Unilateral bullous pemphigoid in a hemiplegic patient
Siham Belmourida , Meriame Meziane, Nadia Ismaili, Laila Benzekri, Karima Senouci
, Meriame Meziane, Nadia Ismaili, Laila Benzekri, Karima Senouci
Department of Dermatology-Venereology, Mohammed V University, Ibn Sina Hospital, Rabat, Morocco
Corresponding author: Siham Belmourida
How to cite this article: Belmourida S, Meziane M, Ismaili N, Benzekri L, Senouci K. Unilateral bullous pemphigoid in a hemiplegic patient. Our Dermatol Online. 2022;13(2):229-230.
Submission: 06.11.2020; Acceptance: 14.02.2021
DOI: 10.7241/ourd.20222.32
Citation tools:
Copyright information
© Our Dermatology Online 2022. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Sir,
Bullous pemphigoid (BP) is the most common autoimmune bullous dermatosis, mainly affecting the elderly. Its association with neurological diseases has been reported for several years in several studies, including with strokes.
We report a new case of unilateral BP in a hemiplegic patient.
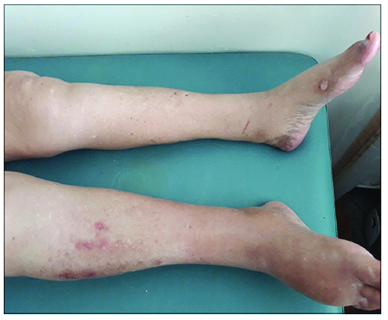
A 78-year-old patient with a history of hypertensive and ischemic heart disease and ischemic stroke three years ago was admitted for pruriginous bullous dermatosis evolving for one month prior to admission. A general examination revealed right hemiplegia with facial involvement and aphasia. A dermatological examination found localized erosions on the paralyzed side of the body, without urticarial or bullous lesions. Nikolsky’s sign was absent and the rest of the clinical examination was without abnormality (Figs. 1a – 1c). A skin biopsy revealed a skin coating widely ulcerated on the surface without eosinophilic infiltrate. Indirect immunofluorescence was positive at 1260. The diagnosis of BP was retained and the patient was started on a strong local dermocorticoid with a good evolution and the disappearance of the lesions after two months.
BP is an autoimmune bullous dermatosis clinically characterized by large, tense bubbles resting on erythematous skin and, histopathologically, by subepidermal bubbles with an eosinophilic infiltrate. Immunohistochemically, there are immunoglobulin (Ig) G and C3 deposits in the basal membrane of the epidermis. The initiating factor for the development of BP antibodies is not fully understood. Several studies have revealed the association of BP with neurological disorders such as stroke, dementia, Parkinson’s disease, multiple sclerosis, and epilepsy. The risk of association is greater if the neurological disorder is in a well-developed state [1–3]. However, the exact mechanism of this phenomenon remains an enigma. It might be explained by a decrease in blood in the paralyzed side with altered neurological functions associated with a defect in the contraction of the muscles or it might be an adverse effect from the drugs used for neurological diseases [4]. Further studies are needed to better support this causal link.
Keep in mind the diagnosis of BP in patients with chronic neurological diseases if faced with a bubble or erosive lesion.
Consent
The examination of the patient was conducted according to the principles of the Declaration of Helsinki.
The authors certify that they have obtained all appropriate patient consent forms, in which the patients gave their consent for images and other clinical information to be included in the journal. The patients understand that their names and initials will not be published and due effort will be made to conceal their identity, but that anonymity cannot be guaranteed.
REFERENCES
1. Chen YJ, Wu CY, Lin MW, Chen TJ, Liao KK, Chen YC, et al. Comorbidity profiles among patients with bullous pemphigoid:A nationwide population-based study. Br J Dermatol. 2011;165:593-9.
2. Langan SM, Groves RW, West J. The relationship between neurological disease and bullous pemphigoid:A population-based case-control study. J Invest Dermatol. 2011;131:631-6.
3. Tsuruta D, Nishikawa T, Yamagami J, Hashimoto T. Unilateral bullous pemphigoid without erythema and eosinophil infiltration in a hemiplegic patient. J Dermatol. 2012;39:787-9.
4. Moro F, Fania L, Sinagra JLM, Salemme A, Zenzo GD. Bullous pemphigoid:Trigger and predisposing factors. Biomolecules. 2020;10:1432.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
 http://orcid.org/0000-0002-2795-9161 http://orcid.org/0000-0002-2795-9161 |





Comments are closed.