Laser and IPL hair depilation in pilonidal disease
Chaymae Jroundi , Hanane Baybay, Jihad Kassel, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
, Hanane Baybay, Jihad Kassel, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II of Fez, Morocco
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Pilonidal sinus disease (PNS) is a chronic inflammatory disease of the natal cleft occurring in young adults. We report our experience with laser hair removal using Nd: YAG laser and IPL for the treatment of pilonidal cysts.
Materials and Methods: Twelve patients presenting with pilonidal disease with or without a history of surgery were examined and treated from October 2016 to October 2021. All patients had modifiable risk factors. Treatments were performed with intense pulsed light (IPL) in nine patients and Nd: YAG laser at a wavelength of 1064 nm in five patients, and occasionally both were used in two patients. The number of treatments ranged from three to five, performed at four-to-eight-week intervals.
Results: Progressive hair depilation of the gluteal cleft was achieved in all patients. None of the patients have required further surgical treatments to date. No side effects were reported. All patients experienced a partial or complete remission of the pilonidal disease.
Conclusion: Laser hair depilation is a promising therapy in the prevention and management of pilonidal disease.
Key words: Pilonidal sinus; Laser depilation; Intense pulsed light; Nd: YAG
INTRODUCTION
Pilonidal sinus corresponds to a pseudo-cystic cavity containing hair, most often located in the natal cleft. It may manifest as pilonidal disease, in the form of acute infection (abscess), or chronic, persistent discharge of one or more sinuses [1]. There are two hypotheses regarding the etiopathogenesis of this entity: the congenital and the acquired theory [2]. The acquired theory, which is retained by most authors, states that, following repeated microtrauma, the broken free hairs penetrate and migrate under the skin, creating a fistulous pathway and behaving like foreign bodies, which triggers an inflammatory reaction with the resultant long-term, low-grade infection [2,3]. The risk factors include the male sex, a family history, obesity, and hirsutism [1]. Its benignity contrasts with the importance of its morbidity leading to an alteration in the quality of life with major socio-professional repercussions. The difficulty of its management is related to the high risk of recurrence, estimated to be 30% [2]. Although surgery is still considered the gold-standard treatment, it has a high recurrence rate and a prolonged healing time. Therefore, search is still ongoing for more optimal management alternatives [3].
PATIENTS AND METHODS
This was a retro-prospective study conducted between October 2014 and October 2021, including twelve patients presenting pilonidal disease with or without a history of surgery. Patients presenting with an acute pilonidal abscess were not excluded from the study; however, they received oral antibiotic therapy and were scheduled for laser treatment 2-3 weeks after the resolution of the inflammatory process. Nine patients were treated with an intense pulsed light (IPL) device (Nordlys by Ellipse) with HR 600 to 950 nm filters and the following parameters: 11-13.5 J/cm2, 40 ms. Five of our patients were treated with laser epilation with Nd: YAG laser (Fotona Dynamis XP) with a spot size of 9 mm and the following parameters: fluence 10-18 J/cm2, pulse duration of 1.6-3 ms. A dynamic cooling system was employed during the laser session. In two patients, the first treatment was performed with IPL before using Nd: YAG laser. With both procedures, hair was removed in a round area of 5 cm around the affected sinus. Treatments were performed at 4-to-8-week intervals for the first three to four treatments and then every 8-to-16 weeks until the remission of infection and the removal of most of the hair.
During each treatment session, the natal cleft was shaved with the application of a topical anesthetic agent (Figs. 1a and 1b). Laser depilation of the natal cleft with an appropriate wavelength not only for the patient’s skin type, yet also the degree of pigmentation of the area to be treated, was performed. The primary end point was assessed immediately with clinical and dermoscopic evaluations. In the cases with ulcerations or loss of substance, a preparation with hair and debris removal was performed (Figs. 1a and 1b). After the session, topical fusidic acid with a primary dressing made of saline-soaked compresses and a secondary absorbent dressing were applied. The patients’ pain tolerance and side effects were evaluated during the session and during the follow-up before every other session.
 |
Figure 1: Preparation phase: (a) the shaving area to be treated 5 cm from the midline and removing hair debris from the sinuses; (b) after a month with one session treatment with Nd: YAG laser. |
The study was conducted according to the principles of the Declaration of Helsinki and informed consent was obtained from all patients for the treatment and release of photographic images for scientific purposes.
RESULTS
Twelve patients (eight males and four females), aged 15 to 29 years (avg.: 22 yrs. +/- 7), came to our department with a history of pilonidal sinus disease in the natal cleft. Five of the patients underwent surgical treatment before admission. All patients had risk factors (Table 1). None had a family history of pilonidal sinus. Progressive hair depilation of the gluteal cleft was achieved in all patients. Pain tolerance was evaluated with the EVA scale with an average of 6/10. To date, none of the patients has experienced more acute abscesses or infections in the epilated area. All patients experienced a partial or complete remission of the pilonidal disease. Complete healing was achieved in 91% of the patients (only two patients have an active lesion with serosal discharge with ongoing treatment) (Figs. 2a and 2b). None of the patients has required further surgical treatment to date. No side effects were reported. Table 2 summarizes our results.
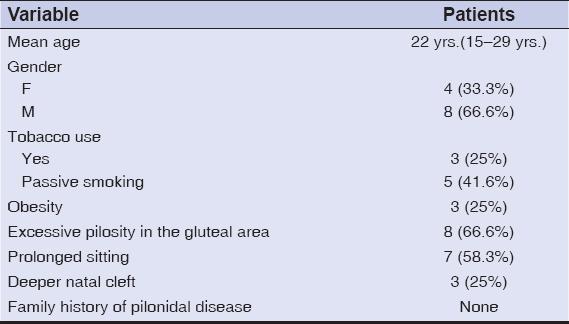 |
Table 1: Risk factors of pilonidal disease. |
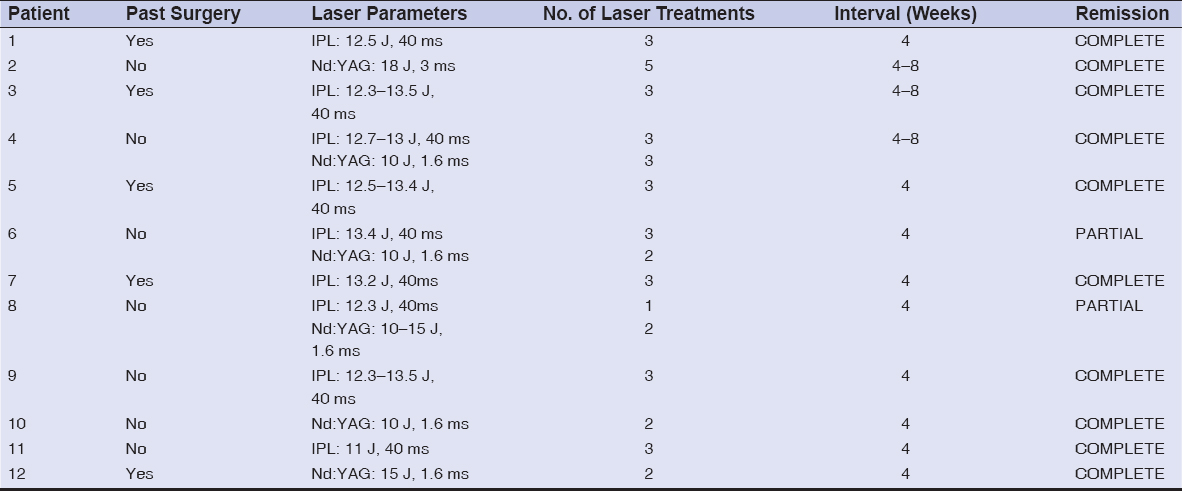 |
Table 2: Session parameters and results of laser epilation treatments in pilonidal disease. |
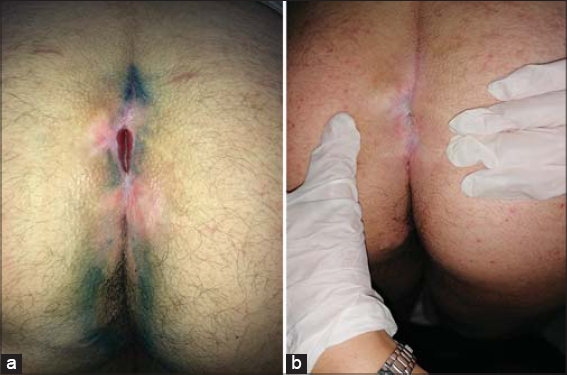 |
Figure 2: (a) After several unsuccessful treatment sessions of methylene blue and before hair removal; (b) complete remission after three IPL sessions. |
DISCUSSION
Pilonidal sinus disease (PNS) is a chronic inflammatory disease of the superior natal cleft that affects approx. 26 per 100,000 adolescents and young adults [4]. It is most common in males (at a ratio of 3-4: 1) and in Caucasians. It occurs most commonly in hirsute individuals [5]. The risk factors include obesity, hirsutism, poor hygiene, repeated microtrauma and friction, and a deep intergluteal cleft [2,6]. A case-controlled study on the risk factors of pilonidal sinus disease in preparatory school students conducted by Faraj et al. reported that sitting on hard surfaces for long periods of time should be considered a risk factor for developing PNS among secondary school students [7]. A prolonged sitting posture was indeed found in 58% of our patients due to their occupation (six students, one driver). The results of our study are consistent with those in the literature as at least one of these risk factors was reported by all of our patients (Table 1). Pilonidal disease may manifest itself in different forms depending on the degree of the inflammatory reaction. The asymptomatic form (3.2% of cases) presents as one or more non-inflammatory orifices located in the natal cleft 4-8 cm above the anal margin. The course of the disease may also start in the form of an acute abscess in 45% to 50% of cases, with painful swelling and, in some cases, a lateral extension and fever. The subcutaneous collection may be evacuated spontaneously through a secondary drainage orifice. The chronic form manifests itself by a continuous intermittent suppuration of the intergluteal fold that may or may not follow an abscess. Secondary and lateral orifices may communicate with one of the medial fossae with discharge of serositis or pus, which may persist [8]. The histopathological features are those of an epidermal lined dermoid cyst or a sinus tract. The cystic cavities are lined with granulation tissue with a mixed inflammatory infiltrate, hair, and keratin debris [5]. The treatment may be divided into surgical and non-surgical techniques. Surgical treatment remains the first-line therapy for pilonidal cysts, yet it is associated with significant postoperative morbidity and a high recurrence rate, estimated at 30% [2,9,10], hence the importance of prevention by managing the modifiable risk factors, particularly excessive pilosity. Laser epilation is a highly effective method of reducing hair growth and various laser devices have been tested for the treatment of pilonidal cysts, especially postsurgical relapse. According to the Clinical Practice Guidelines for the Management of Pilonidal Disease of the American Society of Colon and Rectal Surgeons (ASCRS), laser epilation has a strong recommendation grade based on low-quality evidence [11]. It has been stated that, compared to surgical treatment of recurrences, laser depilation is an efficient and cost-effective method for preventing recurrence and reducing morbidity and loss of man-hours [12]. In a study conducted by Dragoni et al. which carried out an ultrasound evaluation at the beginning and end of treatment with Nd: YAG laser to further confirm treatment success, all patients experienced the disappearance of their pilonidal cysts. None of the patients presented recurrence of the disease during the follow-up [13]. Intense pulsed light (IPL) has also been successfully employed. A study done by Shafigh et al. including thirty patients noted a reduced recurrence rate estimated at 13.3% during a follow-up of 2.5 years on average, which shows that this hair removal technique still has its role as a safe, nearly painless alternative [14,15]. Our study supports what has been reported in the literature and illustrates that laser hair removal could potentially be a less invasive alternative to surgery in pilonidal disease by possibly avoiding the need for surgery and postoperative comorbidity. Laser hair removal could eventually play a role in preventing recurrences in patients requiring surgical management.
CONCLUSION
Despite its benign nature, pilonidal sinus disease is characterized by a high recurrence rate and a significant alteration in the quality of life of the patients. The role of excessive pilosity in the etiopathogenesis, yet also in the recurrence of PNS, is clearly established. Laser hair depilation is a promising therapy in the prevention and management of pilonidal disease.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975
REFERENCES
1. Pronk AA, Eppink L, Smakman N, Furnee EJB. The effect of hair removal after surgery for sacrococcygeal pilonidal sinus disease:A systematic review of the literature. Tech Coloproctol. 2018;22:7-14.
2. La Torre V. Le kyste pilonidal. Rev Francoph Cicatrisation. 2018;2:35 42.
3. Kelati A, Passeron T, Lacour JP, Bréaud J, Lagrange S. Intéret du laser épilatoire post-chirurgical dans la prévention des récidives de kyste pilonidal?: une étude cas-témoin monocentrique niçoise. Ann Dermatol Vénéréologie. 2017;144:S175.
4. Halleran DR, Onwuka AJ, Lawrence AE, Fischer BC, Deans KJ, Minneci PC. Laser hair depilation in the treatment of pilonidal disease:A systematic review. Surg Infect (Larchmt). 2018;19:566-72.
5. Bolognia JL, éditeur. Dermatology:ExpertConsult. 3rd edition ff. Edinburgh:Elsevier;2012.
6. Levinson T, Sela T, Chencinski S, Derazne E, Tzur D, Elad H, et al. Pilonidal sinus disease:A 10-year review reveals occupational risk factors and the superiority of the minimal surgery trephine technique. Mil Med. 2016;181389 94.
7. Faraj FH, Baba HO, Salih AM, kakamad FH. Risk factors of pilonidal sinus disease in preparatory school students:A case control study. Ann Med Surg. 2020;57:46 8.
8. De Parades V, Bouchard D, Janier M, Berger A. Pilonidal sinus disease. J Visc Surg. 2013;150:237-47.
9. Croke L. Pilonidal disease management:Guidelines from the ASCRS. Am Fam Physician. 2019;100:582-3.
10. Bi S, Sun K, Chen S, Gu J. Surgical procedures in the pilonidal sinus disease:A systematic review and network meta-analysis. Sci Rep. 2020;10:13720.
11. Johnson EK, Vogel JD, Cowan ML, Feingold DL, Steele SR;Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons’Clinical Practice Guidelines for the Management of Pilonidal Disease. Dis Colon Rectum. 2019;62:146-57.
12. Khan MAA, Javed AA, Govindan KS, Rafiq S, Thomas K, Baker L, et al. Control of hair growth using long-pulsed alexandrite laser is an efficient and cost effective therapy for patients suffering from recurrent pilonidal disease. Lasers Med Sci. 2016;31:857 62.
13. Dragoni F, Moretti S, Cannarozzo G, Campolmi P. Treatment of recurrent pilonidal cysts with nd-YAG laser:Report of our experience. J Dermatolog Treat. 2018;29:65-7.
14. Shafigh Y, Beheshti A, Charkhchian M, Rad FS. Successful treatment of pilonidal disease by intense pulsed light device. Adv Clin Exp Med. 2014;23:277-82.
15. Lopez JJ, Cooper JN, Fischer BA, Gonzalez DO, Deans KJ, Minneci PC. Safety and tolerability of laser hair depilation in pilonidal disease:A pilot study. Surg Infect (Larchmt). 2017;18:890-3.
Notes
Source of Support: Nil,
Conflict of Interest: The authors have no conflict of interest to declare.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0003-3455-3810 http://orcid.org/0000-0002-5942-441X http://orcid.org/0000-0002-5942-441X |



Comments are closed.