A clinicoepidemiological study on topical steroid misuse in a tertiary-care hospital in North India and the role of dermoscopy as a non-invasive diagnostic modality
Shagufta Rather , Saniya Akhtar, Insha Latief, Iffat Hassan
, Saniya Akhtar, Insha Latief, Iffat Hassan
Department of Dermatology, Venereology & Leprosy, Government Medical College, Srinagar, University of Kashmir, Jammu and Kashmir, India
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Topical corticosteroids (TCs) are one of the most frequently prescribed medications by dermatologists, yet may lead to an array of side effects due to prolonged and improper use. Because of the easy availability of topical corticosteroids as over-the-counter medications in India, these drugs are misused and abused.
Objective: The objective was to determine the extent and the side effect profile of topical corticosteroid misuse/abuse in patients attending the OPD, to determine the demographic data and the reason and source of procuring TCs, and to characterize the dermoscopic findings of TSDF.
Materials and Methods: This was a prospective, cross-sectional, clinical study conducted over a period of two years in which a predesigned, questionnaire-based proforma was employed. Patients above the age of fifteen reporting to the OPD giving a history of the application of a steroid cream continuously or intermittently for the minimum duration of four weeks were included in the study. A total of two hundred patients who met the clinical criteria were subjected to dermoscopic examination with a handheld dermoscope (DermLite DL4; 3Gen, U.S.; 10×).
Results: A total of 2400 patients (fifteen-year-old or older) were enrolled in the study, in which 65% of the patients were females while 35% were males. Mostly, the patients procured these medicines from the pharmacist or paramedic, followed by general practitioners. The most common indications for which topical preparations were used included acne, followed by photodermatoses and ephelides. Most of the patients used combination creams, followed by potent steroids such as clobetasol propionate and betamethasone valerate. The most common side effects were erythema (74%), followed by photosensitivity (49%), hypertrichosis (47%), telangiectasia (42%), acneiform eruption (33%), contact dermatitis (21%), wrinkles (23.50%), etc. The main findings noticed on dermoscopy were irregularly dilated, branching, tortuous vessels almost interconnecting with each other in 79.78%, followed by hypertrichosis in 56.34%, white structureless areas representing atrophy in 42.33%, red dots in 7.22%, and a reddish background in 92.20%.
Conclusion: The rampant use of TCs by patients for a prolonged period of time leads to a variety of side effects. Due to the topographical location, the climate of the valley, and the lighter skin type of the local population, the indications for which TCs were employed in our study group and the side effect profile were unique from the rest of the country. Dermoscopy may play a vital role in improving the diagnostic accuracy of TSDF and help us to differentiate it from close mimics.
Key words: Topical corticosteroids; Abuse/misuse; Side effect profile; Indications; Dermoscopy
INTRODUCTION
Topical corticosteroids (TCs) were introduced in dermatology in the 1950s. Owing to their potent anti-inflammatory and anti-proliferative effects [1], they became one of the most frequently prescribed medications by dermatologists. Soon after the advent of topical corticosteroids, their side effects began to surface. Prolonged and improper use of TCs may lead to an array of side effects, including skin atrophy, telangiectasias, striae, rosacea, acneiform eruption, ecchymosis, and steroid addiction [2–5].
Topical steroid damaged/dependent facies (TSDF) is a term denoting the phenomenon in which the misuse of and dependence on steroids applied to the face lead to a number of side effects such as erythema, telangiectasia, rosacea, atrophy, and acne. It is semipermanent or permanent damage to the skin of the face precipitated by the irrational, indiscriminate, unsupervised, or prolonged use of TCs, resulting in a plethora of cutaneous signs and symptoms and psychological dependence on the drug [6]. Similar side effects may be seen on any other part of the body as well when TCs are used over a prolonged period of time and may lead to atrophy, erythema, telangiectasias, and ecchymosis. Due to the easy availability of topical corticosteroids as over-the-counter medications in India, these drugs are misused and abused, which is responsible for the increasing number of patients presenting to the dermatology outpatient department (OPD) with signs and symptoms suggestive of steroid damage [7].
Objective
The objective was to determine the extent and the side effect profile of topical corticosteroid misuse and abuse in patients attending the OPD on any part of the body, to determine the demographic data, reason, and source of procuring TCs, and to characterize the dermoscopic findings of TSDF.
MATERIALS AND METHODS
This was a prospective, cross-sectional, questionnaire-based, clinical study conducted over a period of two years from May 2017 to May 2019. A predesigned, questionnaire-based proforma was employed for the study. Institutional ethical clearance was sought before undertaking the study. Patients above fifteen years of age reporting to the OPD giving a history of the application of a steroid cream continuously or intermittently to any part of the body for the minimum duration of four weeks were included in the study. The brand names of the preparations available on the market were requested. All patients younger than fifteen years, with PCOS, Cushing, or thyroid disorders, and those unwilling to answer the questionnaire were excluded from the study. Patients on systemic steroids, oral contraceptives, and hormone replacement therapy were also excluded from the study. Dermoscopic evaluation of the patients was performed in a later part of the study with a handheld dermoscope (DermLite DL4; 3Gen, U.S.; 10×) as the dermoscope was not available throughout the study period. Both polarized and non-polarized modes were used to study the characteristic features of TSDF. Images were recorded directly with the digital camera of the dermoscope with an attachment for a smartphone.
RESULTS
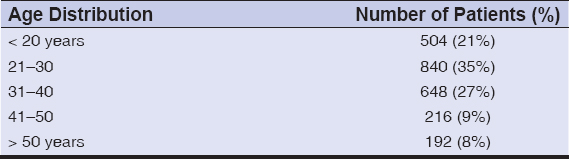
A total of 2400 patients (fifteen-year-old or older) were enrolled in the study and subjected to further questioning and examination. The majority of the patients were females (65%), as compared to males (35%). Most of the patients were in the 21-30 age group (35%) (Table 1). We noticed that the rural population consisted of 60% of the study group, while 40% were the urban population. The occupation-wise distribution included 28% of students, 26% of housewives, 24% of laborers, 12% of office workers, and 10% of businessmen and professionals. As for literacy level, 28% were undergraduate, 20% were graduate, 14% were postgraduate, and 38% were illiterate. Seventy-eight (78%) of the participants had heard about one or more of these topical preparations. Among them, 64% revealed the use of these preparations by a close family member or friend. None was aware of their side effects. Thirty-two (32%) were not ready to accept the fact that side effects were due to the use of TCs on the face and were not ready to stop their use despite our counseling. Most of the patients (83%) had been using TCs on the face, 9% had been using it on other parts of the body, and 8% had been using TCs on the face as well as on other parts of the body.
Most of the patients had procured these medicines from pharmacists or paramedics, followed by general practitioners and others (Table 2). Only in the case of 4%, these preparations were prescribed by the dermatologist. Twenty-seven percent of the patients had employed these preparations for acne, 19% for photodermatoses, 17% for ephelides, 14% for fungal infections, 12% for melasma, 7% for facial xerosis, and 4% for other indications (Table 3). The duration of application was not advised in 81% of the patients, yet 19% of the patients were advised not to prolong the use of these preparations without medical advice. In most cases, such information was given by the dermatologist.
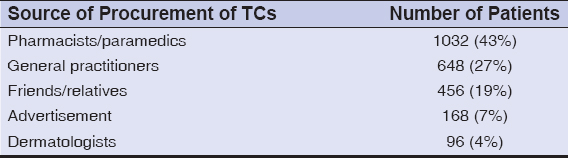 |
Table 2: Source of procurement of topical corticosteroids (TCs). |
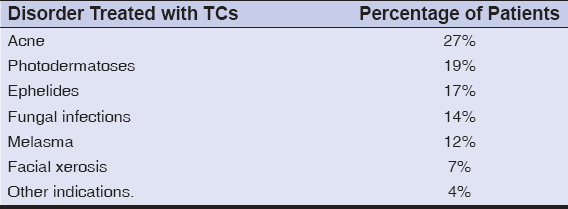 |
Table 3: Disorder for which the patient had been using topical corticosteroids. |
The frequency of application was once a day in 76% of the cases, twice a day in 19.4%, and more than twice a day in 4.6%. Sixty-eight percent of the patients applied topical steroids to the entire face while 32% to the affected areas only. The duration of use was one to three months in 29%, three to six months in 33%, six months to one year in 20%, and more than one year in 18%. On questioning about the effects of treatment, 83% of the patients believed to have a transient improvement, while 17% saw no improvement after the use of TCs. Among these 17%, the primary disorder for which the drug was used worsened in 6%, while it remained as it was in 11%. On the stoppage of the drug, there was worsening of the symptoms in 89% of the patients and no effect in 11%. Asked about the reasons for continued drug use, the patient stated reasons such as maintaining improvement (79%) and the avoidance of withdrawal side effects (16%), while the remaining 5% gave various other reasons.
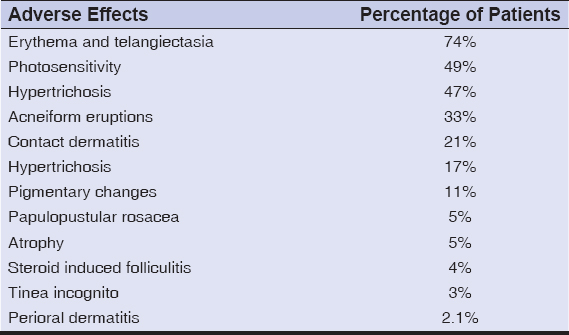
40.3% of the patients used clobetasol propionate while 29.4% used combination creams with clobetasol or gentamicin. 18.9% used betamethasone valerate, and 11% used mometasone cream, 1.3% used fluticasone cream. One side effect was seen in 15% of the patients and two side effects in 68%. Only 17% had three or more side effects. The most common side effect was erythema in 74% of the cases, followed by photosensitivity in 49%, hypertrichosis In 47%, telangiectasia in 42% (Figs. 1a and 1b), acneiform eruption in 33% (Figs. 1c and 1d), contact dermatitis in 21% (Fig. 2), pigmentary changes in 11% (Fig. 3a), papulopustular rosacea in 5% (Fig. 3b), atrophy in 5% (Fig. 3c), steroid-induced folliculitis in 4%, tinea incognito in 3%, and perioral dermatitis in 2.1% (Fig. 3d) (Table 4).
A total of two hundred patients were subjected to dermoscopic evaluation in our study. The main findings noticed on dermoscopy were irregularly dilated, branching, tortuous vessels almost interconnecting with each other in 79.78% of the cases, followed by hypertrichosis in 56.34%, structureless areas representing atrophy in 42.33%, red dots in 7.22%, and a reddish background in 92.20% (Figs. 4a – 4f). Other features observed were a fine, brown, reticular pattern on the background of a faint, light brown, structureless area in the cases of melasma (14%) and grayish-brown macules with interspersed, confetti-like, hypopigmented, macular areas in the cases those using combination creams for melasma, corresponding to exogenous ochronosis (3.5%).
DISCUSSION
TC misuse is a growing concern for dermatologists in India as it is slowly evolving into an epidemic-like condition. The rampant availability and use of TCs is alarming especially in a developing country such as India, as these medications are freely available on the market at very low prices. Also, for a significant number of patients, the first point of contact is the local pharmacist rather than the practicing doctor, selling these medications without proper prescription due to relaxed government guidelines [8]. Similar reports have been published in other countries [9–14].
In our study, the total number of patients enrolled over the period of two years was 2400. We found that a higher number of patients were misusing TCs in our study when compared to studies done in India by Mahar et al. [15] and Jha et al. [16], in which 256 and 410 patients misusing TCs were enrolled over a period of six months and one year, respectively. The majority of the patients in our study were females, with a male-to-female ratio of 1:1.8, which may be attributed to females being more concerned about dermatological issues. This finding is in accordance with other studies from India [15–17]. Also, a majority of the patients were from rural areas, with an urban-to-rural ratio of 1:1.5, which was possibly because of the lesser availability of practicing dermatologists in the rural areas of our country. These patients have easy access to local pharmacies in which TCs are easily available and sold by the shop owner without prescription [8]. Also, due to the low price of these medications, the underprivileged people of rural areas purchase them instantly without seeking further medical advice [7].
In our study, we noticed that the majority of the patients were illiterate. Also, there was a decrease in the number of patients misusing TCs with an increasing level of literacy. However, we even noticed patients with higher qualifications misusing TC. The patients in our study group were from different occupational groups, including housewives, students, laborers, office workers, businessmen, and professionals.
Most of the patients obtained the drug from the local pharmacist or paramedic. This trend is an indication of the level of malpractice in our society in which even the most potent TCs are easily available at very low prices on the market and are sold by the pharmacist without effort due to relaxed government guidelines. Similar findings have been observed in other studies from India as well [16,17]. Also, there is a need to increase awareness among general practitioners who prescribe TCs, especially in combination with antibiotics and antifungals for common skin diseases presenting to them, as 27% of our patients had received TCs from the general practitioner. Another factor responsible for this trend in our society is the dearth of dermatologists in rural areas in our valley where the first point of contact for the patient is a pharmacist, followed by a general practitioner. Advertisements regarding the use of TCs should to be banned completely in our country. Also, the dermatologist needs to counsel all patients being prescribed TCs for relevant indications that the prolonged use of TCs may damage the skin and these medications are not safe for use by other family members. A prescription from the dermatologist should include the duration of application of the TC, as incomplete information may promote the misuse of such medicines.
In our study, we found that most of the patients had been using TCs for acne vulgaris, followed by photodermatoses. Since Kashmir is situated at a high altitude, there is increased UV exposure in patients involved in outdoor agricultural activities. These patients use TCs to receive relief from common conditions such as polymorphic light eruptions and sunburns. However, as these patients use higher potency TCs such as clobetasol propionate and betamethasone valerate for prolonged periods of time, the benefits of TCs are masked by their side effects. Seventeen percent of the patients used TCs for ephelides as fair skin in the valley and increased UV exposure in the local population render people more prone to ephelides. Another condition that we noticed in our study for which TCs had been used was facial xerosis (7%). Due to cold weather conditions in the valley, people are more prone to dry skin, which is aggravated by frequent washing of the face and forearms for prayers by the majority Muslim population in the area. The indications for steroid misuse found in our study were different when compared to other studies from India and other countries. In studies by Sinha et al. [8], Rathi et al. [18], Sharma et al. [19], and Hammed AF [20], TCs were used most commonly as a fairness or cosmetic agent. In a study by Mahar et al. [5], TCs were used most frequently for dermatophytosis. However, we noticed that, in our population, the use of TCs as a fairness agent was not seen frequently, as the local population has fair skin and a lighter skin phototype (Type 3). Also, in none of the studies published so far have TCs been misused for photodermatoses and facial xerosis. These conditions are common in the Kashmiri population due to the high altitude, increased UV exposure, poor sun protection, minimal use of sunscreens, and dry weather conditions of the valley. Most of the patients had used TCs once a day, followed by twice a day. However, several patients applied it numerous times a day to the drying effect of the cold weather in which TC application was associated with the relief of the dryness.
The main symptom noted in our study group was erythema and telangiectasias in 74% of the patients, followed by photosensitivity in 49% and acneiform eruption in 33%. Our findings were different from a study done in India [15] in which tinea incognito was the most common side effect seen, followed by acneiform eruption. Other studies from India [16,19] have found acneiform eruption topping the list of side effects. We also noted acneiform eruption in quite a number of patients. However, due to the fairer complexion of the majority of the population in the valley, the most common side effect noted was erythema with telangiectasias, which was early to occur and most noticeable, followed by photosensitivity.
Dermoscopic evaluation was done in two hundred patients at the end of the study. The main dermoscopic features seen in our study were consistent with other studies, which included prominent telangiectasias, ivory-white-to-strawberry-colored patches, and lesional hypertrichosis [21]. The white structureless areas correspond to areas of dermal atrophy [22]. Also, features of melasma and exogenous ochronosis on dermoscopy were observed in 14% and 3.5% of the patients, respectively, who were using combination creams for melasma. These findings were consistent with the dermoscopic features seen in these patients as reported in other studies [23]. However, in a recent study done in India, dermoscopy of TSDF revealed brown globules (96.2%), followed by red, diffuse areas (92.4%), and vessels (87.1%) as the most common findings, which could represent the melasma for which the patient applied TCs [24].
CONCLUSION
Topical corticosteroids are a highly important class of drugs for the dermatologist. However, the rampant use of TCs by patients for a prolonged period of time leads to a variety of side effects. Due to the topographical location and climate of the valley, the indications for which TCs were used in our study group varied from other studies done in India. Also, due to the lighter skin type in our population, the side effect profile was also unique from the rest of the country. Thorough knowledge of the pattern of side effects with the need to increase awareness among practitioners and prevent the sale of TCs as over-the-counter medications will help to bring down the side effects associated with the misuse and abuse of TCs. Dermoscopy may play a vital role in improving the diagnostic accuracy of TSDF and help us to differentiate it from close mimics.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Smith EW. Do we need new and different glucocorticoids? A re-appraisal of the various congeners and potential alternatives. Curr Probl Dermatol. 1993;21:1-10.
2. Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54:1-15.
3. Rapaport MJ, Rapaport V. The red skin syndrome:Corticosteroid addiction and withdrawal. Expert Rev Dermatol. 2006;1:547-61.
4. Coondoo A, Phiske M, Verma S, Lahiri K. Side-effects of topical steroids:A long overdue revisit. Indian Dermatol Online J. 2014;5:416-25.
5. Abraham A, Roga G. Topical steroid-damaged skin. Indian J Dermatol. 2014;59:456-9.
6. Lahiri K, Coondoo A. Topical steroid damaged/dependent Face (TSDF):An entity of cutaneous pharmacodependence. Indian J Dermatol. 2016;61:265-72.
7. Coondoo A. Topical corticosteroid misuse:The Indian scenario. Indian J Dermatol. 2014;59:451-5.
8. Sinha A, Kar S, Yadav N, Madke B. Prevalence of topical steroid misuse among rural masses. Indian J Dermatol. 2016;61:119.
9. Lu H, Xiao T, Lu B, Dong D, Yu D, Wei H, et al. Facial corticosteroid addictive dermatitis in Guiyang City, China. Clin Exp Dermatol. 2010;35:618-21.
10. Liu ZH, Du XH. Quality of life in patients with facial steroid dermatitis before and after treatment. J EurAcad Dermatol Venereol. 2008;22:663-9.
11. Al Dhalimi MA, Aljawahiry N. Misuse of topical corticosteroids:A clinical study in an Iraqi hospital. East Mediterr Health J. 2006;12:847-52.
12. Mahe A, Ly F, Aymard G, Dangou JM. Skin diseases associated with the cosmetic use of bleaching products in women from Dakar, Senegal. Br J Dermatol. 2003;148:493-500.
13. Solomon BA, Glass AT, Rabbin PE. Tinea incognito and „over the counter”potent topical steroids. Cutis. 1996;58:295-6.
14. Rogers PJ, Wood SM, Garrett EL, Krykant SP, Haddington NJ, Hayhurst J, et al. Use of nonprescription topical steroids:Patients’experiences. Br J Dermatol. 2005;152:1193-8.
15. Mahar S, Mahajan K, Agarwal S, Kar HK, Bhattacharya SK. Topical corticosteroid misuse:the scenario in patients attending a tertiary care hospital in New Delhi. J Clin Diag Res. 2016;10:16-20.
16. Jha AK, Sinha R, Prasad S. Misuse of topical corticosteroids on the face:A cross-sectional study among dermatology outpatients. Indian Dermatol Online J. 2016;7:259-63.
17. Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face:A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
18. Rathi SK, Kumrah L. Topical corticosteroid-induced rosacea-like dermatitis:A clinical study of 110 cases. Indian J Dermatol Venereol Leprol. 2011;77:42-6.
19. Sharma R, Abrol S, Wani M. Misuse of topical corticosteroids on facial skin:A study of 200 patients. J Dermatol Case Rep. 2017;11:5-8.
20. Hameed AF. Steroid dermatitis resembling rosacea:A clinical evaluation of 75 patients. ISRN Dermatol. 2013;2013:491376.
21. Sonthalia S, Jha AK, Sharma R. The role of dermoscopy in a topical steroid-damaged face. Dermatol Pract Concept. 2018;8:2.
22. Jakhar D, Kaur I. Dermoscopy of topical steroid Damaged/Dependent face. Indian Dermatol Online J. 2018;9:286-7.
23. Khunger N, Kandhari R. Dermoscopic criteria for differentiating exogenous ochronosis from melasma. Indian J Dermatol Venereol Leprol. 2013;79:819-21.
24. Sethi S, Chauhan P, Jindal R, Bisht YS. Dermoscopy of topical steroid-dependent or damaged face:A cross-sectional study. Indian J Dermatol Venereol Leprol 2022;88:40-6.
Notes
Source of Support: Nil,
Conflict of Interest: The authors have no conflict of interest to declare.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-0980-6014 http://orcid.org/0000-0002-0980-6014 |







Comments are closed.