with and without thrombophlebitis (TF), depending on the time of ulcer closure, analyzed as a time shorter than twelve weeks and twelve weeks or longer (p = 0.0079). Thrombophlebitis was diagnosed in 30 (50%) patients with delayed healing vs. 11 (24.4%) patients with normal healing of venous ulcers (Table 3).
DISCUSSION
Hypertension did not prove to be an important factor in the prognosis of venous ulcer treatment, although it was the most common comorbidity among our subjects, with a representation of 67.6% of the subjects.
Thrombophlebitis was also shown to be an important marker during the process of epithelization of lower limb wounds. In our study, 50% of the patients with delayed ulcer closure were diagnosed with thrombophlebitis. Only 11 patients diagnosed with thrombophlebitis were observed in the group of quick ulcer closure up to twelve weeks. The patients with a history of deep vein thrombosis had a lower chance of rapid ulcer healing and develop larger ulcers, all due to the damage that thrombosis leaves to the vessel walls.
However, the relationship between thrombophlebitis and the duration of the venous ulcer has quite poorly been described and insufficiently confirmed in the literature. In our study, the association of the presence of thrombophlebitis with the delayed healing of the venous ulcer was demonstrated.
The presence of diabetes mellitus did not prove to be an important prognostic factor in the delayed healing of venous ulcers. Among the patients with delayed healing of the venous ulcer, 15.6% were diagnosed with diabetes mellitus. Delayed wound healing in diabetics is thought to occur as a result of extracellular matrix deposits and the abundant cellular infiltrate present.
Diabetes is associated with endothelial dysfunction, thereby the more frequent occurrence of peripheral arterial occlusive disease and abnormal local cellular and cytokine activity, leading to defective and delayed wound closure.
In our study, out of the 23 patients diagnosed with DM, delayed healing was observed in 16; in 7 patients, there was a normal closure of the ulcer in a period of four to twelve weeks.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Vasilev B, Vasileva M, Vasileva S. The role of peripheral arterial occlusive disease in the healing of venous ulcers. Our Dermatol Online. 2022;13:280-2.
2. Malhi HK, Didan A, Ponosh S, Kumarasinghe SP. Painful leg ulceration in a poorly controlled hypertensive patient:A case report of Martorell ulcer. Case Rep Dermatol. 2017;9:95-102.
3. Shanshal M. Dermatologic Emergencies CME Part II:Infections and infection-related complications. Our Dermatol Online. 2022;13:483-94.
4. Pereira de Godoy JM, Pereira de Godoy LM, Pacheco EF, Guerreiro Godoy Mde F. The initial impact of low-level laser therapy on a traumatic leg ulcer. Our Dermatol Online. 2021;12:171-3.
5. Vasileva M, Brishkoska Boshkovski V, Petrov A, Zisovska E. Treatment of venous ulcers in drug addicts:A case report. Our Dermatol Online. 2021;12:439-41.
6. Raffetto JD, Ligi D, Maniscalco R, Khalil RA, Mannello F. Why venous leg ulcers have difficulty healing:Overview on pathophysiology, clinical consequences, and treatment. J Clin Med. 2020;10:29.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-6807-5557 http://orcid.org/0000-0002-6807-5557 http://orcid.org/0000-0002-1580-6117 http://orcid.org/0000-0002-1580-6117 |





Comments are closed.