Pruritic papular eruption revealing HIV
Chaymae Jroundi 1, Hanane Baybay1, Hajar El Bennaye1, Imane Couissi1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Mouna Rimani2
1, Hanane Baybay1, Hajar El Bennaye1, Imane Couissi1, Zakia Douhi1, Sara Elloudi1, Fatima Zahra Mernissi1, Mouna Rimani2
1Department of Dermatology, University Hospital Hassan II, Fes, Morocco, 2Hassan Center of Pathology, Rabat, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2023. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Pruritic papular eruption (PPE) described in HIV is a skin disease often encountered in HIV-positive patients. It is most often a sign of severe immunodeficiency and is commonly reported in African, Southeast Asian, and Indian populations [1,2]. It affects both adult females and males and may also be seen in children. The elementary lesion is a discrete, firm, erythematous, urticarial, very itchy papule of the extremities, face, and trunk, sparing the palms and soles. Painful excoriations in the genital mucosa are sometimes described. The CD4+ lymphocyte count (CD4) is usually below 250 cells/mm3. Histopathology reveals a lymphohistiocytic, inflammatory, perivascular, and periannexal infiltrate with a variable number of eosinophils. According to the World Health Organization (WHO), it is recommended to all HIV patients with antiretroviral therapy (ART), regardless of the staging and the CD4 count [3]. However, an elective treatment for PPE has not yet been found. Regression has been noted in some cases after the initiation of antiretroviral therapy. UVB therapy seems to be the most successful method in cases not improving with antiretroviral therapy [4]. Herein, we report the case of a patient who presented with PPE revealing HIV.
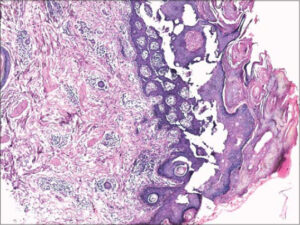
A 42-year-old patient presented with itchy, papular eruption persistent for over one year, worsening with topical steroids. A clinical examination revealed erythematous papules and urticarial plaques, some of which were purpuric and located on the trunk, limbs, and face (Fig. 1). Also, the presence of pustules on the nose, forehead, and arms, without palmoplantar involvement was noted. A mucosal examination showed hairy leukoplakia of the tongue (Fig. 2) and two erosions on the penis. The patient also had recurrent episodes of bronchitis and diarrhea. A blood examination was performed, which returned positive for HIV. A skin biopsy was performed showing marked hyperkeratosis with parakeratosis and keratotic, follicular plugs, also mild to moderate inflammatory infiltrates of the perivascular dermis, including eosinophils, lymphocytes, and histiocytes (Fig. 3), confirming the diagnosis of PPE related to HIV. A biological assessment showed a CD4 count of 234, and antiretroviral therapy was initiated.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Resneck JS, Van Beek M, Furmanski L, et al. Etiology of pruritic papular eruption with HIV infection in Uganda. JAMA. 2004;292:2614-21.
2. Ekpe O, Forae GD, Okpala CI. Pruritic papular eruption of HIV:A review article. Our Dermatol Online. 2019;10:191-6.
3. Rajput PS, Das AK, Paudel U, Parajuli S. Mucocutaneous disorders in HIV/AIDS at a tertiary care hospital in Nepal:An observational study. Our Dermatol Online. 2021;12:101-5.
4. Bellavista S, D’Antuono A, Infusino SD, Trimarco R, Patrizi A. Pruritic papular eruption in HIV:A case successfully treated with NB-UVB. Dermatol Ther. 2013;26:173-5.
Notes
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |






Comments are closed.