The epidemiology of cutaneous leishmaniasis in Al-Ramadi, Iraq
Abdullah Mancy 1, Khalid Mohammed Awad1, Thamer Abd-Al-Majeed2, Nusaibah Fakhree Jameel1
1, Khalid Mohammed Awad1, Thamer Abd-Al-Majeed2, Nusaibah Fakhree Jameel1
1Department of Dermatology and Venereology, Al-Ramadi Teaching Hospital, Al-Anbar Health Directorate, Ministry of Health, Iraq, 2Department of Dermatology and Venereology, Medical College, Al-Anbar University, Ministry of High Education, Iraq
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
ABSTRACT
Background: Cutaneous leishmaniasis is a disease caused by various species of the genus Leishmania via the bite of the different species of the vector infected female sandfly. It is an endemic disease in most Iraqi cities. This study was arranged to shed light on the epidemiological criteria of the disease in the city of Al-Ramadi.
Materials and Methods: A descriptive study on cutaneous leishmaniasis in the city of Al-Ramadi was conducted over a three-year period from 2019 to 2021. The diagnosis of the disease was dependent mainly on the clinical features of the infection. Detailed information was obtained from all patients, who were grouped according to their age. Sites, numbers, and any previous scars were recorded during the clinical examination.
Results: Five hundred and thirty-two patients affected by cutaneous leishmaniasis were examined in the dermatology clinic of Al-Ramadi Teaching Hospital in a period of three years from 2019 to 2021. The prevalence rate was 59/100,000. The highest number of patients affected during the year 2020 constituted around 39.5% of the cases. Mostly, infections appeared during the winter months (December, January, and February). Those younger than 2o years were mainly attacked by cutaneous leishmaniasis, constituting 63.3%. Males were more involved than females (57.5%). The hands, face, and feet were the most commonly involved sites, corresponding to around 20.57%, 20.11%, and 17.68% of the cases, respectively.
Conclusions: Cutaneous leishmaniasis is an endemic disease in Al-Ramadi, representing a public health problem for both the individuals and the community. For individuals, scarring of the face represents the main cosmetic and psychological trauma.
Key words: cutaneous leishmaniasis; Sandfly; vector; Old World; Scarring
INTRODUCTION
Cutaneous leishmaniasis (CL) is a protozoal disease resulting from infection with the protozoan of the genus Leishmania (L.) via the bite of the infected female sandfly [1]. The disease is distributed globally and geographically in the Old World and New World [2]. There are around twenty species of the genus Leishmania that attack humans: in the Old World, L. tropica, L. major, L. aethiopica, and L. donovani infuntum, and in the New World, L. brazelience complex and L. Mexicana complex [3]. There are different species of the sandfly, Phlebotomus species (P.) in the Old World and the Lutzomyia species in the New World [4].
CL is considered a zoonotic disease: the human is incidentally affected, and wild and domestic animals represent the primary reservoir host [5]. In some cases, the human plays the role of the primary reservoir host, as in the disease caused by the strains of L. tropica [6]. Another rare mode of transmission is venereal, vertical, and via infected blood and needles [7].
The life cycle of the Leishmania consists of two forms, the promastigote (the flagellated form that presents in the gut of the sandflies) and the amastigote in the vertebrate animals [8]. When the vector inoculates the parasites into the human body, the appearance of the disease depends on the species, the inoculum of the parasite, and the host’s immune status [3]. The clinical manifestations range from self-healing nodules to chronic and diffuse skin involvement with ugly, disfiguring scar formation [9].
In endemic regions, the diagnosis of CL is not difficult and mainly depends on the endemicity and clinical manifestations of the infection, in addition to tissue smear, histopathology, and culture [10–12].
In Iraq, two species of Leishmania are usually present: L. tropica, anthroponotic cutaneous leishmaniasis, and L. major, the zoonotic species [6,11]. Also, the number of sandflies is different according to the geographical region and time of the year (its peak being present during June and September) [13,14]. In Iraq, the most common species are P. papatasi and P. sergenti [15]. CL was reported in most Iraqi provinces, yet the epidemiological characteristics of the disease in the Al-Ramadi district remain poorly studied. Herein, we try to describe the epidemiological criteria of the disease in this locality.
MATERIALS AND METHODS
This was a descriptive study on CL conducted in the city of Al-Ramadi, the capital of the Al-Anbar province, which lies to the west of Iraq and has boundaries with three countries: Saudi Arabia, Syria, and Jorden. The city is divided by the Euphrates river into two parts, in addition to many-branched rivers that divide the city further, with agricultural farms distributed along both sides and the city and its surroundings with around 900,000 inhabitants. The study was performed from the beginning of January 2019 to the end of December 2021 in the dermatology outpatient clinic of Al-Ramadi Teaching Hospital. This hospital was the only present in the city, which was attended by patients affected by CL. The diagnosis of CL was depend on clinical features, in addition to the history of insect bites. In cases in which the diagnosis was uncertain, a tissue smear was taken from the suspected lesion for microscopical examination. If negative, the case was excluded from the study. The patients were inquired about their age, sex, time of infection, residence, occupation, previous infections, a family history, and any history of medical diseases and immunosuppressive drugs. The patients were grouped into three groups according to their age: group 1 (< 20 years), group 2 (21-40 years), and group 3 (> 41 years). On examination of the patients, the sites and number of lesions were determined and any scars from previous infections were noted. The study was performed after obtaining approval from the ethical committee. Written informed consent was taken from all patients.
Statistical Analysis
The differences among variables in the period of three years were assessed by the chi-squared test and the data was analyzed by SPSS. A p value below 0.05 was considered significant.
RESULTS
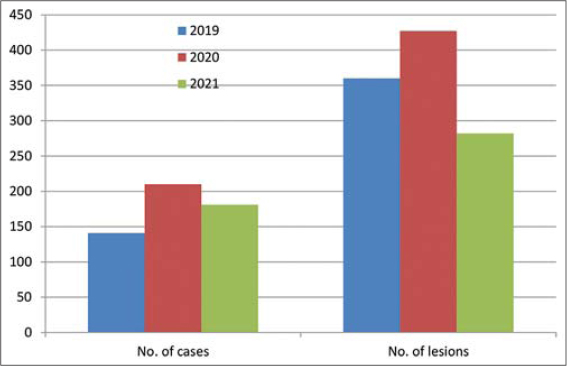
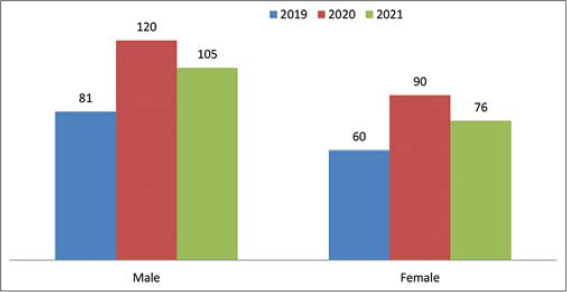
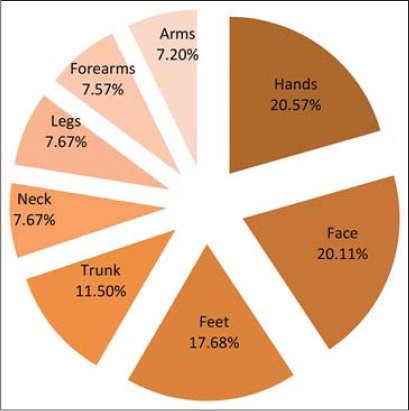
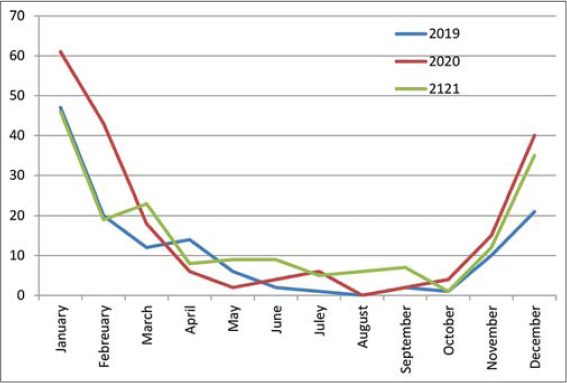
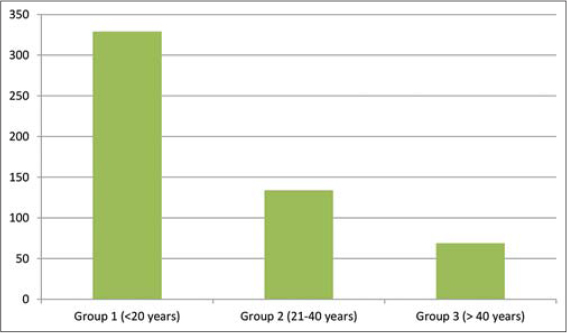
Five hundred and thirty-two patients and a total of 1069 skin lesions were seen in the dermatology clinic of Al-Ramadi Teaching Hospital over a three-year period from 2019 to 2021 (Table 1). The prevalence rate of the disease in Al-Ramadi was 59/100,000. The highest number of patients affected was in the year 2020 (39.5%), followed by 2021 (34%) and 2019 (26.5%) (Fig. 1). Also, most lesions of CL were seen during the year 2020, and the difference was significant (p < 0.01). Males were more commonly involved, constituting around 57.5% of the cases, while females comprised around 42.5% (Fig. 2). The exposed sites, the hands (20.57%), face (20.11%), and feet (17.68%), were the most often involved (p < 0.01) (Figs. 3 and 4). CL was most evident during the months of December, January, and February (winter season), constituting 63.3% of the cases, and was least so during June, Juley, and August (summer season), constituting 6.8% of the cases (Fig. 5). An early and young age were the primary culprits of the disease (Fig. 6), with ages ranging from two months to 85 years, those of an early age, less than twenty years old, were most affected (63.3%), followed by the age of 21-40 years, comprising 25.2% of the cases (p < 0.01). The presence of a previous scar of CL in association with novel lesions was reported in two cases (Fig. 7). A family history of the disease was present in 7.3% of the cases.
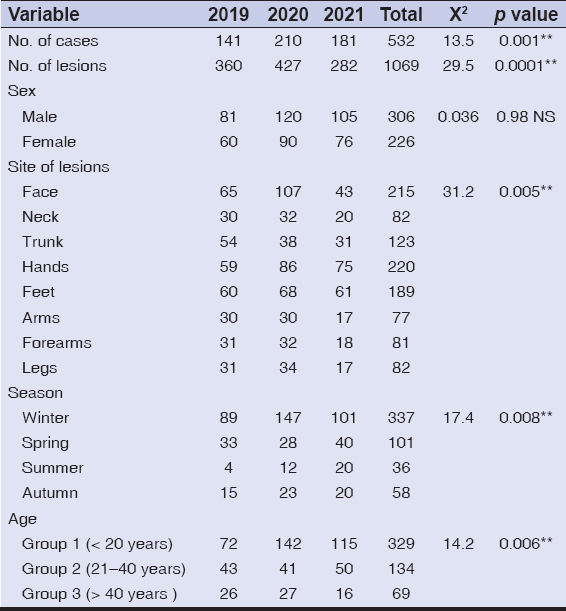 |
Table 1: Various parameters used to analyze the patients’ data from the three-year period of the study. **: (p≤0.01); NS: not significant. |
Leishmaniasis is recognized as one of the neglected tropical diseases [5,16]. It is endemic in around 98 countries, and around 0.7-1.2 million patients are affected yearly [17]. CL is endemic in Iraq, in addition to the high prevalence rate in the neighboring countries (Saudi Arabia, Iran, Turkey, and Syria) [12].
CL cases are widespread in most Iraqi provinces, and the first patients affected were reported in the cities of Mosul and Baghdad [18]. Previously, medical education and health care in Iraq were the most developed in the area [19]. In 2003, Iraq was exposed to an invasion with different aspects of terrorist attacks. These led to the destruction of the health system in the country. As a consequence, the frequency of communicable diseases in Iraq increased, CL being one of these [19,20].
The prevalence rate in Al-Ramadi was 59/100,000 of the population, and this is considered high. In comparison to other parts of Iraq, in the Al-Diwaniya province, three hundred cases were reported in 2008, in the Al-Rhamania province, four hundred cases were recorded in 2009, and 45/10,000 in the Al-Haweja district [11,21]. In the Rabeea district, Mosul province, 1482 cases of CL were recorded over a twelve-month period in addition to an outbreak of CL in the northern provinces of Iraq observed in 2003 [6,12]. This may be related to the military operations in the West and some regions in the North of Iraq that lead to the augmentation of people poverty, forced displacement of people, and migration from endemic to the non-endemic regions, reduction in health services that people need in association with poor sanitary states, the presence of agriculture farms and rivers throughout the city resulting in an increased density of the sandflies distribution and their reservoir. The highest number of patients and lesions of CL was seen in the year 2020. This variation of the disease from one year to another, because CL is unstable epidemiologically, sometimes presents with huge and unpredictable fluctuations in numerous cases [11,22]. Although the number of cases in 2019 was less than in 2021, there were more lesions in that year, which is explained by the development of multiple lesions in most patients.
In CL, all ages and both sexes may be affected, yet we discovered that children and adolescents are the most frequently affected. This was also seen in other studies [10] and by Al-Obaidi et al. and Klein et al. [23,24]. Younger individuals are more susceptible to being infected because they have not been exposed to bites of sandflies, thus they have not built an immune response against infections, in contrast to the elderly, who have been exposed to infections. Also, males were more often affected than females, which was also observed in other studies [23–25], yet another study found that females were more often affected [11]. In our locality, males are responsible mostly for outdoor work, thus are more prone to bites, especially performing farming and agricultural activities.
Cases of CL were recorded during cold weather, in the winter season, during December, January, and February, with the highest rate in January, then the rate decreasing slowly toward the hot season, with the lowest rate in August. Then, the rate of infections began to rise again toward the winter season. These results were also mentioned by Al-Warid et al. and Al-Samarai et al., yet the peak was in February [11,15]. In Iraq, the most suitable periods for breeding sandflies are April to November, and their peak falls in September and October [14]. This may be related to the presence of the vector and animal reservoir at this time of the year. Hence, the appearance of the disease depends on the incubation period of the parasite, which ranged from 1 to 4 months and may be extended from two weeks to one year [26]. Also, the exposed parts of the body were the most affected and this is logically acceptable as the insect usually attacks the exposed parts of the body at night for sucking blood. This is determined by individual habits such as sleeping outdoors in hot weather or wearing certain clothing for sleeping. The same results were observed by Khan et al., Oetken et al., and Aytekin et al. [27–29].
CONCLUSION
Cutaneous leishmaniasis is endemic in the city of Al-Ramadi. Disfiguring scars on the face, particularly, are the main drawback of the infection. Thus, the study of the epidemiology of this parasitic infection is essential for the prevention of such complications.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2008 revision of the Declaration of Helsinki of 1975.
Statement of Informed Consent
Informed consent for participation in this study was obtained from all patients.
REFERENCES
1. Sharquie KE, Hameed AF, Noaimi AA. Panniculitis is a common unrecognized histopathological feature of cutaneous leishmaniasis. Indian J Pathol Microbiol. 2016;59:16-9.
2. Masmoudi A, Hariz W, Marrekchi S, Amouri M, Turki H. Old World cutaneous leishmaniasis:Diagnosis and treatment. J Dermatol Case Rep. 2013;7:31-41.
3. Downing C, Tyring S. Parasitic disease. In:Barker J, Griffiths C, Bleiker T, Chalmers R, Creamer D. editors. Rook’s Textbook of Dermatology. 9th ed. Oxford:Wiley Blackwell;2010:1019-73.
4. Maroli M, Khoury C. Prevention and control of leishmaniasis vectors:Current approach. Parassitologia. 2004;46:211-5.
5. Stebut EV. Leishmaniasis and other protozoan infections. In:Sewon K, Masayuki A, Anna LB, Alexander HE, Devid JM, Amy JM, et al, editors. Fitzpatrick’s Dermatology. 9th ed. McGraw-Hill;2019:3257-397.
6. Salam N, Al-Shaqha WM, Azzi A. Leishmaniasis in the middle East:Incidence and epidemiology. PLoS Negl Trop Dis. 2014;8:e3208.
7. Reithinger R, Dujardin JC. Molecular diagnosis of leishmaniasis:Current status and future applications. J Clin Microbiol. 2007;45:21-5.
8. Stevending D. The history of leishmaniasis. Parasit Vectors. 2017;10:82.
9. Sharquie K, Noaimi A, Saleh B. cutaneous leishmaniasis as imitator of skin diseases and a diagnostic challenge. J Cosmet Dermatol Sci Appl. 2018;8:158-77.
10. James WD, Berger TG and Elastone DM. Parasitic infestations, stings, and bites. In:Andrews Diseases of the Skin:Clinical Dermatology.13th ed. Philadelphia. WB Saunders Company, 2020:491-526.
11. Al-Samarai AM, Al-Obaidi HS. Cutaneous leishmaniasis in Iraq, Infect Developing Countries. 2009;3:123-9.
12. Al-Bajalan MMM, Al-Jaf SMA, Niranji SS, Abdulkareem DR, Al-Kayali KK, Kato H. An outbreak of Leishmania major from an endemic to a non-endemic region posed a public health threat in Iraq from 2014-2017:Epidemiological, molecular and phylogenetic studies. PLoS Negl Trop Dis. 2018;12:e0006255.
13. Coleman RE, Burkett DA, Sherwood V, Caci J, Spradling S, Jennings BT, et al. Impact of phlebotomine sand flies on U.S. Military operations at Tallil Air Base, Iraq:2. Temporal and geographic distribution of sand flies. J Med Entomol. 2007;44:29-41.
14. Stoops CA, Heintshcel B, El-Hossary S, Kaldas RM, Obenauer PJ, Farooq M, et al. Sand fly surveillance and control on Camp Ramadi, Iraq, as part of a leishmaniasis control program. J. Vector Ecol. 2013;38:411-4.
15. Al-Warid HS, Al-Saqur IM, Al-Tuwaijari SB, AL Zadawi KM. The distribution of cutaneous leishmaniasis in Iraq:Demographic and climate aspects. Asian Biomed. 2017;11:255-60.
16. Elizabeth A, Ochola, S, Diana MS. The Impact of neglected tropical diseases (NTDs) on women’s health and wellbeing in Sub-Saharan Africa (SSA):A case study of Kenya. Int J Environ Res Public Health. 2021;18:2180.
17. Al-Jabi SW. Arab world’s growing contribution to global leishmaniasis research (1998-2017):A bibliometric study. BMC Public Health. 2019;19:625.
18. Al-Hayali H, Al-Kattan M. Overview on epidemiology of leishmaniasis in Iraq. Rafidian J Scien. 2021;30:28-37.
19. Al Hilfi TK, Lafta R, Burnham G. Health services in Iraq. Lancet. 2013;381:939-48.
20. Zhao Y, Riyadh L, Amy H, Abraham DF. The epidemiology of 32 selected communicable diseases in Iraq, 2004-2016. Int J Infect Dis. 2019;89:102-9.
21. Qasim BA, Nazar P, Al-Hadithi TS. An outbreak of cutaneous leishmaniasis in Erbil governorate of Iraqi Kurdistan Region in 2015. J Infect Dev Ctries. 2018;12:600-7.
22. Sharquie KE, Jabbar RI. Leishmania Recidivans could be induced by intralesional infiltration of cutaneous Leishmaniasis by Sodium Stibogluconate, with new therapeutic trial. J Clin Exp Invest. 2022;13:em00788.
23. Al-Obaidi M, Yaseen M, Al-Saqur IM. Survey study on the prevalence of cutaneous leishmaniasis in Iraq. Iraqi J Scien. 2016;57:2181-7.
24. Lockard RD, Wilson ME, Rodríguez NE. Sex-related differences in immune response and symptomatic manifestations to infection with Leishmania Species. J Immunol Res. 2019;2019:4103819.
25. Al-Sabawi B, Al-kallak S, Al-Niaeemi B. Cutaneous leishmaniasis and health awareness to prevent its spread in Nineveh Governorate, Iraq. Annals of R.S.C.B. 2021;25:10937-48.
26. El-Sayed M, Anwar AE. Intralesional sodium stibogluconate alone or its combination with either intramuscular sodium stibogluconate or oral ketoconazole in the treatment of localized cutaneous leishmaniasis:A comparative study. J Eur Acad Dermatol Venereol. 2010;24:335-40.
27. Khan SJ, Muneeb S. Cutaneous leishmaniasis in Pakistan. Dermatol Online J. 2005;11:4.
28. Oetken T, Hiscox B, Orengo I, Rosen T. Cutaneous leishmaniasis mimicking squamous cell carcinoma. Dermatol Online J. 2017;23:13030/qt8f36814f.
29. Aytekin S, Ertem M, Yagdiran O, Aytekin N. Clinico-epidemiologic study of cutaneous leishmaniasis in Diyarbakir Turkey. Dermatol Online J, 2006;12:14.
Notes
Source of Support: Nil,
Conflict of Interest: The authors have no conflict of interest to declare.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-3688-6953 http://orcid.org/0000-0002-3688-6953 |





Comments are closed.