Basosquamous cell carcinoma: A specific finding of a basaloid squamous cell transition
Shohei Igari1, Takako Miura1, Osamu Yamamoto2, Toshiyuki Yamamoto 1
1
1Department of Dermatology, Fukushima Medical University, Fukushima, Japan, 2Department of Dermatology, Tottori University, Tottori, Japan
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Basosquamous cell carcinoma is a relatively rare tumor with unique histopathological features of both basal and squamous cell carcinoma [1]. Herein, we report a case of basosquamous cell carcinoma on the face of an elderly male.
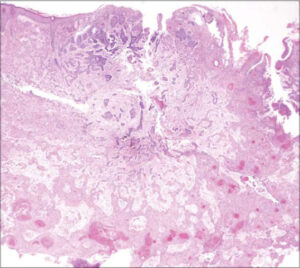
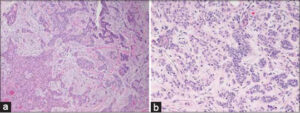
An 85-year-old male visited a local dermatology clinic complaining of a nodule on the face, which enlarged one month prior. He was a farmer and a never smoker, and his medical history included cerebral infarction, prostatic hypertrophy, and myocardial infarction. On physical examination, a relatively well-circumscribed, keratotic nodule measuring 15 × 12 mm in size was observed on the right cheek (Fig. 1). A biopsy specimen revealed a central basophilic area and an eosinophilic area surrounding the center of the dermis (Fig. 2). The peripheral eosinophilic area displayed anastomosing islands of atypical squamous cells with polygonal cytoplasm and intercellular bridges. The tumor cells had a keratinization tendency represented by cancer pearls. On the other hand, the central area exhibited smaller, solid or cord-like nests composed of basaloid cells, showing peripheral palisading and mucinous clefts between the nests and surrounding stroma. Both areas continued to the epidermis. In addition, some nests of both areas directly continued each other as transitional zones (Figs. 3a and 3b). Immunohistochemistry revealed the expression of AE1/AE3 (pancytokeratin) and CAM 5.2 (cytokeratin 8) in both areas, yet stronger in the squamous area (Fig. 4a), whereas the expression of BerEp4 was detected only in the basaloid cell areas (Fig. 4b). Epithelial membrane antigen was negatively stained. The patient was referred to our clinic for a surgical operation. Examination by computed tomography revealed lymph node metastasis. The remaining nodule was removed completely with a 6-mm margin, and covered with a full-thickness skin graft from the abdomen. Post-operative radiation therapy was not performed. Neither local recurrence nor lymph node metastasis was observed during a three-year follow-up period.
The definition of basosquamous cell carcinoma remains controversial. Some consider basosquamous cell carcinoma to be a variant of basal cell carcinoma (BCC), while others suggest a biological similarity to squamous cell carcinoma (SCC) with a metastatic potential [2]. In addition, the diagnosis of basosquamous cell carcinoma is often established when the collision of BCC and SCC is recognized in the same specimen, whereas other reports have defined basosquamous cell carcinoma only after the recognition of direct continuity between the areas of SCC and BCC [3]. It was highlighted that basosquamous cell carcinoma is neither a collision tumor nor a coincidental finding of adjacent BCC and SCC [1]; however, cases such as ours, exhibiting the direct transition between BCC and SCC, are extremely rare. Mitsuhashi et al. reported the concomitant occurrence of basosquamous cell carcinoma and spindle cell SCC. Their case also had a transitional zone between SCC and BCC, showing diminished BerEp4 staining in the former. In the present case, BerEp4 was detected only in the basaloid area. Furthermore, the expression fashion of cytokeratin was clearly different in the transitional zones. The mucinous stroma was prominent in the BCC areas. Recent studies have genetically defined basosquamous cell carcinoma and demonstrated that basosquamous cell carcinoma likely originates as BCC through the accumulation of ARID1A mutations and RAS/MAPK pathway activation, suggesting that basosquamous cell carcinoma resembles BCC more closely than SCC [4].
Basosquamous cell carcinoma has a significantly more frequent site of occurrence in sun-exposed areas. In a report collecting seventy-six cases of basosquamous cell carcinoma, the head and neck regions were the most common (76.3%), followed by the trunk (10.5%), lower limbs (7.9%), and upper arm (5.2%) [5]. A recent multi-center, prospective cohort study revealed that basosquamous cell carcinomas were localized on the head and neck in over 70% of cases, followed by the trunk (14.2%), arms (8%), and legs (7.3%) [6].
Basosquamous cell carcinoma is occasionally invasive and bears a high recurrence rate, suggesting its highly aggressive behavior [1]. Therefore, careful and long-term follow-up is necessary. The treatment of basosquamous cell carcinoma is performed according to SCC, and surgery with a wide and deep margin or Mohs surgery is the first-line option, with or without postoperative radiation therapy. A recent systematic review showed a high recurrence rate of basosquamous cell carcinoma after Mohs surgery and wide local excision [7]. Because the facial tumor was removed completely with a negative margin, additional therapies were not performed in the present case. Under the careful follow-up period, the patient has been free from either local recurrence or lymph node metastasis. In conclusion, our case was not a collision, yet a direct transition between BCC and SCC, and basosquamous cell carcinoma should be defined as such cases.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Shukla S, Khachemoune A. Reappraising basosquamous carcinoma:A summary of histologic features, diagnosis, and treatment. Arch Dermatol Res. 2020;312:605-9.
2. Garcia C, Poletti E, Crowson AN. Basosquamous carcinoma. J Am Acad Dermatol 2009;60:137-43.
3. Mitsuhashi T, Itoh T, Shimizu Y, Ban S, Ogawa F, Hirose T, et al. Squamous cell carcinoma of the skin:Dual differentiations to rare basosquamous and spindle cell variants. J Cutan Pathol. 2006;33:246-52.
4. Chiang A, Tan CZ, Kuonen F, Hodgkinson LM, Chiang F, Cho RI, et al. Genetic mutation underlying phenotypic plasticity in basosquamous carcinoma. J Invest Dermatol. 2019;139:2263-71.
5. Betti R, Crosti C, Ghiozzi S, Cerri A, Moneghini L, Menni S. Basosquamous cell carcinoma:A survey of 76 patients and a comparative analysis of basal cell carcinomas and squamous cell carcinomas. Eur J Dermatol. 2013;23:83-6.
6. Gualdi G, Soglia S, Fusano M, Monari P, Giuliani F, Porreca A, et al. Characterization of basosquamous cell carcinoma:A distinct type of keratinizing tumour. Acta Derm Venereol. 2021;101:adv00353.
7. Tan CZ, Rieger KE, Sarin KY. Basosquamous carcinoma:Controversy, advances, and future directions. Dermatol Surg. 2017;43:23-31.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-8390-2573 http://orcid.org/0000-0002-8390-2573 |






Comments are closed.